Overview
Elephantiasis, also known as lymphatic filariasis, is a parasitic infection caused by thread-like worms known as filarial nematodes. These parasites are transmitted to humans through the bites of infected mosquitoes, primarily in tropical and subtropical regions. Once inside the body, the worms target the lymphatic system, causing blockages and disrupting the normal flow of lymph, a fluid that helps the immune system fight infections and remove waste.
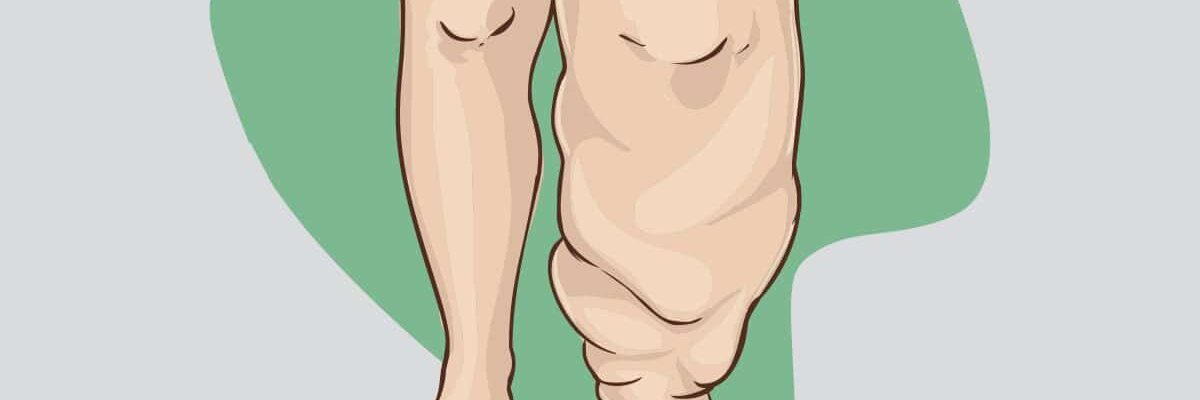
The most visible and distressing effect of elephantiasis is the severe swelling and thickening of the skin and tissues, particularly in the legs, arms, breasts, or genital area. This disfigurement is often accompanied by pain, reduced mobility, and social stigma, significantly impacting the quality of life of those affected. The condition can also lead to recurrent bacterial infections due to the impaired lymphatic system and poor skin health in swollen areas.
Treatment for elephantiasis involves a combination of antiparasitic medications to kill the worms, such as diethylcarbamazine (DEC) or ivermectin, and antibiotics to address secondary infections. In advanced cases, management focuses on reducing swelling through lymphatic drainage techniques, compression bandaging, and meticulous skincare to prevent further complications. In some situations, surgery may be necessary to address severe deformities or remove excess tissue.
Efforts to combat elephantiasis on a global scale include mass drug administration programs aimed at interrupting parasite transmission. Preventive measures, such as using mosquito nets, wearing protective clothing, and eliminating mosquito breeding sites, are critical in reducing the spread of this debilitating condition. Awareness and community-based initiatives also play an essential role in supporting affected individuals and promoting early diagnosis and treatment.
Table of Contents
When to See a Doctor
Seeking timely medical attention for elephantiasis is essential to prevent complications and manage the condition effectively. While early symptoms might be mild or easily overlooked, certain signs and situations warrant a consultation with a healthcare professional to ensure proper care and treatment.
Signs to see a doctor:
- Unexplained swelling or persistent swelling in the limbs, genitals, or other areas. If you notice swelling that does not resolve on its own or worsens over time, it may indicate an underlying issue with the lymphatic system and requires medical evaluation.
- Frequent infections in affected areas. Recurrent skin infections, redness, warmth, and tenderness in swollen regions are signs of impaired lymphatic function and may need antibiotic treatment and preventive measures to avoid further complications.
- Pain or discomfort affecting mobility or daily activities. Swelling associated with elephantiasis can become painful and interfere with normal functioning. Seeking medical help can lead to interventions that alleviate pain and improve quality of life.
- Signs of systemic infection, such as fever or chills. These may indicate that the condition has led to secondary bacterial infections, requiring urgent medical treatment.
- If you have been in areas where lymphatic filariasis is endemic and suspect exposure. Early treatment can prevent the progression of the disease, especially if you experience initial symptoms like mild swelling or lymphatic discomfort.
Prompt medical care not only helps in managing symptoms but also reduces the risk of permanent tissue damage and social stigma associated with advanced cases. Early intervention can ensure a better prognosis and minimize the long-term impact of the condition.
What Type of Doctor to Seek
When dealing with elephantiasis, it is important to seek the expertise of a healthcare professional familiar with lymphatic and infectious diseases. A primary care physician is often the first point of contact and can evaluate initial symptoms, provide basic care, and refer you to a specialist if necessary. In many cases, a tropical medicine specialist or an infectious disease specialist is the ideal choice, as they have the training and experience to diagnose and treat conditions caused by parasitic infections like lymphatic filariasis.
