Quick Answer: Tinea versicolor, known locally as an-an, is a common fungal skin condition caused by the overgrowth of yeast naturally present on the skin. While it cannot be entirely prevented due to its natural presence, the risk of flare-ups and recurrence can be minimized by practicing proper hygiene, avoiding triggers like excessive sun exposure and oily products, and using preventive antifungal treatments.
Loose, breathable clothing and early intervention with antifungal creams or medications can also help manage the condition effectively. For persistent or severe cases, consult a dermatologist for professional advice and treatment.
How to Prevent Tinea Versicolor?
Since the fungus that causes tinea versicolor naturally resides on the skin, there is no definitive way to eliminate the risk entirely. However, certain measures can help prevent recurrence and manage the condition effectively:
- Avoid using excessively oily products. Products like fragrant oil essences or heavy moisturizers can create an ideal environment for yeast overgrowth. Choose non-comedogenic and lightweight skincare products to reduce the risk.
- Limit sun exposure. Prolonged exposure to the sun not only triggers the condition but also makes the discoloration more apparent, especially on darker or tanned skin. Use a broad-spectrum sunscreen daily to protect your skin and prevent uneven pigmentation.
- Use antifungal creams or lotions preventively. Applying antifungal treatments, particularly in humid or hot climates, can curb fungal overgrowth and reduce the risk of flare-ups. Focus on areas prone to sweating, such as the back, chest, and neck.
- Wear loose, breathable clothing. Tight clothing can trap sweat and create a moist environment where fungi thrive. Opt for fabrics like cotton that allow better airflow and help keep your skin dry.
- Maintain good personal hygiene. Regularly wash and dry your skin thoroughly, especially after activities that cause sweating. Fungal infections are more likely to occur in areas that remain damp or unclean.
By integrating these habits into your daily routine, you can significantly lower the risk of recurring tinea versicolor. If symptoms persist despite preventive measures, seek advice from a dermatologist to explore more advanced treatment options, such as prescription medications or specialized therapies.
What Is Tinea Versicolor?
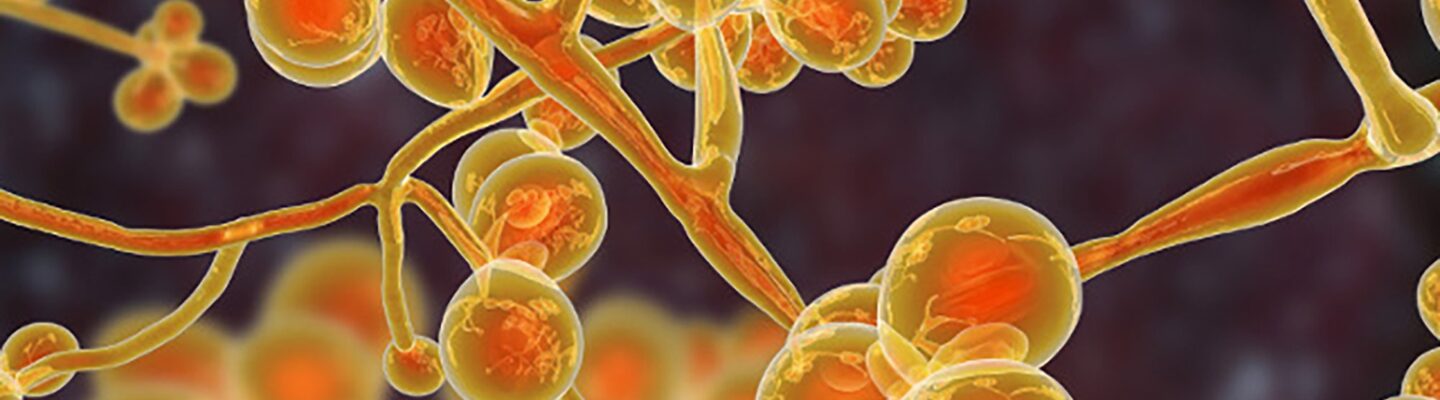
Tinea versicolor, or an-an, is a superficial fungal infection caused by an overgrowth of a type of yeast called Malassezia. This yeast is naturally present on the skin but can become problematic under certain conditions, such as excessive sweating, hormonal changes, or prolonged sun exposure. The condition is characterized by patches of skin discoloration, which may appear lighter or darker than the surrounding skin. It is most commonly seen on the chest, back, neck, and arms. While it is not contagious, it can be persistent and bothersome if left untreated.
Who Is at Risk for Tinea Versicolor?
Certain factors increase the likelihood of developing tinea versicolor. These include:
- Living in hot and humid climates. The warm, moist environment promotes yeast overgrowth.
- Excessive sweating. People who sweat heavily, such as athletes, are more susceptible.
- Oily skin. Individuals with naturally oily skin are more prone to fungal overgrowth.
- Weakened immune systems. Conditions like diabetes or the use of immunosuppressive drugs can increase risk.
- Hormonal changes. Adolescents and young adults are more commonly affected due to hormonal fluctuations that may influence skin conditions.
Understanding these risk factors can help in adopting preventive measures tailored to individual lifestyles and environments.
How Is Tinea Versicolor Treated?
Treatment for tinea versicolor typically involves antifungal medications. Options include:
- Topical antifungal treatments. These include creams, lotions, or shampoos containing active ingredients like selenium sulfide, ketoconazole, or clotrimazole. They are applied directly to the affected areas.
- Oral antifungal medications. For more severe or widespread cases, doctors may prescribe oral antifungals like fluconazole or itraconazole. These are particularly useful for recurring infections.
- Specialized therapies. Dermatologists may recommend medicated soaps or periodic maintenance treatments to prevent recurrence.
It’s important to follow the prescribed regimen and continue treatment even after symptoms improve to prevent relapse.