Overview
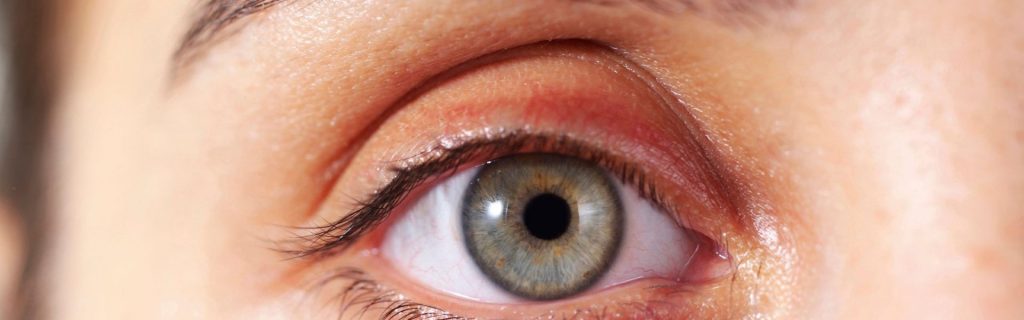
Eye inflammation is a condition that can affect individuals of all ages, occurring as a reaction to irritation, injury, or infection in the eyes. It may also serve as a symptom of allergies, inflammatory eye diseases, or autoimmune disorders.
When experiencing eye inflammation, patients may notice additional symptoms such as eye redness, pain, blurred vision, and heightened sensitivity to light. These symptoms can vary in severity depending on the underlying cause and the individual’s overall health.
Doctors consider eye inflammation a treatable condition, with recovery depending on its cause and severity. In many cases, inflammation resolves with appropriate treatment, such as prescribed antibiotics or other interventions tailored to the specific issue. While it is a relatively common condition, prompt attention is essential to prevent complications, particularly in more severe cases.
Table of Contents
Possible Causes of Eye Inflammation
To effectively treat eye inflammation, it is crucial to identify its root cause. Eye inflammation can stem from various factors, including physical injuries, infections, allergies, or underlying health conditions such as autoimmune diseases or eye disorders. Below are the common causes of eye inflammation:
- Eye injuries. Physical trauma to the eye—whether from sports, accidents, or foreign objects—can cause swelling. In addition to inflammation, patients may experience pain or even bleeding in severe cases.
- Allergies or irritation. Allergens like dust, pollen, pet dander, and hair can trigger inflammation in sensitive individuals. Allergic reactions often lead to redness, itching, and swelling of the eyes.
- Eye inflammatory diseases. Certain diseases directly affect the eyes and result in inflammation:
- Uveitis. Inflammation of the uvea, the colored part of the eye that includes the iris, choroid, and ciliary body. It may be caused by infection, trauma, or autoimmune disorders and can affect one or both eyes.
- Keratitis. Also known as corneal ulcer, keratitis involves inflammation of the cornea, often due to bacterial, viral, fungal, or parasitic infections. It can lead to pain, blurred vision, and sensitivity to light.
- Conjunctivitis (sore eyes). This common condition inflames the conjunctiva, turning the whites of the eyes pink or red. Symptoms include itching, tearing, and eye discharge.
- Thyroid eye disease. Also called Graves’ eye disease, this condition arises from an overactive thyroid gland, causing inflammation and bulging of the eyes due to excessive tissue and fat buildup behind them.
- Blepharitis. Unlike styes, which are localized bumps, blepharitis inflames the entire eyelid. Symptoms may include flaking skin, redness, and dryness.
- Dry eye syndrome. When the eyes do not produce enough moisture, they can become irritated, inflamed, and sensitive to light, leading to persistent discomfort if untreated.
- Endophthalmitis. This is a serious inflammation inside the eye caused by bacterial or fungal infections, often accompanied by pus, light sensitivity, and eyelid swelling.
- Iritis. Inflammation of the iris, often linked to trauma or infectious diseases, which can lead to eye pain, redness, and blurred vision.
- Serious eye conditions. Eye inflammation may be a symptom of more severe diseases, including:
- Orbital cellulitis. A bacterial infection of the eye socket’s soft tissues, causing severe swelling, pain, and vision loss. If untreated, it can lead to blindness, meningitis, or brain abscesses.
- Corneal abrasion. A scratch or injury to the cornea that can lead to infection, severe pain, and blurred vision if not addressed promptly.
- Autoimmune diseases. Eye inflammation is sometimes a symptom of systemic autoimmune conditions, such as:
- Rheumatoid arthritis. Although it primarily affects joints, rheumatoid arthritis can also inflame the eyes due to similarities in the tissue structures.
- Sjogren’s syndrome. This chronic condition targets glands responsible for maintaining moisture, causing dry and inflamed eyes along with mouth dryness.