For managing advanced symptoms, such as significant swelling or complications like recurrent infections, consulting a lymphedema therapist or a vascular surgeon may be beneficial. These specialists focus on improving lymphatic function, reducing swelling, and addressing any structural deformities caused by the condition. Additionally, dermatologists can help manage skin-related issues in affected areas, ensuring comprehensive care. Choosing the right specialist often depends on the specific symptoms and complications you are experiencing.
What to Expect from Your Visit to a Doctor
During your visit to a doctor for elephantiasis, the initial steps typically involve a thorough medical history and physical examination. The doctor will ask about your symptoms, their duration, and any recent travel to regions where lymphatic filariasis is common. They may also inquire about mosquito bites or exposure to unsanitary conditions. A physical exam will focus on identifying swelling, skin changes, and signs of secondary infections in the affected areas.
To confirm the diagnosis and determine the cause, the doctor may recommend laboratory tests. These could include blood tests to detect the presence of microfilariae (larval parasites) or antibodies against the worms. In some cases, imaging tests such as ultrasounds or lymphoscintigraphy may be performed to assess lymphatic system damage. Based on the findings, the doctor will discuss a tailored treatment plan, which might include medications, skincare routines, or referrals to specialists for further management. This comprehensive approach ensures that all aspects of the condition are addressed effectively.
Elephantiasis Treatment Options

Image Source: www.freepik.com
Treating elephantiasis involves a combination of medication and supportive measures aimed at managing symptoms, eliminating the parasitic infection, and preventing complications. Depending on the stage and severity of the condition, doctors may recommend the following interventions:
- Antiparasitic drugs. Medications such as diethylcarbamazine (DEC), ivermectin (Mectizan), albendazole (Albenza), and doxycycline are essential for killing the adult worms and their eggs within the lymphatic system. These drugs help stop the progression of the disease and reduce the risk of further damage.
- Antihistamines. These medications alleviate itching and irritation in the affected areas, providing relief and preventing further damage to the skin caused by excessive scratching.
- Analgesics. Pain relievers help manage discomfort and pain caused by the swelling and inflammation of the affected limbs or other body parts, improving the patient’s quality of life.
- Antibiotics. If open wounds or skin lesions develop due to scratching or poor lymphatic drainage, antibiotics are prescribed to prevent or treat bacterial infections, which can exacerbate the condition.
Beyond medications, supportive care is crucial for managing elephantiasis and improving outcomes:
- Daily washing of affected areas. Washing the swollen and hardened skin with soap and water helps reduce itching and softens the skin, preventing infections and further damage.
- Application of moisturizing lotion. Regular use of moisturizers can alleviate dryness and itching, promoting healthier skin in swollen areas.
- Cleaning wounds regularly. Open wounds should be cleaned daily with antiseptics like povidone-iodine, especially after bathing and before bed, to prevent infections and promote healing.
For long-term management and to minimize swelling, additional measures may be necessary:
- Elevation of affected limbs. Keeping swollen limbs elevated helps improve lymphatic fluid flow and reduces swelling.
- Daily exercise. Gentle exercises strengthen muscles and encourage lymphatic drainage. Patients should consult their doctor to determine the most appropriate exercises based on their condition.
- Use of compression bandages. Wrapping the affected limbs with elastic bandages helps reduce swelling. Medical professionals can teach patients the correct way to apply these bandages.
While early and consistent treatment can restore the appearance and function of affected limbs, severe cases of elephantiasis may lead to permanent changes in tissue and limb size. For this reason, seeking medical care at the first sign of unusual swelling is critical to ensure the best possible outcome and prevent irreversible damage.
Elephantiasis Prognosis
The prognosis for elephantiasis depends significantly on early intervention and adherence to prescribed treatments. While the condition may not always be entirely reversible, appropriate treatment can halt its progression, manage symptoms, and improve quality of life. Below is an overview of what to expect from each treatment option:
- Antiparasitic drugs. When administered early, these medications can effectively eliminate the worms, preventing further lymphatic damage. However, they may not reverse existing swelling or tissue changes caused by prolonged infection.
- Antihistamines. These provide symptom relief, particularly for itching, which can minimize skin damage and reduce the likelihood of secondary infections. However, they do not address the underlying lymphatic dysfunction.
- Analgesics. Pain relievers improve daily comfort but do not impact the condition’s progression. They are most beneficial when used alongside other treatments that target the root cause.
- Antibiotics. Treating secondary infections can prevent severe complications and promote faster healing of wounds. Consistent use also helps maintain better skin health in affected areas.
- Supportive care (e.g., washing, moisturizing, elevation, exercise, and compression). These measures significantly reduce swelling, improve lymphatic drainage, and maintain skin integrity. While they cannot cure the condition, they are crucial for managing symptoms and preventing further complications.
With proper treatment and care, many individuals can regain functionality and reduce discomfort. However, advanced cases may result in permanent tissue changes, emphasizing the importance of early medical intervention and a commitment to ongoing care.