Overview
Wilson’s Disease is a rare genetic disorder that prevents the body from properly eliminating excess copper, leading to its accumulation in vital organs such as the liver, brain, and eyes. It is caused by mutations in the ATP7B gene, which plays a key role in copper transport and excretion. Without treatment, this buildup can cause severe damage to the affected organs and lead to life-threatening complications.
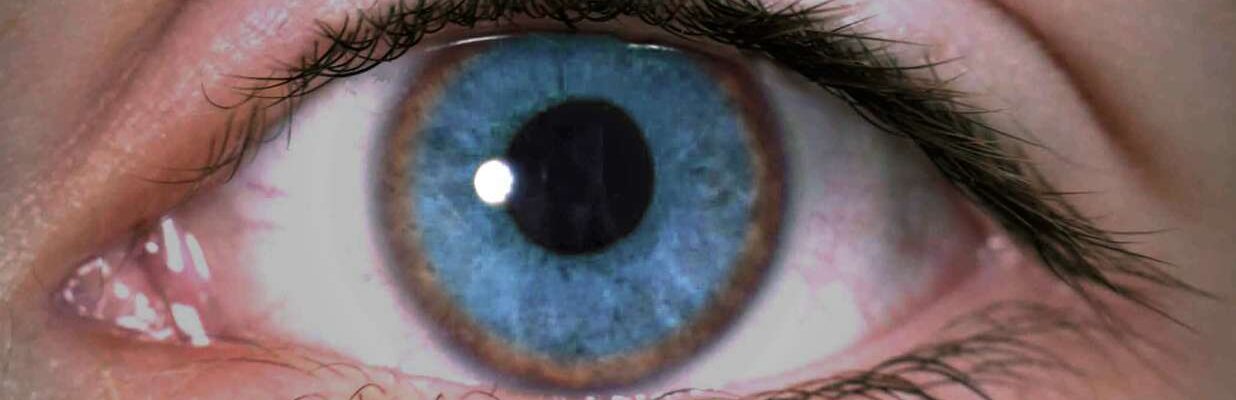
The effects of Wilson’s Disease depend on the extent and location of copper accumulation. In the liver, copper buildup may cause chronic liver disease, hepatitis, or cirrhosis. In the brain, it can lead to neurological and psychiatric symptoms such as tremors, difficulty speaking, mood swings, and depression. Copper deposits in the eyes can cause Kayser-Fleischer rings, a hallmark sign of the disease. Symptoms typically appear between the ages of 5 and 35 but can occur earlier or later.
Treatment for Wilson’s Disease aims to reduce copper levels in the body and prevent further accumulation. Chelating agents like penicillamine or trientine are commonly prescribed to bind with copper and facilitate its excretion through urine. Zinc salts may also be used to block copper absorption from food. In severe cases where liver damage is advanced, a liver transplant may be necessary. Dietary adjustments, such as avoiding copper-rich foods like shellfish and nuts, are also part of the treatment plan.
With early diagnosis and lifelong treatment, individuals with Wilson’s Disease can lead healthy, fulfilling lives. Regular monitoring and adherence to therapy are crucial to managing the condition and preventing complications. Advances in medical care continue to improve outcomes for those living with this rare disorder.
Table of Contents
When to See a Doctor
Early diagnosis and treatment of Wilson’s Disease are essential to prevent severe organ damage and improve long-term outcomes.

Signs to see a doctor:
- Family history of Wilson’s Disease. If you have a relative diagnosed with Wilson’s Disease, it’s important to undergo genetic testing or screening to determine if you are a carrier or affected by the condition.
- Unexplained liver symptoms. Symptoms such as jaundice, fatigue, abdominal pain, or swelling in the legs and abdomen may indicate liver damage caused by copper accumulation. Immediate evaluation is crucial to identify the cause.
- Neurological or psychiatric changes. If you experience tremors, difficulty with coordination, mood swings, or depression without a clear cause, consult a doctor. These could be signs of copper buildup in the brain.
- Presence of Kayser-Fleischer rings. If an eye exam reveals brown or golden rings around the cornea, it may be a sign of Wilson’s Disease. An ophthalmologist or general physician can refer you for further evaluation.
- Delayed diagnosis or persistent symptoms. If you have symptoms suggestive of liver disease or neurological issues that do not respond to standard treatments, a thorough evaluation for rare conditions like Wilson’s Disease may be necessary.
Seeking medical attention early ensures timely diagnosis and appropriate treatment. Proactive evaluation and testing are key to managing Wilson’s Disease effectively and preventing complications.
