Overview
Mitral regurgitation (MR) is a common heart valve disorder characterized by the backflow of blood from the left ventricle into the left atrium during systole, due to incomplete closure of the mitral valve. This condition often arises when the mitral valve’s leaflets or supporting structures are damaged, leading to inefficiency in the heart’s pumping mechanism. MR can range from mild and asymptomatic to severe and life-threatening.
The disorder places an increased workload on the heart as it compensates for the regurgitated blood. Over time, the left atrium may enlarge, and pulmonary pressure can rise, potentially causing symptoms like shortness of breath, fatigue, and palpitations. In severe cases, MR can lead to heart failure, atrial fibrillation, or pulmonary hypertension. The degree of impact varies based on the severity of regurgitation and the duration of the condition.
Mitral regurgitation can be caused by a variety of factors, including mitral valve prolapse, rheumatic heart disease, endocarditis, or ischemic heart disease. Some cases are congenital, while others develop due to age-related degenerative changes or secondary conditions such as left ventricular dilatation.
Treatment for MR depends on its severity and underlying cause. Mild cases are often managed with regular monitoring and lifestyle modifications. Medications, such as diuretics and beta-blockers, may alleviate symptoms but do not cure the condition. In moderate to severe cases, surgical or transcatheter intervention is often required. Options include mitral valve repair or replacement, which can be performed via traditional open-heart surgery or minimally invasive techniques. Early diagnosis and tailored management are key to improving outcomes and maintaining quality of life for individuals with MR.
Table of Contents
When to See a Doctor
Recognizing when to consult a healthcare provider for mitral regurgitation (MR) is crucial to managing the condition effectively. Early intervention can prevent complications and improve outcomes.
Signs to see a doctor:
- Persistent shortness of breath. If you experience difficulty breathing during physical activity or while lying down, it may indicate worsening mitral regurgitation or heart strain.
- Unexplained fatigue or weakness. Constant tiredness or reduced stamina without a clear reason may be a symptom of decreased cardiac efficiency.
- Irregular or rapid heartbeat. Palpitations or episodes of atrial fibrillation can arise as MR progresses and should prompt evaluation.
- Swelling in the legs or abdomen. Fluid retention in these areas, also known as edema, is a sign of potential heart failure linked to severe MR.
- Chest pain or pressure. While less common in MR, any discomfort in the chest should not be ignored, as it may signal concurrent coronary issues or advanced disease.
- History of heart murmurs. If you have been diagnosed with a heart murmur and notice new or worsening symptoms, it’s essential to have it reassessed by a healthcare provider.
Even in the absence of symptoms, individuals with known mitral regurgitation should have regular follow-ups with a cardiologist. Routine echocardiograms help monitor the severity of the condition and guide the timing of interventions. Early diagnosis and prompt treatment can significantly improve quality of life and prevent serious complications.
What Type of Doctor to Seek
If you suspect you have mitral regurgitation or have been diagnosed with the condition, the most appropriate specialist to consult is a cardiologist. Cardiologists specialize in diagnosing and managing heart-related disorders, including valve diseases like MR. They will typically perform a physical examination, listen for heart murmurs, and order diagnostic tests such as an echocardiogram to assess the severity of regurgitation and its impact on heart function.
In advanced cases or when surgical intervention is necessary, you may be referred to a cardiothoracic surgeon or an interventional cardiologist. These specialists focus on performing procedures such as mitral valve repair or replacement, either through traditional open-heart surgery or minimally invasive techniques like transcatheter approaches. Collaboration between these specialists ensures comprehensive care, from initial diagnosis and symptom management to advanced interventions if needed.
What to Expect from Your Visit to a Doctor
When you visit a doctor regarding mitral regurgitation, the initial consultation typically begins with a thorough medical history review and a physical examination. Your doctor will ask about symptoms such as shortness of breath, fatigue, or chest discomfort, as well as any relevant family history of heart disease. During the examination, they will use a stethoscope to listen for a heart murmur—a common indicator of MR.
