Overview
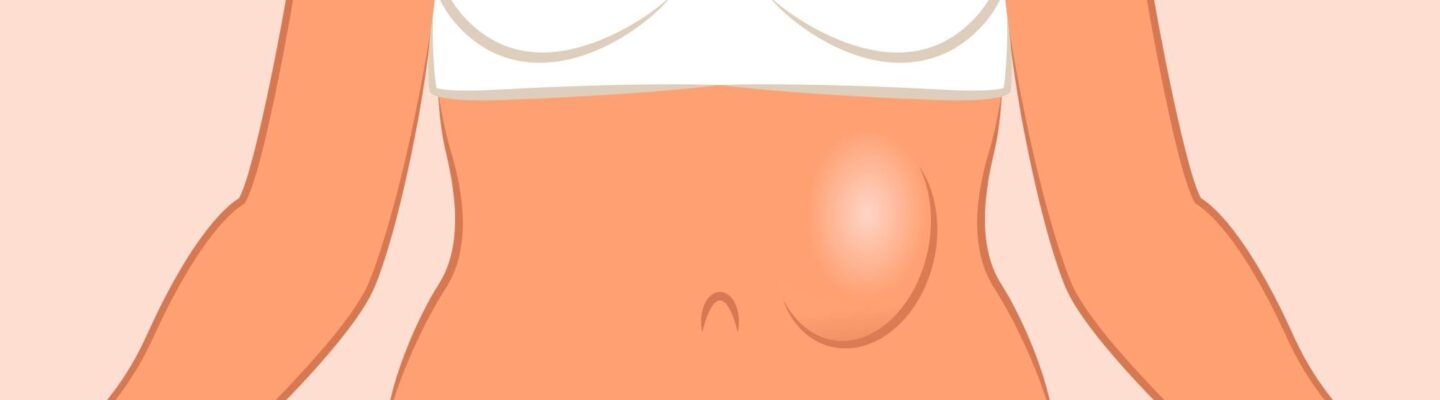
A hernia occurs when an organ or tissue pushes through a weak spot in the surrounding muscle or connective tissue. This condition commonly affects the abdominal area, though it can also appear in other regions, such as the groin or upper thigh. The most common types of hernias include inguinal (groin), umbilical (near the belly button), hiatal (upper stomach), and incisional (through a surgical scar).
Hernias often cause noticeable swelling or a bulge in the affected area, which may worsen with activities like lifting, bending, or coughing. Other symptoms include pain or discomfort, particularly during movement, and a sensation of heaviness in the affected region. In some cases, hernias may become incarcerated or strangulated, where the blood supply to the herniated tissue is cut off, leading to severe pain and a potential medical emergency.
Treatment options for hernias depend on the type, severity, and location of the hernia. In cases where the hernia is small and not causing significant symptoms, a doctor may recommend lifestyle changes, such as avoiding heavy lifting, maintaining a healthy weight, and strengthening the abdominal muscles, to manage symptoms and prevent progression. For more prominent or symptomatic hernias, surgical intervention is typically necessary. There are two main surgical methods: open surgery and minimally invasive laparoscopic surgery. Both procedures aim to repair the weakened tissue and reinforce it, often with a synthetic mesh to provide additional support.
With proper treatment, the outlook for hernia patients is generally favorable, especially when addressed before complications develop. Early diagnosis and timely intervention can significantly improve recovery outcomes and reduce the likelihood of recurrence.
Table of Contents
When to See a Doctor
Although some hernias may not cause immediate discomfort, it’s essential to seek medical attention if symptoms persist or worsen. Addressing a hernia early can prevent complications and ensure appropriate management.
- Persistent Pain or Swelling. If you experience ongoing pain, swelling, or a noticeable bulge that does not go away when lying down, it’s advisable to consult a doctor. This could indicate that the hernia is progressing and may need medical intervention.
- Worsening Symptoms with Activity. If pain intensifies during physical activities, such as lifting, bending, or even coughing, a doctor should evaluate the hernia to assess its severity and determine the best course of action.
- Sudden, Severe Pain or Hardening of the Bulge. If the hernia becomes firm, tender, or discolored and is accompanied by intense pain, it may be incarcerated or strangulated. This condition cuts off blood supply to the herniated tissue and requires immediate medical care, as it is potentially life-threatening.
- Digestive Issues. If the hernia affects your digestive tract, you might experience symptoms such as nausea, vomiting, or difficulty with bowel movements. In such cases, prompt medical attention is necessary to avoid further complications.
What Type of Doctor to Seek
In most cases, a primary care physician can provide initial evaluation and guidance. If the hernia requires specialized care or surgery, a general surgeon or a specialist in hernia repair is typically recommended. General surgeons are experienced in both open and laparoscopic hernia repair, ensuring the appropriate treatment approach for each patient.
What to Expect from Your Visit to a Doctor
During the appointment, the doctor will ask about your symptoms, medical history, and any activities that may exacerbate the hernia. They may perform a physical examination to assess the location and severity of the hernia. If necessary, imaging tests like an ultrasound, CT scan, or MRI may be ordered to gain a clearer view of the hernia’s characteristics.
