Overview
Cervical cancer is a type of cancer that develops in the cells of the cervix, the lower part of the uterus that connects to the vagina. It is primarily caused by persistent infection with certain high-risk types of human papillomavirus (HPV), a sexually transmitted virus. While HPV infections are common and often resolve on their own, persistent infections can lead to the development of precancerous changes and, eventually, cervical cancer.
In its early stages, cervical cancer may not cause noticeable symptoms, which is why regular screening through Pap smears or HPV testing is crucial for early detection. As the disease progresses, symptoms may include abnormal vaginal bleeding (such as bleeding after intercourse, between periods, or after menopause), unusual vaginal discharge, and pelvic pain. Advanced stages of the disease can lead to more severe symptoms, including swelling of the legs, pain during urination, and kidney failure due to obstruction of the urinary tract.
Treatment for cervical cancer depends on the stage at which it is diagnosed. Early-stage cervical cancer can often be treated successfully with surgery, such as a hysterectomy or conization, which removes the affected tissue. For more advanced stages, radiation therapy and chemotherapy are commonly used, either alone or in combination. Targeted therapies and immunotherapy are newer options that may be employed in specific cases to improve outcomes.
Cervical cancer is one of the most preventable cancers, thanks to effective screening programs and HPV vaccines, which significantly reduce the risk of infection with high-risk HPV strains. Early detection through regular gynecological check-ups and preventive measures, such as vaccination and safe sexual practices, are key to reducing the global burden of cervical cancer.
Table of Contents
When to See a Doctor
Early detection of cervical cancer is crucial for effective treatment and better outcomes. It is recommended to consult a medical professional if you experience any of the following symptoms or situations.
Signs to see a doctor:
- Abnormal vaginal bleeding. Bleeding between menstrual periods, after intercourse, or after menopause should be evaluated promptly, as it is one of the most common early symptoms of cervical cancer.
- Unusual vaginal discharge. Watery, pink, or foul-smelling discharge that is not part of your regular cycle may indicate an underlying condition, including cervical cancer.
- Pelvic pain or discomfort. Persistent pain in the pelvic region, especially if it is not related to your menstrual cycle, warrants medical attention.
- Pain during intercourse. Discomfort or pain during sexual activity may signal changes in the cervix that require further investigation.
- Family history or risk factors. If you have a family history of cervical cancer, a history of HPV infection, or other risk factors, it is essential to discuss screening and preventive measures with your doctor.
Regular screening is also critical for detecting cervical cancer in its early, more treatable stages. Even without symptoms, women should follow their doctor’s recommendations for Pap smears and HPV tests based on their age and medical history. Prompt medical evaluation can make a significant difference in outcomes and overall health.
What Type of Doctor to Seek
If you have symptoms such as abnormal vaginal bleeding, unusual discharge, or pelvic pain, your first step should be to consult a gynecologist, a doctor specializing in women’s reproductive health. Gynecologists perform routine screenings, including Pap smears and HPV tests, which can detect cervical abnormalities or cancer in its early stages. They can also conduct pelvic examinations and colposcopies to examine the cervix more closely.
If cervical cancer is diagnosed or suspected, you may be referred to a gynecologic oncologist, a specialist trained in treating cancers of the female reproductive system. Gynecologic oncologists manage advanced treatments, including surgery, radiation therapy, and chemotherapy. In some cases, a multidisciplinary team of specialists, including medical oncologists and radiation oncologists, may collaborate to provide comprehensive care tailored to your condition.
What to Expect from Your Visit to a Doctor
When visiting a doctor for concerns about cervical cancer, your appointment will typically begin with a discussion about your symptoms, medical history, and risk factors, including sexual health and any prior HPV infections. The doctor may ask about your menstrual history and whether you have experienced abnormal bleeding or discharge.
A pelvic examination is often conducted to check the health of your reproductive organs. If cervical abnormalities are suspected, the doctor may perform a Pap smear or HPV test to collect cells from the cervix for analysis. In cases where further investigation is needed, a colposcopy may be done to closely examine the cervix, and a biopsy may be taken to confirm a diagnosis. After the evaluation, the doctor will discuss the findings and outline the next steps, which could include additional tests, treatment options, or referrals to a specialist. Be prepared to ask questions and express any concerns during the visit to ensure you fully understand your diagnosis and treatment plan.
