Overview
Sarcoidosis is an inflammatory disease characterized by the formation of granulomas—small clusters of immune cells—in various organs, most commonly the lungs, lymph nodes, skin, and eyes. The exact cause of sarcoidosis remains unknown, but it is believed to involve an abnormal immune response. While sarcoidosis can resolve on its own without treatment, some cases require medical intervention, especially if the condition affects critical organs or causes severe symptoms.
The treatment approach for sarcoidosis depends on the severity and location of the disease. In mild cases, regular monitoring may be sufficient, as the condition may improve or disappear without intervention. However, for patients with more active disease, medications are used to control inflammation and prevent organ damage. Corticosteroids are often the first line of treatment, as they effectively reduce inflammation and granuloma formation. In cases where corticosteroids are not effective or cause significant side effects, immunosuppressive drugs such as methotrexate, azathioprine, or hydroxychloroquine may be used as alternative treatments.
Advanced cases of sarcoidosis that affect critical organs like the heart or lungs may require more aggressive treatment and specialized care. In rare instances, a lung transplant may be considered if sarcoidosis severely damages lung tissue and impairs breathing. Early diagnosis, personalized treatment, and regular follow-up care are essential for managing sarcoidosis effectively and minimizing long-term complications.
Table of Contents
When to See a Doctor
Monitoring symptoms and recognizing when to seek medical care are crucial for managing sarcoidosis effectively. Although many cases of sarcoidosis are mild and may resolve without treatment, certain symptoms can indicate a need for medical attention and possible intervention.
Signs to see a doctor:
- Persistent shortness of breath or chest pain. If you experience ongoing difficulty breathing, chest pain, or a persistent cough, these could signal lung involvement and should be evaluated promptly.
- Vision problems or eye pain. Sarcoidosis can affect the eyes, causing redness, pain, blurred vision, or sensitivity to light. Immediate medical care can help prevent long-term damage to your vision.
- Unexplained skin rashes or lesions. If you notice new or unusual rashes, lumps, or skin discolorations, it could be a sign of sarcoidosis affecting the skin, requiring further examination.
- Swelling or pain in joints. Sarcoidosis can cause joint inflammation, leading to pain, stiffness, or swelling, which may need anti-inflammatory treatment.
- Heart palpitations or fainting. In rare cases, sarcoidosis can impact the heart, causing irregular heartbeats or dizziness. These symptoms should be addressed immediately due to potential cardiac involvement.
Seeking medical care when these symptoms appear can prevent complications and ensure that sarcoidosis is managed appropriately.
What Type of Doctor to Seek
Your initial evaluation can be done by a primary care physician. However, for ongoing care, a pulmonologist—a lung specialist—is typically recommended for cases where sarcoidosis affects the lungs. Depending on the organs involved, you may also need care from other specialists, such as a rheumatologist for joint symptoms, a dermatologist for skin issues, or an ophthalmologist for eye complications.
What to Expect From Your Visit to a Doctor
During your visit, the doctor will review your medical history, discuss your symptoms, and perform a physical exam. Diagnostic tests may be ordered to determine the extent of sarcoidosis and assess any organ involvement, such as:
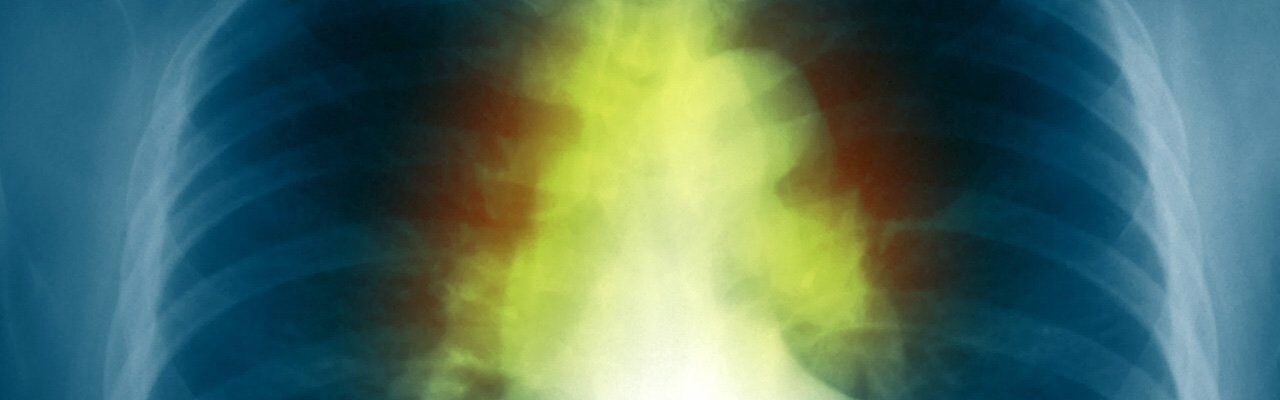
- Chest X-ray or CT scan. These imaging tests help evaluate lung involvement and detect granulomas or inflammation.
