Overview
Alzheimer’s disease is a progressive neurological disorder and the most common cause of dementia, primarily affecting older adults. It is characterized by the deterioration of brain cells, leading to a decline in cognitive abilities such as memory, thinking, and reasoning. The exact cause is not fully understood, but it is believed to result from a combination of genetic, environmental, and lifestyle factors. Hallmarks of the disease include the buildup of amyloid plaques and tau tangles in the brain, which disrupt normal brain function.
The effects of Alzheimer’s disease extend beyond memory loss. In the early stages, individuals may experience forgetfulness and difficulty recalling recent events. As the disease progresses, symptoms worsen to include confusion, disorientation, difficulty with language and communication, changes in personality and behavior, and eventually a loss of independence. In advanced stages, individuals often require full-time care, as they lose the ability to perform basic activities like eating, dressing, and bathing.
Currently, there is no cure for Alzheimer’s disease, but treatments focus on managing symptoms and slowing its progression. Medications such as cholinesterase inhibitors (e.g., donepezil, rivastigmine) and NMDA receptor antagonists (e.g., memantine) can help improve memory and cognitive function in some individuals. Non-pharmacological approaches, including cognitive therapies, physical activities, and creating structured routines, are also used to support individuals and their caregivers.
While Alzheimer’s is a challenging condition, early diagnosis and intervention can improve quality of life for both patients and caregivers. Ongoing research into therapies targeting amyloid plaques, tau tangles, and other biological mechanisms offers hope for future advancements in treatment. With the right support, individuals with Alzheimer’s can maintain dignity and comfort throughout the disease’s progression.
Table of Contents
When to See a Doctor
Recognizing the early signs of Alzheimer’s disease and seeking medical attention promptly can lead to better management and improved quality of life. If you or a loved one experiences any of the following symptoms, it is recommended to consult a healthcare professional.
Signs to see a doctor:
- Frequent memory loss. Forgetting recently learned information, important dates, or events and needing frequent reminders can be an early indicator of Alzheimer’s.
- Difficulty completing familiar tasks. Struggling to carry out routine activities, such as cooking, driving to a familiar location, or managing finances, may signal cognitive impairment.
- Confusion with time or place. Losing track of dates, seasons, or the passage of time, as well as forgetting where you are or how you got there, warrants medical attention.
- Changes in language or communication. Difficulty following or joining conversations, struggling to find the right words, or frequently repeating oneself may be a sign of Alzheimer’s.
- Mood or personality changes. Experiencing unusual anxiety, depression, irritability, or withdrawal from social activities may indicate early stages of cognitive decline.
- Family history or risk factors. If you have a family history of Alzheimer’s or other risk factors such as high blood pressure, diabetes, or a sedentary lifestyle, regular screenings are advisable.
Early diagnosis not only provides clarity but also opens opportunities for treatment options that may slow disease progression and improve symptom management.
What Type of Doctor to Seek
If you or a loved one is experiencing symptoms that may indicate Alzheimer’s disease, the first step is to consult a primary care physician or family doctor. These doctors can evaluate your medical history, perform initial screenings, and rule out other potential causes of cognitive decline, such as vitamin deficiencies, thyroid disorders, or depression. Based on the findings, they may recommend further evaluation by a specialist.
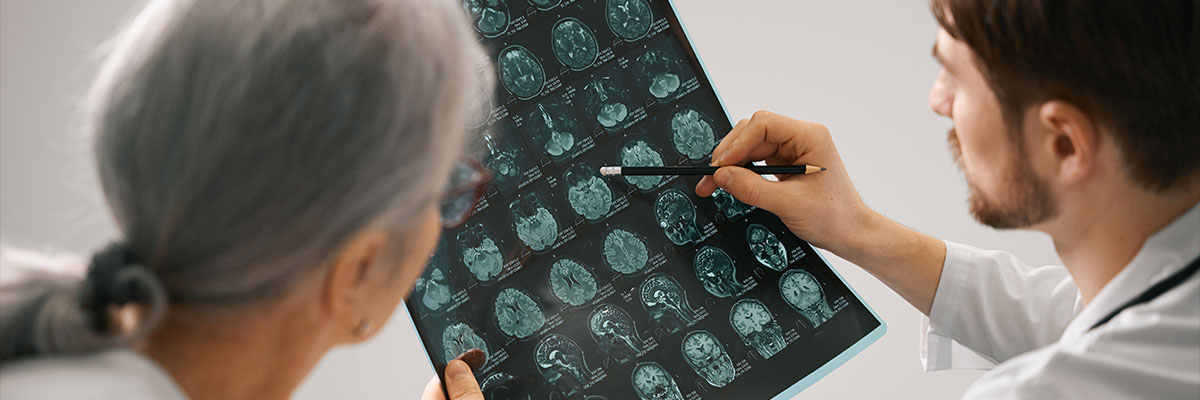
For a more comprehensive assessment, a neurologist is the most appropriate specialist to consult. Neurologists focus on disorders of the brain and nervous system, including Alzheimer’s disease and other forms of dementia. They may use advanced diagnostic tools such as brain imaging (MRI or CT scans) and neuropsychological tests to confirm the diagnosis and assess the stage of the disease. In some cases, a geriatrician, who specializes in the care of older adults, or a psychiatrist may also be involved to address behavioral and emotional symptoms associated with the condition. Working with a team of specialists ensures a well-rounded approach to diagnosis and treatment.