- Multiple sclerosis (MS). MS affects the brain, spinal cord, and optic nerve, often leading to eye inflammation and vision issues.
- Reiter’s disease. This form of autoimmune arthritis inflames the joints, urinary tract, and eyes, often causing redness and swelling.
Understanding the cause of eye inflammation is critical for effective treatment. Early diagnosis and proper management can prevent complications and ensure quicker recovery.
When to See a Doctor
Eye inflammation can sometimes be managed with simple remedies, but certain situations require prompt medical attention. Here are key signs to watch for:
- Severe symptoms. Seek immediate medical care if the inflammation is accompanied by intense pain, sudden vision changes, or extreme sensitivity to light.
- Persistent swelling. If the redness and swelling do not improve within a few days or worsen despite home treatments, consult a healthcare provider.
- Discharge or crusting. Yellow or green discharge, excessive tearing, or crusting around the eyes could indicate an infection requiring medical treatment.
- Vision impairment. Blurry vision, double vision, or partial loss of vision associated with inflammation should be evaluated immediately.
- Recent trauma or injury. If the inflammation follows an eye injury or exposure to harmful chemicals, visit a doctor without delay.
- Associated symptoms. Additional symptoms like fever, headache, or swelling in other areas of the body could point to a more serious underlying condition, such as orbital cellulitis or an autoimmune disorder.
Prompt medical evaluation ensures the underlying cause of eye inflammation is identified and treated effectively, helping to prevent potentia
What Type of Doctor to Seek
For eye inflammation, it’s important to consult the right specialist based on the suspected cause.
- Optometrist or ophthalmologist. These eye care professionals specialize in diagnosing and treating eye conditions, including inflammation caused by infections, injuries, or allergies.
- Primary care physician. They can provide an initial evaluation and refer you to a specialist if necessary.
- Allergist. If the inflammation is linked to allergic reactions, an allergist can help identify triggers and recommend treatment.
- Rheumatologist. For inflammation caused by autoimmune diseases like rheumatoid arthritis or Sjogren’s syndrome, a rheumatologist’s expertise is essential.
What to Expect From Your First Doctor Visit
During your initial consultation, the doctor will likely:
- Review your medical history. Be prepared to discuss when the inflammation started, any associated symptoms, and any previous eye conditions or injuries.
- Conduct a physical examination. The doctor will closely examine your eyes for signs of redness, swelling, discharge, or other abnormalities.
- Order diagnostic tests. Depending on your symptoms, tests like slit-lamp examination, blood tests, or imaging studies may be recommended to determine the cause.
- Provide a treatment plan. Based on the diagnosis, you may be prescribed medications such as eye drops, antibiotics, or anti-inflammatory treatments and given advice on follow-up care.
By understanding what to expect and consulting the right specialist, you can ensure that your eye inflammation is properly managed and treated.
Eye Inflammation FAQs
Eye inflammation is a common symptom that can result from various conditions or external factors. Below are answers to some frequently asked questions about this condition to help you better understand its causes, symptoms, and treatments.
- What is eye inflammation? Eye inflammation refers to swelling, redness, and irritation of the eyes caused by injury, infection, allergies, or underlying health conditions.
- What are the symptoms of eye inflammation? Common symptoms include redness, swelling, pain, itching, blurry vision, discharge, and sensitivity to light.
- What causes eye inflammation? It can be caused by infections (e.g., conjunctivitis, keratitis), allergies, autoimmune diseases (e.g., rheumatoid arthritis, Sjogren’s syndrome), or physical trauma.
- Can eye inflammation go away on its own? Mild cases of eye inflammation, such as those caused by minor irritants or allergies, may resolve without treatment. However, persistent or severe cases require medical attention.
- When should I see a doctor for eye inflammation? Consult a doctor if symptoms are severe, persist for more than a few days, or are accompanied by vision loss, severe pain, or discharge.
- How is eye inflammation treated? Treatment depends on the cause and may include antibiotic or antiviral eye drops, antihistamines for allergies, corticosteroids, or artificial tears for dry eyes.
- Can eye inflammation cause permanent damage? If left untreated, some causes of eye inflammation, such as uveitis or orbital cellulitis, can lead to complications like vision loss or scarring.
- How can I prevent eye inflammation? Maintain good hygiene, avoid rubbing your eyes, use protective eyewear, and manage chronic conditions like allergies or autoimmune diseases to reduce risk.
- Are there home remedies for eye inflammation? Cold compresses, artificial tears, and avoiding irritants can provide relief for minor inflammation, but professional care is recommended for severe symptoms.
- Can children experience eye inflammation? Yes, children can experience eye inflammation due to infections like conjunctivitis, allergies, or injuries. Prompt medical attention is important, especially for younger children.
Understanding eye inflammation and its potential causes is essential for timely and effective treatment. If symptoms persist or worsen, seek medical advice to prevent complications and ensure proper care.


