Overview
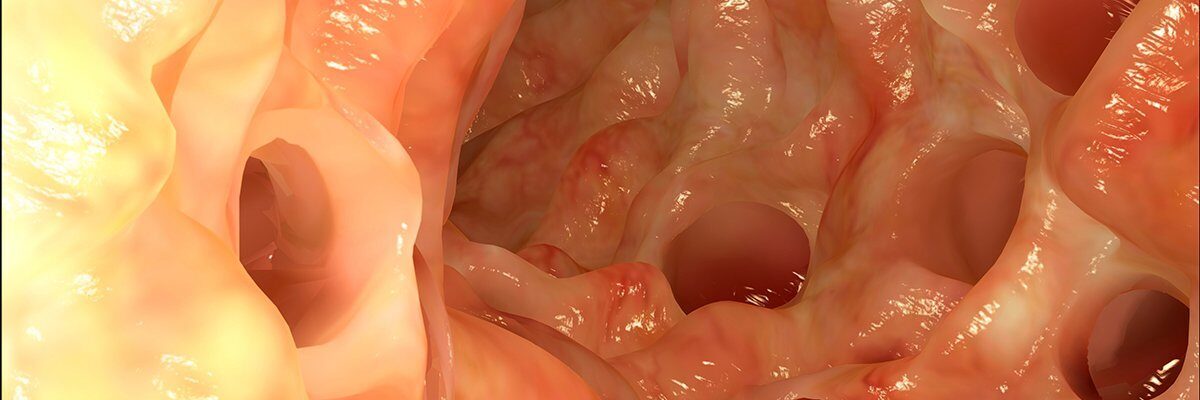
Diverticulitis is a condition where small pouches (diverticula) in the lining of the digestive tract become inflamed or infected, causing symptoms such as abdominal pain, fever, nausea, and changes in bowel habits. Treatment for diverticulitis depends on the severity of the symptoms and the extent of the inflammation or infection. The main goals of treatment are to manage symptoms, clear the infection, and prevent complications or recurrences.
For mild cases, diverticulitis can often be managed with rest, a temporary liquid diet, and antibiotics to address the infection. This approach helps relieve pressure on the digestive system, allowing the inflammation to subside. Once symptoms improve, patients are usually advised to gradually reintroduce fiber-rich foods to support healthy digestion and reduce the risk of future flare-ups.
In more severe cases, hospitalization may be necessary, especially if the patient experiences intense pain, high fever, or complications such as abscesses or perforation. Treatment in the hospital typically involves intravenous (IV) antibiotics, fluids to prevent dehydration, and sometimes a temporary dietary restriction. Surgery may be recommended if there are repeated episodes of diverticulitis or if complications arise that don’t respond to other treatments.
With prompt and appropriate treatment, most people with diverticulitis can manage the condition effectively and avoid severe complications. Adopting a high-fiber diet, staying hydrated, and regular follow-ups with a healthcare provider are key steps in maintaining digestive health and preventing future episodes of diverticulitis.
Table of Contents
When to See a Doctor
Knowing when to seek medical attention for diverticulitis is essential to prevent complications and ensure effective treatment. Mild cases can often be managed at home, but certain symptoms may indicate a more serious infection or complications that require professional care.
Signs to see a doctor:
- Severe or persistent abdominal pain. Pain in the lower left abdomen is a common symptom of diverticulitis, but if it becomes intense or does not improve, medical evaluation is recommended.
- Fever and chills. A fever, especially if accompanied by chills, may indicate an infection that requires antibiotics or further treatment.
- Nausea or vomiting. These symptoms, particularly if severe or persistent, may suggest that the digestive system is blocked or significantly inflamed.
- Changes in bowel habits. Sudden constipation, diarrhea, or bloody stools can be signs of complications and should be assessed by a healthcare provider.
Prompt medical evaluation is important to manage diverticulitis effectively and prevent serious outcomes like abscesses or perforation.
What Type of Doctor to Seek
For initial symptoms, a primary care physician can provide an assessment and recommend treatment. In more complex cases, or if complications are present, a gastroenterologist or colorectal surgeon may be consulted to provide specialized care.
What to Expect from Your Visit to a Doctor
During the visit, the doctor will review your symptoms, perform a physical examination, and may order imaging tests like a CT scan to confirm the diagnosis and assess the severity. Treatment options may include antibiotics, dietary modifications, and, in some cases, hospitalization for more intensive care. In recurrent or severe cases, surgery might be considered to prevent future episodes.
Consulting a doctor when symptoms are severe or persistent helps ensure proper diagnosis and treatment, promoting faster recovery and reducing the risk of complications from diverticulitis.
Diverticulitis Treatment Options
 Image Source: www.freepik.com
Image Source: www.freepik.com
In mild cases of diverticulitis, the condition can often be managed by the patient at home with medical guidance. This typically includes taking antibiotics and pain relievers prescribed by a doctor. It is crucial to complete the full course of these medications as directed, even if symptoms have already subsided, to ensure the infection is fully treated.
Common antibiotics prescribed for diverticulitis include:
- Ciprofloxacin
- Metronidazole
- Cephalexin
- Doxycycline
It’s important to note that antibiotics can reduce the effectiveness of contraceptive medications. This effect may last for up to seven days after stopping the antibiotic, so alternative contraceptive measures should be considered during this period.
Hospitalization may be required in the following cases:
- Severe pain that cannot be managed with standard pain relievers.
- Inability to drink sufficient fluids, leading to dehydration.
- Difficulty taking antibiotics orally.
- Patient has a weakened health status or compromised immune system.
- The doctor suspects complications or immune suppression in the patient.
- Home treatment is ineffective after two days.
For severe or recurrent cases, surgery may be considered to prevent complications or further episodes of diverticulitis.
Surgical Intervention. Patients who experience diverticulitis multiple times may be advised to undergo surgery. Without surgery, there is a higher risk of recurrence or complications from the condition. One surgical option is removing the affected portion of the large intestine, which can reduce the risk of future episodes. This procedure typically does not impact the patient’s ability to pass stool normally. However, following the surgery, patients are usually advised to slowly reintroduce solid foods, especially meats, into their diet to allow for proper healing.
With a combination of medication, lifestyle modifications, and, if necessary, surgical intervention, diverticulitis can be effectively managed, helping patients maintain a healthier digestive system and avoid future complications.
Diverticulitis Prognosis
The prognosis for diverticulitis is generally positive, especially when diagnosed early and treated promptly. Most people with mild cases respond well to antibiotics, rest, and dietary modifications, allowing them to recover fully within a few weeks. Once symptoms resolve, patients can take preventive steps, such as adopting a high-fiber diet, to reduce the risk of recurrence.
In cases of recurrent or complicated diverticulitis, the risk of further episodes and complications, such as abscesses or bowel perforation, may increase. For these individuals, additional treatments, including surgery, may be necessary to manage the condition effectively and prevent future flare-ups. The success rate for surgical treatment is high, and many patients experience significant improvement in quality of life after surgery.
Overall, with proper management and lifestyle changes, most individuals with diverticulitis can lead healthy, symptom-free lives. Regular follow-up with a healthcare provider and adherence to dietary recommendations are key to maintaining digestive health and minimizing the likelihood of further episodes.