To confirm the diagnosis and determine the severity of the condition, your doctor will likely order diagnostic tests. An echocardiogram is the most common imaging test, as it provides detailed visuals of the heart valves and measures the extent of blood flow back into the left atrium. Additional tests, such as a chest X-ray, electrocardiogram (ECG), or stress test, may also be conducted to evaluate heart size, rhythm, and function. Based on these findings, your doctor will discuss the next steps, which may include lifestyle adjustments, medication, or referrals for surgical evaluation if necessary.
Mitral Regurgitation Treatment Options
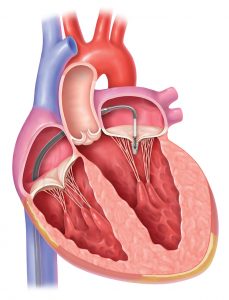
Image Source: www.froedtert.com
The treatment for mitral regurgitation (MR) varies depending on the severity of the condition and the presence of symptoms. For individuals without noticeable symptoms, immediate treatment may not be necessary, but regular monitoring is crucial to track any changes. For those experiencing symptoms, doctors often recommend a combination of medications and surgical interventions to manage the condition and prevent complications. Below are the commonly prescribed treatments:
- Medications to lower blood pressure. High blood pressure can worsen mitral regurgitation by increasing the strain on the heart. Medications such as ACE inhibitors, angiotensin II receptor blockers, or beta-blockers are often prescribed to control blood pressure and reduce the burden on the heart.
- Diuretics to reduce fluid retention. These medications help alleviate swelling (edema) by promoting the elimination of excess fluids through increased urination. Diuretics can relieve symptoms but do not address the underlying valve problem.
- Blood-thinning medications. To prevent blood clots, which are a potential complication of mitral regurgitation, doctors may prescribe aspirin or anticoagulants (blood thinners). These medications reduce the risk of stroke or other blockages in blood vessels caused by thickened blood.
While medications can provide symptom relief and reduce complications, they do not repair the faulty mitral valve. For a long-term solution, surgical or minimally invasive procedures are often necessary:
- Valve repair. If the mitral valve can be salvaged, valve repair is often the preferred surgical option. Techniques may include stitching the valve, attaching a clip to improve closure, or removing excess tissue. These procedures are usually performed through small incisions near the heart, resulting in shorter recovery times.
- Valve replacement. In cases where the mitral valve is severely damaged, replacement becomes necessary. The damaged valve is replaced with either a mechanical valve or a biological valve made from animal tissue (e.g., from pigs or cows). Mechanical valves are durable but require lifelong blood-thinning medication, while biological valves have a shorter lifespan but may not require long-term anticoagulants.
It’s important to note that medications are not a permanent solution for mitral regurgitation, as they only address symptoms and complications. For lasting improvement and to prevent further heart damage, surgical intervention is often required. Discussing options with a healthcare provider ensures that treatment is tailored to the individual’s condition and overall health.
Mitral Regurgitation Prognosis
The prognosis for mitral regurgitation largely depends on the chosen treatment and the patient’s overall health. While medications can manage symptoms and slow progression, surgical interventions often provide a more definitive solution. Here’s a breakdown of the prognosis for each treatment option:
- Medications. Medications like diuretics, blood pressure controllers, and blood thinners improve symptoms and reduce complications. However, they do not reverse the underlying valve problem. Patients may experience symptom relief, but without surgical repair or replacement, the condition can progress over time.
- Valve repair. Mitral valve repair generally has an excellent prognosis, particularly when performed before significant heart damage occurs. Patients typically regain normal heart function, with a lower risk of complications compared to valve replacement. Long-term survival rates are high, and many individuals return to normal activities within a few months.
- Valve replacement. Prognosis after valve replacement is also favorable, though it depends on the type of valve used. Mechanical valves are durable and can last a lifetime but require lifelong anticoagulation therapy, which carries risks of bleeding. Biological valves, while avoiding the need for anticoagulants, may require replacement after 10-20 years. In both cases, the surgery significantly improves symptoms and quality of life.
Each treatment option offers distinct benefits and outcomes. Early diagnosis and timely intervention are critical to achieving the best possible prognosis. With appropriate care, most patients with mitral regurgitation can lead healthier and more active lives.