Overview
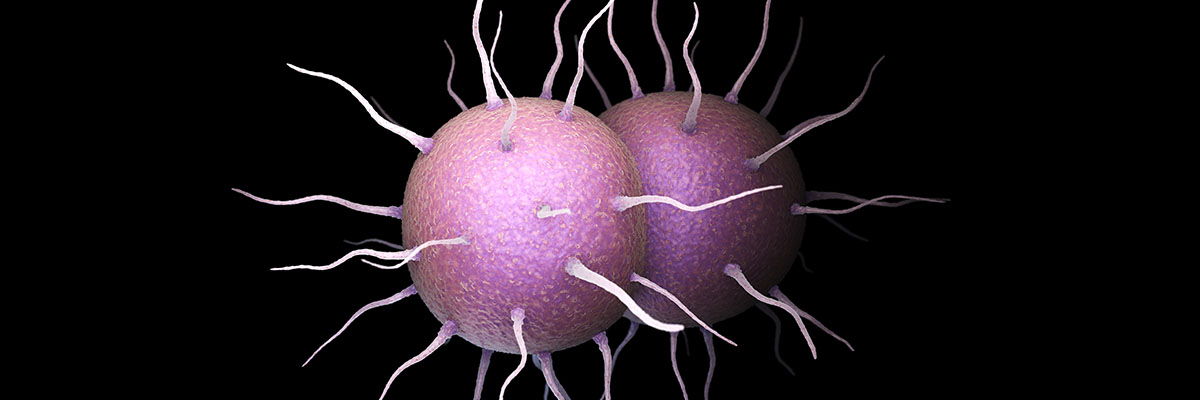
Gonorrhea is a common sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It spreads through sexual contact, including vaginal, anal, and oral intercourse, and can also be passed from mother to child during childbirth. The infection primarily affects the mucous membranes of the reproductive tract, but it can also infect the throat, rectum, and eyes. While often asymptomatic, particularly in women, untreated gonorrhea can lead to severe health complications.
The effects of gonorrhea vary depending on the site of infection. In women, it can lead to pelvic inflammatory disease (PID), causing chronic pelvic pain, ectopic pregnancies, and infertility. Men may experience painful urination, discharge, and in rare cases, epididymitis, which can also lead to infertility. If the bacteria enter the bloodstream, it can result in disseminated gonococcal infection (DGI), a potentially life-threatening condition characterized by fever, joint pain, and skin lesions.
Gonorrhea is treatable with antibiotics, but the emergence of antibiotic-resistant strains has made treatment increasingly challenging. The Centers for Disease Control and Prevention (CDC) currently recommends dual therapy with ceftriaxone and azithromycin for uncomplicated cases. However, drug-resistant strains necessitate careful monitoring and may require alternative regimens. Early diagnosis and prompt treatment are critical to prevent long-term complications.
Preventing gonorrhea involves practicing safe sex, including the consistent use of condoms and regular STI screenings for sexually active individuals. Education about STIs and open communication between sexual partners also play crucial roles in reducing its spread. With proper awareness, early detection, and appropriate medical care, gonorrhea can be effectively managed, reducing its impact on individual and public health.
Table of Contents
When to See a Doctor
Recognizing the need for timely medical attention is critical when dealing with gonorrhea, as early diagnosis and treatment can prevent serious complications. It’s important to consult a healthcare provider if you suspect you might have been exposed to gonorrhea or are experiencing symptoms of the infection.

Signs to see a doctor:
- You notice symptoms of gonorrhea. Common symptoms include unusual discharge from the genitals, painful or burning sensations during urination, and discomfort or pain in the pelvic area. Infections in other areas, such as the throat, rectum, or eyes, may cause soreness, rectal bleeding, or conjunctivitis-like symptoms.
- You have had unprotected sex or suspect exposure. If you or your partner has engaged in unprotected sexual activity, especially with multiple partners, it is wise to get tested for gonorrhea and other sexually transmitted infections, even if no symptoms are present.
- Your partner has been diagnosed with gonorrhea. If a current or recent sexual partner informs you of their diagnosis, seek medical advice immediately to get tested and treated, even if you are asymptomatic.
- You are pregnant or planning to become pregnant. Gonorrhea can be transmitted from mother to child during delivery, leading to severe complications for the baby, such as eye infections or even blindness. Pregnant women should undergo routine STI screening to ensure timely treatment.
- You experience complications or recurrent infections. Persistent symptoms after treatment or a recurring infection may indicate antibiotic resistance or an underlying condition, both of which require professional medical evaluation.
Seeking medical attention promptly ensures proper diagnosis, effective treatment, and prevention of further health complications. Additionally, it helps reduce the spread of gonorrhea within the community. Do not hesitate to consult a healthcare professional if you are concerned about your sexual health.
What Type of Doctor to Seek
If you suspect gonorrhea, your primary care physician, such as a family doctor or internist, can provide initial evaluation, testing, and treatment. They are often the first point of contact and can address general concerns while referring you to a specialist if necessary.
For more specialized care, women may consult a gynecologist for reproductive health concerns, while men can see a urologist for symptoms affecting the urinary or reproductive systems. If the infection is severe or involves complications like antibiotic resistance, an infectious disease specialist can provide advanced treatment and management. Seeking the right medical professional ensures proper care and prevention of complications.
What to Expect from Your Visit to a Doctor
When you visit a doctor for suspected gonorrhea, the appointment will typically begin with a discussion of your medical history and sexual activity. The doctor may ask about your symptoms, recent sexual partners, and any previous diagnoses of sexually transmitted infections (STIs). This information helps guide the evaluation and ensures accurate diagnosis and treatment.
The doctor will likely perform a physical examination and collect samples for testing. For genital infections, this may involve a urine test or swabs from the affected area, such as the cervix, urethra, throat, or rectum. Results from laboratory tests are usually available within a few days, and the doctor will discuss treatment options based on the findings. If gonorrhea is confirmed, antibiotics will be prescribed, and your doctor may recommend notifying recent sexual partners so they can be tested and treated as well.
Gonorrhea Treatment Options