- Blood tests. Blood work can assess organ function and inflammatory markers, providing insights into disease activity.
- Pulmonary function tests. These tests evaluate lung capacity and function, which may be impaired in sarcoidosis.
- Biopsy. In some cases, a biopsy of affected tissue may be necessary to confirm the diagnosis and evaluate granulomas.
Based on the results, the doctor will create a treatment plan and recommend lifestyle changes to manage symptoms. Regular follow-up visits are essential for tracking the disease’s progress and adjusting treatments as needed to maintain quality of life and prevent complications.
Sarcoidosis Treatment Options

Image Source: www.freepik.com
In many cases, sarcoidosis can resolve on its own without the need for treatment, especially if symptoms do not interfere with daily activities. However, if symptoms cause discomfort or impact quality of life, the following treatments may be considered:
- Various Medications. When granulomas (clusters of immune cells) in organs pose a risk to overall health, doctors may prescribe the following medications:
- Corticosteroids. Corticosteroids are often the first line of treatment for sarcoidosis due to their effectiveness in reducing inflammation. They are commonly administered in tablet form, but topical corticosteroid creams may be used for skin lesions, and corticosteroid eye drops can treat inflammation in the eyes.
- Immunosuppressive Medications. To suppress an overactive immune response, patients may be prescribed drugs like methotrexate or azathioprine. These medications help control inflammation and reduce immune activity, preventing further damage to affected organs.
- Hydroxychloroquine. Often used for skin lesions and to reduce elevated calcium levels in the blood, hydroxychloroquine can be particularly helpful for patients with skin-related sarcoidosis symptoms.
- Tumor Necrosis Factor-alpha (TNF-alpha) Inhibitors. Typically used to treat rheumatoid arthritis, TNF-alpha inhibitors can also be effective for sarcoidosis patients, especially if other medications have not been successful in managing symptoms.
- Organ Transplant. For patients with severe organ damage, such as to the lungs, heart, or liver, an organ transplant may be considered. A transplant can improve quality of life and longevity when sarcoidosis has caused irreversible organ failure.
- Symptom-Based Therapies. Additional treatments may be recommended based on specific symptoms:
- Physical Therapy. For patients experiencing muscle weakness or joint pain, physical therapy can help improve strength and mobility.
- Pulmonary Rehabilitation. For those with breathing issues, pulmonary rehabilitation can help manage respiratory symptoms and enhance lung function.
- Cardiac Pacemaker. In cases where sarcoidosis affects the heart and leads to irregular heartbeats, a pacemaker may be implanted to regulate heart rhythm.
Sarcoidosis is generally not a life-threatening condition, especially when symptoms are mild. Many individuals with sarcoidosis can lead healthy and active lives. In most cases, symptoms resolve within two years, even without treatment. However, regular monitoring and appropriate management can ensure that the condition does not lead to complications, allowing patients to maintain a good quality of life.
Sarcoidosis Prognosis
The prognosis for sarcoidosis varies widely depending on the organs involved, the severity of symptoms, and the individual’s overall health. In many cases, sarcoidosis is mild and may resolve on its own within a few months to years without requiring treatment. For these individuals, the outlook is generally positive, and they may experience little to no long-term effects.
However, some patients may develop chronic sarcoidosis, where symptoms persist or recur over time, requiring ongoing treatment and monitoring. Chronic sarcoidosis can lead to complications, particularly if it affects critical organs like the lungs, heart, or eyes. In cases where sarcoidosis causes fibrosis (scarring) in the lungs or other organs, there may be a risk of permanent organ damage, which can impact quality of life and life expectancy.
With early diagnosis, regular follow-up, and appropriate treatment, many individuals with sarcoidosis can manage their symptoms and maintain a good quality of life. Advances in treatment have improved outcomes for those with more severe or chronic forms of the disease. Ongoing care and lifestyle adjustments can help prevent complications, making long-term management achievable for most patients.