Cervical Cancer Treatment Options

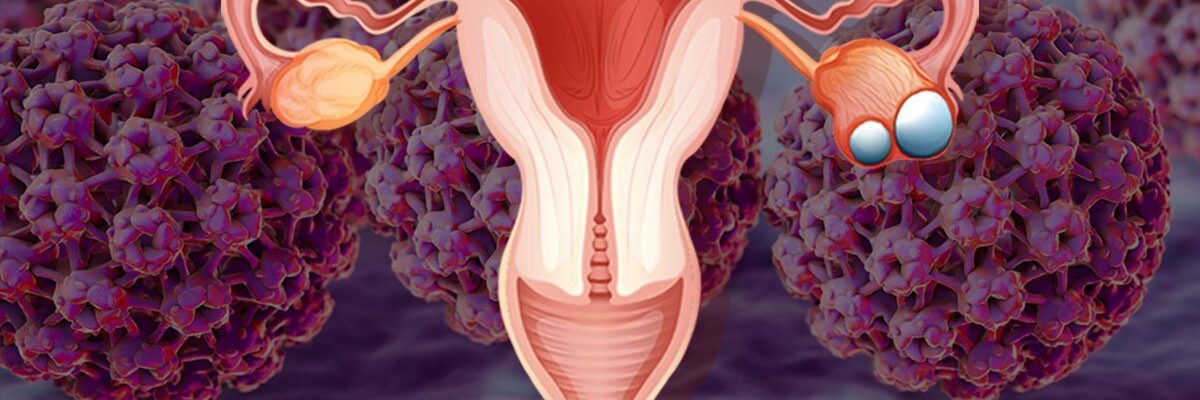
Image Source: www.freepik.com
Cervical cancer is highly treatable, especially when detected early through regular screenings. The choice of treatment depends on the stage and severity of the condition, as well as the patient’s overall health. Below are the most common treatment options available for cervical cancer:
- Surgery. Surgery is often the first line of treatment for early-stage cervical cancer. For small, localized tumors, procedures like a cone biopsy or loop electrosurgical excision (LEEP) may be used to remove the affected tissue. For more advanced cases, a hysterectomy (removal of the uterus and cervix) may be necessary, and in some instances, nearby lymph nodes may also be removed to prevent the spread of cancer.
- Chemotherapy. Chemotherapy involves the use of drugs administered orally or intravenously to kill cancer cells or stop their growth. It is often combined with radiation therapy to enhance effectiveness, especially in advanced stages. While chemotherapy is effective, it can also affect healthy cells, leading to side effects such as fatigue, nausea, and hair loss.
- Radiation therapy. Radiation therapy uses high-energy rays to target and destroy cancer cells. External beam radiation therapy directs radiation from outside the body to the affected area, while internal radiation therapy (brachytherapy) places radioactive material near the tumor inside the body. This dual approach is often used in advanced or recurrent cases.
- Targeted drug therapy. Targeted therapy focuses on attacking specific cancer cells while sparing healthy tissue. Drugs like bevacizumab (Avastin) block the blood supply to the tumor, slowing its growth and spread. This option is often used for advanced cervical cancer or in combination with other treatments.
- Immunotherapy. Immunotherapy strengthens the body’s immune system to fight cancer more effectively. Drugs such as immune checkpoint inhibitors help the immune system recognize and destroy cancer cells. This treatment is particularly useful for advanced or recurrent cases where standard therapies are less effective.
Advancements in medical technology and the availability of preventive measures, like the HPV vaccine, have significantly reduced the mortality rate of cervical cancer. Early detection through regular Pap smears and HPV testing remains essential for successful treatment. If you experience symptoms such as abnormal vaginal bleeding or pelvic pain, consult a doctor immediately to determine the cause and seek appropriate care.
Cervical Cancer Prognosis
The prognosis for cervical cancer varies depending on the stage of diagnosis, the patient’s overall health, and the treatment chosen. Early detection significantly improves outcomes, with high survival rates for localized cases. Here’s an overview of the prognosis for each treatment option:
- Surgery. Surgery has an excellent prognosis for early-stage cervical cancer, often leading to complete remission. For localized tumors, surgical procedures like cone biopsies or hysterectomies are highly effective, with a low risk of recurrence when followed by regular monitoring.
- Chemotherapy. Chemotherapy is effective for managing advanced cervical cancer or preventing recurrence after surgery or radiation therapy. While it may not cure late-stage cancer on its own, it often extends survival and improves quality of life when used in combination with other treatments.
- Radiation therapy. Radiation therapy provides a strong prognosis for patients with locally advanced cervical cancer. When combined with chemotherapy, it is highly effective at shrinking tumors and preventing the cancer from spreading, particularly in mid to advanced stages.
- Targeted drug therapy. Targeted therapies offer a promising prognosis for patients with advanced or recurrent cervical cancer. These treatments help slow tumor growth and, in some cases, significantly extend survival, particularly for cancers resistant to traditional treatments.
- Immunotherapy. Immunotherapy is a newer approach that has shown success in improving outcomes for advanced or metastatic cervical cancer. While still being studied, it offers hope for patients who have not responded to other therapies.
Cervical cancer is one of the most preventable and treatable cancers, particularly when detected early. Regular screenings, early intervention, and advances in treatment options have greatly improved survival rates, offering hope and better outcomes for patients at all stages of the disease.