Overview
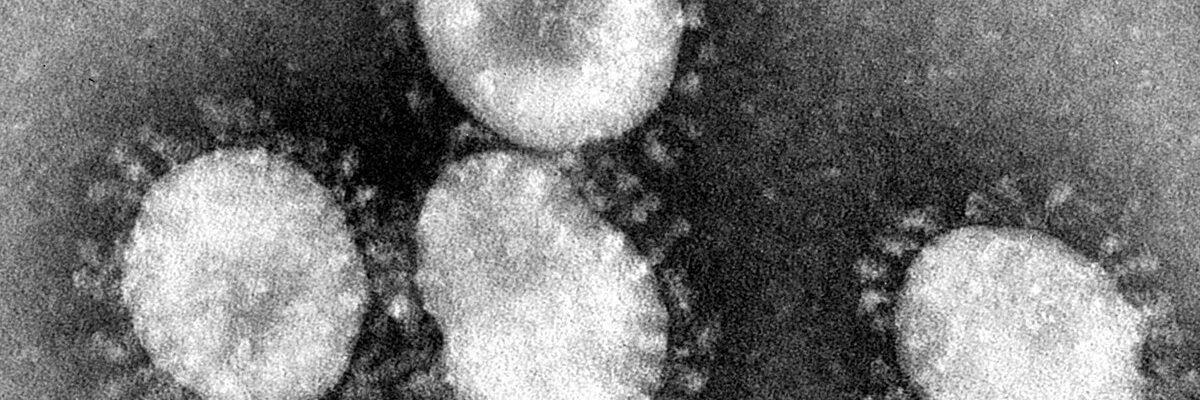
Severe Acute Respiratory Syndrome (SARS) is a contagious and sometimes fatal respiratory illness caused by the SARS coronavirus (SARS-CoV). First identified in 2002, SARS is characterized by symptoms such as high fever, cough, shortness of breath, and in severe cases, pneumonia, which can lead to respiratory failure. SARS is typically spread through respiratory droplets, close contact, and, in some cases, contact with contaminated surfaces. While there is no specific antiviral treatment for SARS, supportive care and interventions targeting symptom management and respiratory support are crucial for affected individuals.
Treatments for SARS focus on alleviating symptoms, preventing complications, and providing intensive care when needed. Supportive treatments, such as supplemental oxygen and mechanical ventilation, are often necessary for patients experiencing significant respiratory distress. In some cases, healthcare providers may use antiviral medications or corticosteroids to help control the virus and reduce inflammation in the lungs, though the effectiveness of these treatments varies and remains under study. Additionally, experimental therapies and investigational drugs were explored during SARS outbreaks to determine their potential in managing the illness, although none have been confirmed as definitive cures.
Patients diagnosed with SARS require isolation to prevent further transmission, with treatment in specialized healthcare settings to ensure both their safety and that of others. Early detection and rapid response are critical to managing SARS, as timely intervention can improve outcomes and minimize the spread of the virus. While the SARS outbreak has since been controlled, the treatments developed and knowledge gained continue to inform medical responses to other coronaviruses, including COVID-19.
Table of Contents
When to See a Doctor
If you suspect you may have symptoms of SARS, it’s important to seek medical attention promptly. SARS can progress rapidly, with symptoms worsening within a few days, leading to severe respiratory distress and, in some cases, life-threatening complications. Early medical intervention is critical to manage symptoms effectively and to prevent further spread of the virus.
You should see a doctor immediately if you experience high fever, persistent cough, shortness of breath, or other flu-like symptoms, especially if you have recently traveled to areas with known SARS outbreaks or have been in contact with someone diagnosed with the virus. These symptoms could be early signs of SARS or another serious respiratory illness, and delaying treatment may increase the risk of complications.
For patients with SARS symptoms, healthcare facilities typically provide specialized care and isolation to ensure the safety of both the patient and the broader community. Rapid diagnosis and supportive care can significantly improve outcomes, as doctors can administer treatments that help manage the illness and provide respiratory support if needed.
What Type of Doctor to Seek
If you suspect you have SARS symptoms, it’s crucial to consult a primary care physician, infectious disease specialist, or pulmonologist as soon as possible. A primary care doctor can perform an initial assessment and refer you to specialists if needed. An infectious disease specialist is particularly suited for handling viral infections like SARS and can coordinate care with a team of healthcare providers. For cases where respiratory symptoms are severe, a pulmonologist—who specializes in lung conditions—may provide essential support for managing breathing difficulties.
During outbreaks, healthcare facilities may designate specific centers or specialists to handle SARS cases. Reaching out to a designated SARS treatment center or hospital may ensure you receive focused care in an environment equipped to handle contagious diseases safely.
