On October 11, 2012, a serious outbreak of fungal meningitis was confirmed in the United States, affecting over 137 people (with numbers still rising). Tragically, 12 individuals have already succumbed to the disease. The outbreak was traced to contaminated injectable pain relief medication administered to patients’ spines, leading to the spread of the infection.
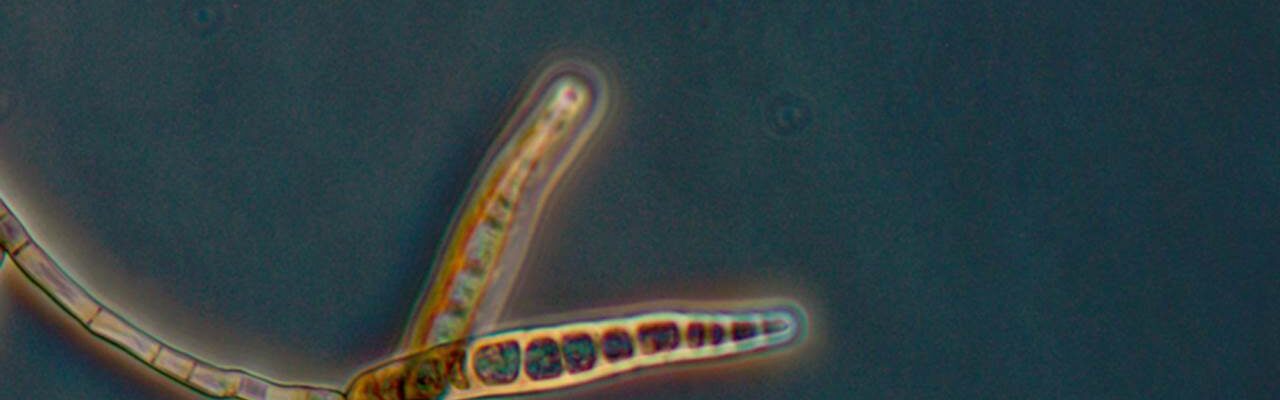
Fungal meningitis is a rare condition that causes inflammation of the protective membranes surrounding the brain and spinal cord. It is caused by fungi, a group of organisms that includes molds and mushrooms. Unlike bacterial or viral meningitis, fungal meningitis is not contagious and typically arises from specific environmental exposures or medical incidents, such as this contamination.
States Affected and Source of Contamination
According to the Centers for Disease Control and Prevention (CDC), cases have been reported in several states, including Florida, Indiana, Maryland, Michigan, Minnesota, North Carolina, Ohio, Tennessee, and Virginia. The source of the outbreak was identified as the New England Compounding Center (NECC), a pharmaceutical company that produced the contaminated drug, methylprednisolone acetate. This steroid is commonly used to treat back pain by reducing inflammation and providing pain relief.
The contamination occurred when fungal spores were introduced into the medication during production, resulting in the widespread infection among individuals who received the injections. This incident highlights significant lapses in quality control and sterility in compounding facilities.
Symptoms and Risks of Fungal Meningitis
Fungal meningitis is an exceptionally rare condition and typically does not spread from person to person. The infection generally occurs when fungal spores enter the bloodstream or spinal fluid, as seen in this outbreak. Common symptoms include:
- Fever
- Severe headaches
- Stiff neck
- Nausea and vomiting
- Dizziness
- Sensitivity to light
- Numbness or tingling
If left untreated, fungal meningitis can lead to life-threatening complications such as brain damage or stroke. Early detection and treatment are critical to managing the disease effectively.
Response and Lessons Learned
The fungal meningitis outbreak of 2012 sparked a national conversation about the safety and regulation of compounding pharmacies in the United States. The NECC, the company responsible for producing the contaminated medication, faced legal and regulatory action for its failure to maintain sterile production conditions.
In response, stricter regulations were implemented to oversee compounding pharmacies, ensuring that they adhere to the highest standards of sterility and quality control. The incident also underscored the importance of rapid reporting and containment measures to prevent the spread of rare but deadly infections.
Preventive Measures
While fungal meningitis remains rare, individuals who undergo medical procedures involving injections should take precautions:
- Ensure that medications are sourced from reputable, regulated suppliers.
- Discuss the risks of infections with healthcare providers, particularly for invasive procedures.
- Be vigilant for early symptoms of meningitis after receiving injections or other medical treatments and seek immediate medical attention if symptoms develop.
This outbreak serves as a reminder of the critical role that healthcare providers, pharmaceutical companies, and regulators play in ensuring patient safety. By learning from such incidents, the healthcare industry can better safeguard against similar tragedies in the future.