Overview
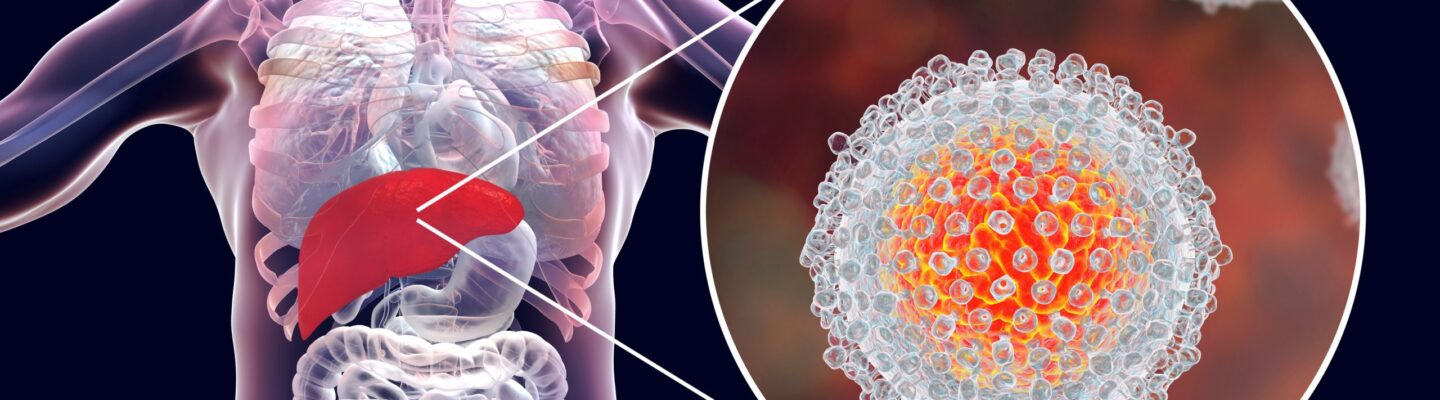
Hepatitis is an inflammation of the liver commonly caused by viral infections, though it can also result from alcohol use, toxins, or autoimmune conditions. The most prevalent forms of viral hepatitis are hepatitis A, B, C, D, and E, each differing in transmission, progression, and treatment methods. The goals of hepatitis treatment are to reduce liver inflammation, prevent disease progression, and manage symptoms, thereby preserving liver function.
Treatment approaches vary based on the type and severity of hepatitis. For acute hepatitis, treatment often focuses on supportive care, allowing the body to fight off the infection and heal naturally. Chronic hepatitis, however, may require more targeted interventions. Antiviral medications are frequently used to control chronic hepatitis B and C infections, aiming to reduce viral load and slow liver damage. In cases of hepatitis B, medications like tenofovir and entecavir help suppress the virus, while direct-acting antivirals (DAAs) can effectively cure hepatitis C for many patients.
For non-viral hepatitis, treatments may include lifestyle changes, such as alcohol cessation, and medications to address autoimmune responses or reduce toxin exposure. In severe cases where liver damage has progressed to cirrhosis or liver failure, a liver transplant may be necessary.
With early diagnosis and appropriate treatment, many forms of hepatitis can be effectively managed, and in some cases, cured. Regular monitoring, lifestyle adjustments, and adherence to prescribed treatments are essential in protecting liver health and preventing complications.
Table of Contents
When to See a Doctor
Recognizing when to seek medical attention for hepatitis is essential for preventing liver damage and ensuring effective treatment. Early intervention can help control the progression of the disease and reduce the risk of complications. While mild cases of hepatitis can sometimes resolve on their own, certain symptoms and risk factors indicate the need for a doctor’s evaluation.
Signs to see a doctor:
- Yellowing of the skin or eyes (jaundice). This is a common symptom of hepatitis and indicates liver involvement that requires medical assessment.
- Dark urine or pale stools. Changes in urine and stool color can signal liver issues, making it important to consult a healthcare provider.
- Unexplained fatigue and weakness. Persistent fatigue or weakness, especially if accompanied by other symptoms, may indicate hepatitis and warrants a medical check-up.
- Abdominal pain or swelling. Discomfort in the upper right abdomen, where the liver is located, could be a sign of liver inflammation or damage.
- Nausea, vomiting, or loss of appetite. These digestive symptoms are commonly associated with hepatitis and may require medical attention.
Promptly addressing these symptoms can help in the early detection and treatment of hepatitis, reducing the risk of long-term liver damage.
What Type of Doctor to Seek
A primary care physician can provide an initial evaluation and refer you to a specialist if hepatitis is suspected. For ongoing management, a hepatologist, a doctor specializing in liver diseases, or a gastroenterologist, a specialist in digestive system health, may be consulted. These specialists can offer targeted treatment and monitor liver function effectively.