The doctor will discuss treatment options based on the type and severity of the hernia, along with your health profile and lifestyle. For some patients, lifestyle adjustments and watchful waiting may be recommended, while others may be advised to undergo surgical repair to prevent further complications.
Timely consultation with a healthcare professional can ensure a favorable outcome, providing relief from symptoms and preventing potential complications associated with hernias.
Hernia Treatment Options

Image Source: www.freepik.com
According to doctors, surgery is the most effective treatment for hernias, as it directly addresses the underlying weakness in the muscle or tissue. Here are the main surgical options available:
- Open Surgery. In open surgery, the surgeon makes a single, larger incision over the hernia site to access the herniated tissue. The herniated organ or tissue is then carefully repositioned to its proper place, and the muscle wall is reinforced, often with sutures or synthetic mesh to prevent recurrence. Although recovery can take longer due to the larger incision, open surgery remains a reliable option with a high success rate.
- Laparoscopic Surgery. Compared to open surgery, laparoscopic surgery is minimally invasive and generally less painful for the patient, with quicker recovery times. In this procedure, the surgeon makes a few small incisions near the affected area and inserts a laparoscope—a thin tube equipped with a small camera and surgical tools. Using a monitor to guide the procedure, the surgeon repairs the hernia from within, often using mesh for reinforcement. Laparoscopic surgery is especially beneficial for patients who require a faster return to daily activities and have a lower risk of postoperative complications.
In certain cases, surgery may not be immediately necessary, especially if the hernia is small and not causing symptoms. However, for individuals experiencing occasional discomfort or mild symptoms, doctors may suggest non-surgical approaches to manage the hernia:
- Wearing Supportive Undergarments. Special supportive garments, such as trusses or hernia belts, provide gentle compression to keep the hernia in place and reduce discomfort. These undergarments are designed to fit snugly but comfortably, and some are adjustable to provide the right level of support. Certain designs include padding to add pressure to the hernia site, helping to keep the tissue from protruding. However, this approach only provides temporary relief, as the hernia may reappear when the support is removed.
- Medications for Symptom Relief. If the hernia causes symptoms such as pain or acid reflux, doctors may prescribe medications to manage these effects. Common medications include pain relievers for discomfort, antacids, H2 receptor blockers, and proton pump inhibitors to reduce stomach acid if a hiatal hernia is present. While these medications do not treat the hernia directly, they can alleviate some associated symptoms.
- Dietary and Lifestyle Adjustments. Including fiber-rich foods in the diet can soften stools and ease bowel movements, reducing strain on the abdominal area. This is particularly helpful in preventing the hernia from worsening. Additionally, gentle exercise, such as walking or low-impact core strengthening, can improve blood flow to the affected area and support abdominal muscle strength, helping to manage symptoms and prevent further complications.
These non-surgical methods may offer temporary relief, but surgery remains the only definitive solution for hernias. Addressing a hernia early through proper treatment and lifestyle management can significantly improve comfort and reduce the risk of complications.
Hernia Prognosis
The outlook for hernia patients is generally positive, especially when the condition is addressed promptly and managed with appropriate treatment. While hernias do not heal on their own, the prognosis varies depending on the type of hernia and the chosen treatment method. Here’s a look at the expected outcomes for common treatment options:
- Lifestyle Modifications and Watchful Waiting. For small hernias that are not causing symptoms or significantly impacting daily activities, a doctor may recommend monitoring the hernia along with lifestyle changes, such as avoiding heavy lifting, maintaining a healthy weight, and strengthening core muscles. While these measures do not cure the hernia, they can help prevent it from worsening. This approach generally has a good prognosis as long as the patient adheres to recommended lifestyle adjustments.
- Open Hernia Repair Surgery. Open surgery involves making an incision over the hernia site, repositioning the tissue, and reinforcing the area with sutures or synthetic mesh. This method has a high success rate, with most patients experiencing full recovery within several weeks. The risk of hernia recurrence after open repair is low, especially when mesh reinforcement is used, leading to an excellent long-term prognosis.
- Laparoscopic Hernia Repair. Minimally invasive laparoscopic surgery involves smaller incisions and the use of specialized tools to repair the hernia from within. This technique often results in a quicker recovery time, less postoperative pain, and a lower risk of infection. The prognosis with laparoscopic repair is also excellent, with a low chance of recurrence and a shorter downtime, making it an effective option for many patients.
- Emergency Surgery for Strangulated or Incarcerated Hernias. If a hernia becomes strangulated, cutting off the blood supply to the affected tissue, emergency surgery is required. Though more complex, prompt surgical intervention in such cases generally has a favorable prognosis if treated quickly. Recovery may take longer than with planned procedures, but the risk of recurrence remains low with proper repair techniques.
With early detection, the prognosis for hernia patients is overwhelmingly positive. Following surgery, most patients can expect a return to normal activities within a few weeks, with minimal risk of recurrence when proper precautions are taken. Routine follow-up care and lifestyle adjustments further enhance the long-term outlook, supporting overall health and reducing the likelihood of future hernias.