Gonorrhea is treated with antibiotics, and several options are commonly prescribed depending on the patient’s needs and potential antibiotic resistance. These medications aim to eliminate the infection and prevent complications. Below is an overview of the most frequently used antibiotics for gonorrhea and their applications.
- Ceftriaxone. Ceftriaxone is a third-generation antibiotic effective against a wide range of bacteria. It is commonly used to treat gonorrhea and other infections such as pneumonia, ear infections, and meningitis. The Centers for Disease Control and Prevention (CDC) recommends administering ceftriaxone via injection in combination with azithromycin to ensure effective treatment and prevent resistance.
- Azithromycin. This antibiotic is widely used for treating sexually transmitted infections, including gonorrhea and chlamydia. Azithromycin can be taken orally as a tablet, capsule, or suspension, making it convenient for patients. It is also recognized by the World Health Organization (WHO) as one of the most essential medicines for human health due to its safety and effectiveness.
- Gemifloxacin. For individuals allergic to cephalosporins like ceftriaxone, gemifloxacin may be prescribed. It is a broad-spectrum antibiotic effective against various bacterial groups and is often paired with azithromycin for treating gonorrhea. It is also used for conditions such as bronchitis and mild pneumonia.
- Doxycycline. Doxycycline is another option for treating gonorrhea, particularly for mild cases. It is available in oral form or as an intravenous injection. This antibiotic is also used to treat other infections like syphilis, chlamydia, and leptospirosis. While not the first-line treatment, doxycycline is effective when tailored to the patient’s specific condition.
Treating gonorrhea effectively requires adherence to the prescribed antibiotic regimen. Failing to complete the course or self-medicating can lead to antibiotic resistance, making the infection harder to treat. Patients should also ensure their sexual partners are tested and treated to prevent reinfection.
Antibiotics for gonorrhea must be used responsibly to prevent the emergence of drug-resistant strains. In cases where resistance is suspected, stronger or combined antibiotics may be necessary. Always follow your doctor’s instructions carefully, and consult them if symptoms persist after treatment. This ensures a full recovery and helps limit the spread of the infection.
Treatment for Antibiotic-Resistant Gonorrhea
Antibiotic-resistant strains of gonorrhea pose a growing challenge in medicine, as these infections no longer respond to standard treatments. Stronger or combination antibiotics, such as ceftriaxone paired with azithromycin, are often required to combat these strains. Resistance arises from improper use of antibiotics, including self-medication, incorrect prescriptions, or failing to complete the full course of treatment, allowing bacteria to adapt and become immune to the medication.
To address this issue, healthcare providers emphasize strict adherence to prescribed regimens, ensuring the infection is completely treated. Public health efforts focus on patient education to discourage self-medication and promote responsible antibiotic use. Proper treatment and prevention strategies are essential to manage resistant gonorrhea and curb its spread, safeguarding both individual and public health.
Vaccine for Gonorrhea
Currently, there is no vaccine available to prevent gonorrhea, though researchers continue to explore this possibility. In the absence of a vaccine, education about gonorrhea is crucial in controlling its spread. The infection is primarily transmitted through sexual contact, but it can also be passed from an infected mother to her newborn during childbirth. While genital symptoms like pain and discharge are common, gonorrhea can also manifest in less obvious ways, such as joint pain, inflammation of the throat, or eye infections.

Preventing gonorrhea relies heavily on practicing safe sex, including consistent condom use and limiting the number of sexual partners. Open communication and honesty between partners are also essential. While gonorrhea is treatable with antibiotics, consulting a healthcare provider remains the best course of action for proper diagnosis and treatment. Natural or herbal remedies have not been scientifically proven to cure gonorrhea; they may only alleviate symptoms temporarily. To ensure complete recovery, always follow your doctor’s prescribed treatment plan diligently.
Gonorrhea Prognosis
The prognosis for gonorrhea depends largely on the type of treatment and the timeliness of medical intervention. With early diagnosis and proper adherence to prescribed therapies, the infection is typically treatable and curable. Below is an overview of the prognosis for various treatment options, including antibiotic-resistant gonorrhea and the potential for future vaccination.
- Standard Antibiotics (Ceftriaxone and Azithromycin). When treated with recommended antibiotics, gonorrhea is highly curable, and most patients recover without complications. However, adherence to the full course of treatment is essential to prevent recurrence or resistance.
- Alternative Antibiotics (Gemifloxacin and Doxycycline). In cases where standard treatments are unsuitable due to allergies or other factors, alternative antibiotics are effective for mild to moderate infections. Prognosis remains positive as long as treatment is timely and appropriate for the patient’s condition.
- Antibiotic-Resistant Gonorrhea. The prognosis for antibiotic-resistant strains depends on the availability of effective therapies. While dual or stronger antibiotic regimens can often manage these infections, delayed treatment may lead to complications such as infertility or systemic infections. Continued research is critical to addressing resistance challenges.
- Future Vaccination. While no vaccine currently exists, progress in research may offer hope for long-term prevention. Once developed, a vaccine would significantly improve the prognosis by reducing infection rates and limiting the spread of resistant strains.
Overall, gonorrhea is a manageable condition when addressed early and treated appropriately. Preventive measures, including safe sexual practices, regular screenings, and adherence to medical advice, are key to maintaining a positive prognosis for all forms of the infection.