What to Expect From Your Visit to a Doctor
During your visit, the doctor will review your symptoms, medical history, and potential exposure to hepatitis risk factors. A physical examination will focus on signs of liver inflammation, such as abdominal tenderness or jaundice.
Diagnostic tests may be recommended to confirm hepatitis and determine its type and severity, including:
- Blood tests. These tests can detect liver enzymes, bilirubin levels, and viral markers, helping diagnose hepatitis and assess liver function.
- Ultrasound or imaging scans. Imaging tests provide detailed views of the liver, identifying inflammation, enlargement, or signs of damage.
- Liver biopsy. In some cases, a liver biopsy may be performed to examine liver tissue and assess the extent of inflammation or scarring.
Following the evaluation, the doctor will discuss your diagnosis and potential treatment options, which may include medications, lifestyle changes, or, in severe cases, further interventions. Early diagnosis and proactive management are key to controlling hepatitis and maintaining liver health over the long term.
Hepatitis Treatment Options

Image Source: liverandpancreassurgeon.com
Here are the treatment approaches for hepatitis based on its various types:
- Hepatitis A. For hepatitis A, patients primarily need sufficient rest and proper nutrition to support recovery. If symptoms such as vomiting and diarrhea occur, the doctor may prescribe medications to alleviate these issues. Since hepatitis A often resolves on its own, supportive care is usually sufficient.
- Hepatitis B. Like hepatitis A, patients with hepatitis B need rest and proper nutrition. However, if the infection becomes chronic, antiviral medications may be prescribed to reduce the viral load and slow disease progression.
- Hepatitis C. Treatment for hepatitis C typically involves antiviral medications, which have high success rates in curing the infection. However, if the liver has developed complications such as cirrhosis, the patient may be considered for a liver transplant.
- Hepatitis D. Currently, there are no effective antiviral medications specifically for hepatitis D. However, doctors may prescribe alpha interferon to help manage symptoms and reduce liver inflammation.
- Hepatitis E. There is no specific treatment for hepatitis E, but the condition often resolves on its own with supportive care. Patients are encouraged to maintain a healthy lifestyle, including proper hydration and nutrition, to support the healing process.
- Alcoholic hepatitis. To prevent the condition from worsening, patients must completely stop consuming alcohol. Unlike viral hepatitis, the liver in alcoholic hepatitis often has extensive scarring. Corticosteroids and pentoxifylline may be prescribed to reduce liver inflammation and scarring. In severe cases, a liver transplant may be considered if liver damage is extensive.
- Toxin and drug-induced hepatitis. For this type of hepatitis, patients must discontinue any medications or substances that contain harmful toxins. Treatment typically involves supportive care, and symptomatic relief medications may be given if necessary.
- Autoimmune hepatitis. Autoimmune hepatitis requires lifelong treatment with maintenance medications, such as prednisone and azathioprine, to reduce liver inflammation. If the condition becomes severe, a liver transplant may be needed.
Overall, viral and drug-induced hepatitis are generally easier to manage than alcoholic and autoimmune hepatitis. This is because viral and drug-induced hepatitis often involve inflammation without significant liver scarring. In contrast, alcoholic and autoimmune hepatitis may lead to substantial liver scarring, making treatment more challenging. Viral hepatitis often improves on its own with adequate rest, a high-calorie diet, and proper hydration. However, if the condition becomes severe, hospitalization may be required to carefully monitor and control food and fluid intake.
With early diagnosis, appropriate treatment, and lifestyle changes, many forms of hepatitis can be effectively managed, preserving liver function and reducing the risk of complications.
Hepatitis Prognosis
The prognosis for hepatitis varies widely depending on the type of hepatitis, the severity of liver damage, and how promptly treatment is received. With early diagnosis and appropriate treatment, many forms of hepatitis can be managed effectively, and some types can even be cured. For example, hepatitis A and E are often acute and typically resolve on their own with supportive care, leading to a full recovery. Hepatitis B and C, however, can become chronic and require ongoing treatment to prevent complications.
For individuals with chronic hepatitis B or C, the prognosis depends on how well the virus is controlled. With antiviral medications, the progression of liver damage can be slowed or halted, significantly improving long-term outcomes. Hepatitis C, in particular, has a high cure rate with direct-acting antiviral (DAA) therapy. However, untreated or poorly managed chronic hepatitis can lead to severe complications, including cirrhosis, liver failure, and liver cancer.
Non-viral forms of hepatitis, such as alcoholic hepatitis or autoimmune hepatitis, also have variable outcomes. Lifestyle changes, such as stopping alcohol consumption, and medications to reduce inflammation can improve the prognosis for non-viral hepatitis. In cases where liver damage progresses despite treatment, a liver transplant may be considered.
With regular monitoring, lifestyle adjustments, and adherence to treatment, individuals with hepatitis can often maintain a good quality of life and prevent further liver damage. Early intervention and proactive care are essential to achieving the best possible outcomes and minimizing the risk of long-term complications.