What Type of Doctor to Seek
If you suspect Wilson’s Disease or have been diagnosed with it, the first step is to consult a primary care physician. They can evaluate your symptoms, perform preliminary blood and urine tests, and refer you to a specialist for further diagnosis and treatment.
For comprehensive care, you may be referred to a hepatologist (a liver specialist) or a neurologist, depending on the predominant symptoms. Hepatologists focus on managing liver damage caused by copper accumulation, while neurologists address neurological and psychiatric symptoms. In complex cases, a geneticist may also be involved to confirm the diagnosis through genetic testing. A multidisciplinary approach ensures that all aspects of the disease are effectively managed.
What to Expect from Your Visit to a Doctor
During your visit, the doctor will start by asking about your symptoms, medical history, and family history of liver or neurological disorders. They will inquire about signs such as fatigue, jaundice, tremors, difficulty walking, or mood changes, which may indicate Wilson’s Disease. If a family member has been diagnosed with the condition, they may recommend screening even if you are asymptomatic.
You can expect a physical examination and diagnostic tests to confirm or rule out Wilson’s Disease. These may include blood tests to check copper levels, liver function, and ceruloplasmin (a copper-binding protein); urine tests to measure copper excretion; and imaging tests like an MRI or CT scan to assess organ damage. An eye exam may also be performed to check for Kayser-Fleischer rings, a telltale sign of the disease. If needed, a liver biopsy or genetic testing may be recommended to confirm the diagnosis. Based on the findings, the doctor will discuss a tailored treatment plan and next steps for managing the condition effectively.
Wilson’s Disease Treatment Options
The primary goal of treating Wilson’s Disease is to eliminate excess copper from the body and prevent further accumulation. Early and consistent treatment significantly improves outcomes and allows individuals to lead healthy, normal lives. Below are the most common treatment options:
Medical Treatments
- Chelating agents. Medications like penicillamine and trientine bind to excess copper in the body, allowing it to be excreted through urine. Another option, zinc acetate, prevents the absorption of copper from food, gradually reducing its levels. These treatments are typically taken for several months to years, depending on the severity of the condition, and require regular monitoring by a healthcare provider.
- Low-copper diet. Patients are advised to follow a diet low in copper to reduce intake. Foods rich in copper, such as mushrooms, nuts, chocolate, shellfish, dried fruits, sesame seeds, and liver, should be avoided. Copper-free options, including beef, eggs, tomatoes, rice, cereal, milk, cheese, and tea, can be safely consumed. This dietary adjustment complements medical treatments to manage copper levels effectively.
Supportive Therapies
- Physical therapy. For patients with neurological symptoms, physical therapy can help restore muscle coordination and strength. While symptoms may not fully resolve until copper levels are reduced, therapy supports gradual recovery and adapts to physical challenges.

Surgical Interventions
- Liver transplant. In severe cases where the liver is extensively damaged, a liver transplant may be necessary. This procedure involves replacing the diseased liver with a healthy one from a donor. The donor liver may come from a deceased individual or a living relative, with only a portion of the liver transplanted. Since the liver has the ability to regenerate, both the donor and recipient typically recover well.
Outlook for Patients
When diagnosed and treated early, Wilson’s Disease has an excellent prognosis, and most individuals can lead normal, active lives. However, delayed diagnosis may result in permanent damage to the liver and brain, even with treatment. Consistent medical care, adherence to prescribed therapies, and regular monitoring are essential for managing the condition and preventing complications.
Wilson’s Disease Prognosis
The prognosis for Wilson’s Disease depends on the stage at which it is diagnosed and how promptly treatment begins. With early and consistent treatment, most patients experience significant improvement and can live healthy lives. Below is an overview of the expected outcomes for each treatment option:
Medical Treatments
- Chelating agents. These medications effectively remove excess copper from the body, with most patients experiencing a marked reduction in symptoms within months. Lifelong treatment ensures copper levels remain under control, preventing further complications.
- Low-copper diet. When combined with medication, a low-copper diet helps maintain optimal copper levels. While dietary changes alone cannot resolve the condition, they play a crucial supportive role in preventing copper buildup.
Supportive Therapies
- Physical therapy. For patients with neurological symptoms, physical therapy aids in restoring motor skills and muscle strength. While recovery is gradual, most patients see significant improvement with consistent therapy as copper levels decrease.
Surgical Interventions
- Liver transplant. In cases of severe liver damage, liver transplantation offers a high success rate. Most patients experience a full recovery of liver function and resolution of symptoms related to copper toxicity, allowing them to return to normal activities.
With early detection and adherence to treatment, the prognosis for Wilson’s Disease is excellent. Regular monitoring, lifelong treatment, and lifestyle adjustments are key to managing the condition effectively and preventing long-term complications.