What to Expect from Your Visit to a Doctor
When visiting a doctor for Alzheimer’s disease concerns, the initial appointment will focus on evaluating symptoms, medical history, and overall health. The doctor will ask detailed questions about memory issues, changes in behavior, and difficulties with daily tasks. They may also review personal and family medical histories to assess risk factors. A physical examination will be conducted to rule out other potential causes of cognitive impairment, such as infections, vitamin deficiencies, or metabolic disorders.
Diagnostic tests will likely be ordered to confirm or rule out Alzheimer’s disease. These may include cognitive and memory tests to evaluate problem-solving, language, and memory skills. Blood tests and imaging studies, such as an MRI or CT scan, may also be performed to look for brain abnormalities or other medical conditions contributing to symptoms. Based on the findings, the doctor will provide a diagnosis and discuss a personalized care plan, including medications, therapies, and lifestyle recommendations. If needed, referrals to specialists such as neurologists or geriatricians may be made for further management.
Alzheimer’s Disease Treatment Options

Although Alzheimer’s disease cannot be cured, several treatments and therapies are available to help slow its progression and manage symptoms. These approaches focus on improving the patient’s quality of life and supporting their cognitive, emotional, and behavioral health. Below are the most common medications and therapies used to address Alzheimer’s disease:
- Taking prescribed medications. Various medications are available to target different aspects of Alzheimer’s disease. These include acetylcholinesterase inhibitors, memantine, and medications for behavioral and psychological symptoms of dementia (BPSD).
- Acetylcholinesterase inhibitors (AChE). These medications increase the levels of acetylcholine, a chemical essential for communication between nerve cells in the brain. By enhancing this communication, these drugs help delay cognitive decline in individuals with mild to moderate Alzheimer’s. Commonly prescribed AChE inhibitors include donepezil, galantamine, and rivastigmine. They are most effective in the earlier stages of the disease.
- Memantine. This medication is typically prescribed for moderate to severe Alzheimer’s cases. It works by regulating glutamate, a chemical that, in excessive amounts, can damage brain cells. Memantine helps preserve brain function and delay further deterioration.
- BPSD medications. These medications manage behavioral and psychological symptoms of dementia, such as anxiety, aggression, delusions, wandering, and depression. While they do not slow the disease’s progression, they can significantly improve the patient’s emotional stability and overall well-being.
- Undergoing different types of therapy. Therapies complement medications by supporting cognitive function, emotional health, and daily activities. These include cognitive stimulation therapy, cognitive rehabilitation, and reminiscence and life story work.
- Cognitive stimulation therapy (CST). In CST, individuals participate in group activities that encourage decision-making and mental engagement. Activities may include storytelling, listening to music, singing, playing word games, or following recipes. These activities help sharpen thinking skills and boost social interaction.
- Cognitive rehabilitation. This therapy focuses on helping patients relearn or remember tasks they may have forgotten. A healthcare professional guides the individual in activities such as using a cellphone, operating appliances, or completing simple repairs, promoting independence.
- Reminiscence and life story work. This therapy involves recalling and sharing past experiences, often using photos or memorabilia. It helps patients reflect on their life in a positive way, improving their mood and emotional well-being.
While these treatments and therapies do not cure Alzheimer’s disease, they can help patients maintain their independence, manage symptoms, and enjoy an improved quality of life. Combining medication with therapy provides a holistic approach, addressing both cognitive and emotional needs. Regular consultation with healthcare professionals ensures the treatment plan is tailored to the individual’s unique situation.
Alzheimer’s Disease Prognosis
The prognosis for Alzheimer’s disease varies depending on the treatment options used and the stage of the disease. While no treatment can cure or stop the progression of Alzheimer’s, the available medications and therapies can significantly improve quality of life and delay symptom progression. Below is an overview of the expected outcomes for common treatments:
- Acetylcholinesterase inhibitors (AChE). These medications are effective in managing symptoms during the early to moderate stages of Alzheimer’s. They help maintain cognitive function for months to years, though their benefits may diminish as the disease progresses.
- Memantine. Used for moderate to severe cases, memantine can help preserve daily functioning and delay the progression of severe symptoms. It is often combined with AChE inhibitors for a more comprehensive effect.
- BPSD medications. These drugs are highly effective in managing behavioral symptoms such as anxiety, aggression, and depression. While they don’t address cognitive decline, they improve the patient’s emotional stability and reduce stress for caregivers.
- Cognitive stimulation therapy (CST). CST helps enhance cognitive abilities and social engagement, particularly in the early to moderate stages. Regular participation can improve memory, decision-making skills, and overall mood.
- Cognitive rehabilitation. This therapy promotes independence by helping patients relearn everyday tasks. It is most effective in the earlier stages of Alzheimer’s, when patients can still apply the skills they relearn.
- Reminiscence and life story work. This therapy supports emotional well-being by fostering positive memories and improving mood. It is especially helpful in reducing feelings of isolation and depression.
While these treatments and therapies cannot halt Alzheimer’s disease, they provide valuable support in managing symptoms and maintaining dignity. A combination of approaches tailored to the individual’s needs offers the best chance for improving their overall quality of life.