Overview
Graves’ disease is an autoimmune disorder that causes the thyroid gland to produce excessive thyroid hormones, leading to a condition known as hyperthyroidism. This overproduction can cause symptoms such as weight loss, rapid or irregular heartbeat, nervousness, and heat intolerance. Treatment options for Graves’ disease aim to reduce thyroid hormone production, alleviate symptoms, and address the underlying autoimmune activity.
There are three main treatment approaches for Graves’ disease: antithyroid medications, radioactive iodine therapy, and surgery. Each option has distinct benefits and potential side effects, and the choice of treatment often depends on the patient’s age, health status, the severity of the disease, and individual preferences. In addition, lifestyle changes and supportive therapies can help manage symptoms and improve overall well-being.
Ultimately, effective management of Graves’ disease requires a personalized approach that considers the unique needs and health profile of each patient. Regular monitoring and follow-up with healthcare professionals are essential to ensure optimal outcomes and to make any necessary adjustments to the treatment plan.
Table of Contents
When to See a Doctor
If you suspect you may have symptoms of Graves’ disease or have been diagnosed with hyperthyroidism, it’s essential to know when to seek medical attention. Early evaluation and treatment can help prevent complications and improve quality of life.
Signs you should see a doctor include:
- Persistent fatigue or weakness. Experiencing ongoing tiredness, especially if accompanied by other symptoms, may indicate thyroid dysfunction and requires medical assessment.
- Rapid or irregular heartbeat. A fast or irregular pulse, especially if it occurs frequently or suddenly, could suggest excessive thyroid hormone levels and may require prompt evaluation.
- Unexplained weight loss. Losing weight without changing your diet or exercise habits could be a sign of hyperthyroidism and should be discussed with a healthcare provider.
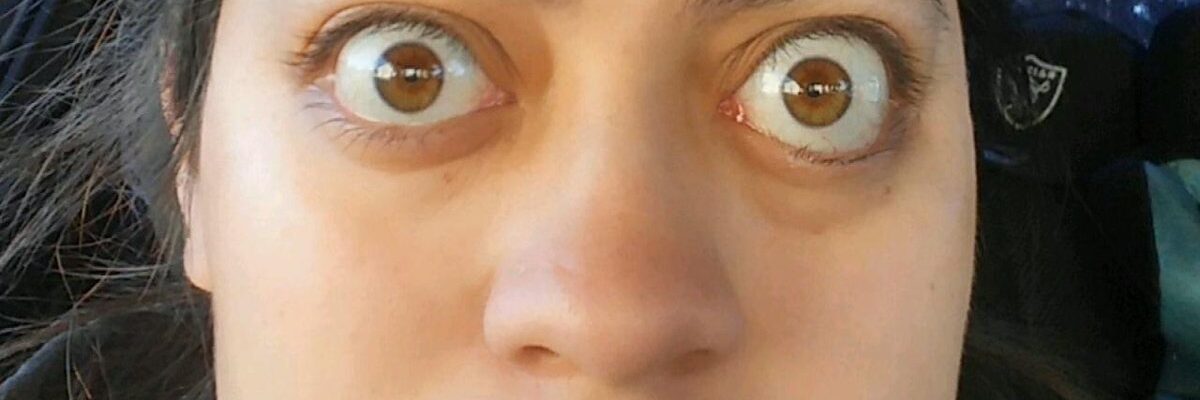
- Eye symptoms. Bulging eyes, dryness, irritation, or double vision can indicate Graves’ ophthalmopathy, a condition associated with Graves’ disease that may need specialized care.
- Increased anxiety or nervousness. If you feel more anxious, jittery, or easily agitated than usual, it may be linked to thyroid overactivity, and consulting a doctor could help determine the cause.
- Heat intolerance and excessive sweating. If you’re struggling to tolerate warm environments or experience frequent sweating, this could be a symptom of an overactive thyroid.
Early medical intervention can help manage symptoms effectively and reduce the risk of complications. Consult a healthcare provider if you notice any of these symptoms, as they can guide you on diagnostic testing and the best course of action. Regular check-ups are also advisable if you have a family history of thyroid disease or autoimmune disorders.
Graves’ Disease Treatment Options
There are three main treatments for Graves’ disease: medications, radioactive iodine therapy, and thyroid surgery. The most common treatment, especially in the United States, is radioactive iodine therapy. However, advanced medications specifically designed for this condition are becoming increasingly popular. Treatment for Graves’ disease depends on several factors, including the patient’s age, pregnancy status, and any other medical conditions.
The following are the various treatments used to manage Graves’ disease:
- Radioiodine therapy. This method involves giving the patient iodine-131, which can be in capsule or liquid form. This radioactive iodine gradually destroys the overactive thyroid cells responsible for excessive thyroid hormone production, helping reduce thyroid function to normal levels. Patients undergoing this therapy often experience gradual symptom relief as the thyroid cells die off over several weeks or months.
- Beta-blockers. These medications do not directly reduce thyroid hormone levels, but they help control symptoms until other treatments take effect. Beta-blockers alleviate symptoms such as tremors, rapid heart rate, and nervousness, providing temporary relief and improving the patient’s comfort during treatment.
- Antithyroid medications. This treatment is one of the simplest methods for managing Graves’ disease. Antithyroid medications, such as methimazole, work by reducing the production of thyroid hormone. These drugs are typically used for mild to moderate cases and can often lead to symptom control within weeks. However, long-term use may be required to maintain stable hormone levels.
- Surgery. While rare, thyroid surgery may be recommended in severe cases or when other treatments are not suitable. In this procedure, the thyroid gland is partially or completely removed to eliminate the source of excess hormone production. Surgery is particularly effective for patients with large goiters or those who do not respond to other treatments. After surgery, patients may need lifelong thyroid hormone replacement to maintain normal hormone levels.
Each treatment option has unique benefits and potential risks, and the choice will vary based on the individual patient’s health needs. Consulting with a healthcare provider to discuss these options and ongoing monitoring is essential for effective management of Graves’ disease.
Graves’ Disease Prognosis
The prognosis for Graves’ disease is generally favorable with appropriate treatment and management. While Graves’ disease is a chronic condition, most individuals can achieve effective control over their symptoms and maintain a good quality of life. Treatment options—including antithyroid medications, radioactive iodine therapy, and, in some cases, surgery—are typically successful in managing the excessive thyroid hormone production caused by the disease.
Factors influencing prognosis include:
- Response to treatment. Many people respond well to initial treatments, with some achieving remission. However, others may require long-term management to prevent recurrence of hyperthyroidism symptoms.
- Early diagnosis and intervention. Identifying Graves’ disease early and beginning treatment promptly can reduce the risk of complications, such as heart problems or bone loss, and improve overall outcomes.
- Management of Graves’ ophthalmopathy. For individuals with eye involvement, the prognosis may vary based on the severity of symptoms and the effectiveness of therapies aimed at protecting vision and reducing discomfort.
- Long-term monitoring and follow-up care. Regular follow-ups are essential to monitor thyroid hormone levels and adjust treatments as needed, helping maintain stable thyroid function over time.
With continued care and lifestyle adjustments, most individuals with Graves’ disease can lead healthy, active lives. Although Graves’ disease may have periods of recurrence, ongoing monitoring and treatment adjustments allow most patients to manage the condition effectively and minimize its impact on their daily life.