What to Expect From Your First Doctor Visit

During your first visit, the doctor will conduct a comprehensive assessment to diagnose the illness and determine its severity. This visit will likely involve several key steps:
- Medical History and Symptom Review. The doctor will ask about recent travel history, exposure to people with SARS, and the duration and nature of your symptoms, such as fever, cough, and breathing difficulties.
- Physical Examination. A thorough physical exam, especially of the respiratory system, will help the doctor assess how SARS is affecting your body. They will check for signs of respiratory distress, such as rapid breathing or reduced oxygen levels.
- Diagnostic Testing. Testing is essential for a definitive diagnosis of SARS. The doctor may order laboratory tests, such as a nasopharyngeal swab (to detect the virus in respiratory secretions) and blood tests to look for signs of infection and inflammation. Imaging tests like chest X-rays or CT scans may also be performed to check for pneumonia or other lung issues.
- Isolation and Preventative Measures. Because SARS is highly contagious, the doctor will follow strict isolation protocols to prevent further spread of the virus. If SARS is suspected, they may advise hospitalization in a specialized unit to monitor your symptoms and reduce exposure risks to others.
Following these initial evaluations, the doctor will discuss possible treatment options based on the severity of your symptoms. Prompt medical attention and isolation are key in SARS cases to help manage the illness and protect the health of those around you.
SARS Treatment Options

Since there is no specific antiviral cure for SARS, treatment focuses on supportive care, symptom management, and prevention of complications. The aim is to alleviate symptoms, maintain respiratory function, and prevent progression to more severe stages. Here are the primary treatment options for managing SARS:
- Supportive Care. Supportive care is essential for patients with SARS to help the body recover from the infection. This may include bed rest, hydration, and nutritional support. Additionally, fever reducers and pain relievers can help manage symptoms like high fever, muscle aches, and headaches.
- Oxygen Therapy. Patients with severe respiratory symptoms often require supplemental oxygen to improve blood oxygen levels. Oxygen therapy can range from a nasal cannula to more intensive support methods, such as a non-invasive ventilator, depending on the patient’s needs.
- Mechanical Ventilation. In cases of severe respiratory distress or respiratory failure, patients may need mechanical ventilation. This treatment provides oxygen directly into the lungs, supporting breathing when the body cannot maintain sufficient oxygen levels on its own. Ventilation is usually administered in an intensive care unit (ICU) where patients receive close monitoring.
- Antiviral and Antibacterial Medications. Although there is no definitive antiviral drug for SARS, certain antiviral medications, such as ribavirin, have been used experimentally. In cases where patients develop bacterial infections alongside SARS, antibiotics may be prescribed to treat these secondary infections. The effectiveness of antiviral treatment for SARS is still under study, and these medications are typically reserved for severe cases under close medical supervision.
- Corticosteroids. Corticosteroids may be administered to reduce lung inflammation in severe cases, as they can help alleviate some respiratory symptoms by dampening the immune response. However, the use of corticosteroids in SARS treatment is controversial, as they can have side effects and their effectiveness varies between patients.
- Experimental and Investigational Therapies. During past SARS outbreaks, doctors and researchers explored other investigational therapies, including immune-modulating drugs and convalescent plasma therapy, which uses antibodies from recovered patients. These treatments are typically considered on a case-by-case basis and are reserved for critically ill patients when standard supportive treatments are insufficient.
Treatment options for SARS are often tailored to each patient’s needs, and doctors may adjust the approach as symptoms progress. While supportive care is the cornerstone of SARS management, advances in research and emergency treatments developed during past outbreaks have helped improve understanding of coronaviruses. Close monitoring and timely intervention are key to managing SARS effectively and preventing severe complications.
SARS Prognosis
The prognosis for SARS (Severe Acute Respiratory Syndrome) varies depending on factors such as the patient’s age, underlying health conditions, and the timing of medical intervention. In general, patients with mild to moderate symptoms who receive early medical care and supportive treatment tend to recover fully. The majority of SARS cases resolve without long-term complications, especially in younger and otherwise healthy individuals. However, recovery may take weeks to months, as patients may experience lingering fatigue and respiratory issues even after the infection clears.
In more severe cases, SARS can lead to serious complications, including pneumonia, respiratory failure, and acute respiratory distress syndrome (ARDS). These complications are more likely to occur in older adults or individuals with pre-existing health conditions, such as heart disease, diabetes, or compromised immune systems. For these high-risk groups, SARS poses a higher mortality risk, and intensive medical care, such as mechanical ventilation, may be necessary.
Despite the potential for severe outcomes in certain cases, SARS treatment advancements and isolation measures have greatly improved the ability to manage the illness and contain its spread. While SARS outbreaks are rare, the knowledge and strategies developed during past outbreaks have significantly informed global healthcare responses to respiratory viruses. With timely medical intervention, most patients can achieve a positive outcome, and global health systems remain vigilant in monitoring and controlling any resurgence of SARS or similar coronaviruses.