Summary
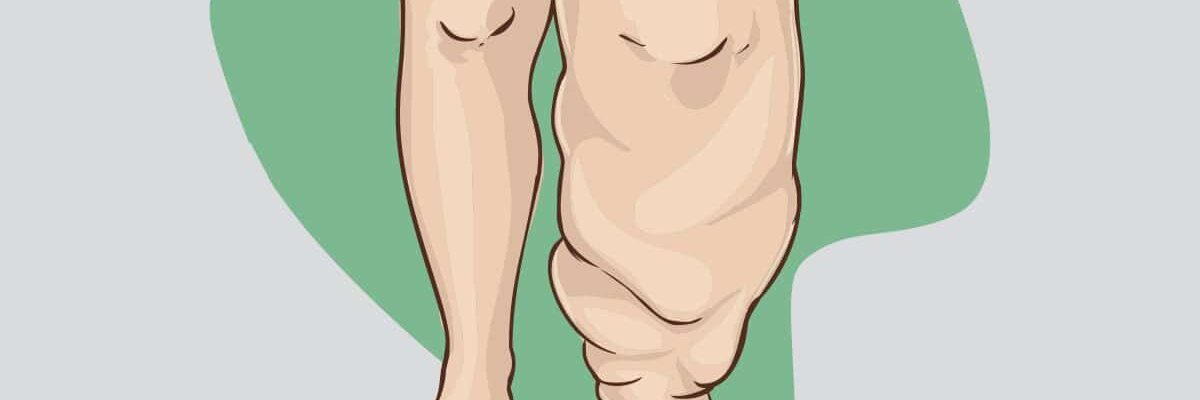
Elephantiasis is a tropical disease, commonly found in regions with warm climates, and is medically known as lymphatic filariasis. In this condition, individuals often experience extreme swelling of the limbs, particularly the legs, giving the appearance of elephant-like feet.
Elephantiasis occurs when a person is bitten by a mosquito carrying larvae of parasitic worms, typically roundworms. Although various types of roundworms can cause the disease, about 90% of cases are due to Wuchereria bancrofti. When the larvae enter the human body, they migrate to the lymphatic system, where they grow and block lymphatic vessels, leading to fluid accumulation and tissue swelling.
To treat elephantiasis, doctors may prescribe antiparasitic medications to eliminate the worms and their larvae. Additional medications may be given to relieve symptoms, such as itching, body pain, fever, and infections, which commonly accompany the condition. Effective treatment can prevent the progression of the disease, though early intervention is critical for better outcomes.
Table of Contents
Symptoms of Elephantiasis

Individuals with elephantiasis may not initially show visible symptoms, such as swollen limbs, but the disease can still affect their lymphatic system and even damage organs like the kidneys. This internal damage can weaken the immune system, leaving the body more susceptible to other infections and illnesses.
If symptoms do develop, they may include the following:
- Swelling or enlargement of the limbs. The legs and arms can become significantly swollen due to fluid buildup, often appearing disproportionate.
- Hardening and thickening of swollen areas. The affected skin may become rough, thick, and stiff, a condition known as lymphedema.
- Enlargement of the scrotum in men. Men may experience swelling of the scrotum (hydrocele), which can be painful and disabling.
- Enlargement of the breasts in women. Women may notice significant swelling in the breasts, which can also become uncomfortable and affect mobility.
- Sores and skin infections. The swollen skin is more prone to developing sores and secondary bacterial infections due to its compromised state.
- Fever. Periodic fevers can occur as the body attempts to fight off infections related to lymphatic damage.
- Muscle chills. Chills and muscle shivering may accompany fever and infection.
- Darkening of affected areas. The skin on swollen limbs may take on a darker, uneven appearance due to tissue damage.
- Body weakness. General fatigue and weakness are common as the immune system is taxed.
- Nodules on affected areas. Small lumps or nodules may form in swollen areas due to tissue and lymphatic changes.
These symptoms can significantly impact the quality of life, causing both physical discomfort and psychological distress. Early medical intervention is essential to manage symptoms, prevent infections, and improve the patient’s overall health and resilience.
Types of Elephantiasis
Elephantiasis, or lymphatic filariasis, can present in different forms depending on the underlying cause. Here are the main types:
- Lymphatic Filariasis. This is the most common form of elephantiasis, caused by parasitic roundworms such as Wuchereria bancrofti, Brugia malayi, and Brugia timori. These worms are transmitted to humans through mosquito bites and lodge in the lymphatic system, leading to swelling and tissue hardening. Symptoms may take years to develop, and the disease progresses with repeated exposure and infection, causing significant limb swelling, genital enlargement, and skin thickening.
- Non-Filarial Elephantiasis (Podoconiosis). Unlike lymphatic filariasis, non-filarial elephantiasis is not caused by parasitic worms but by long-term exposure to irritant minerals in volcanic soil. This condition is more common in high-altitude areas of tropical regions where people frequently walk barefoot. The irritant minerals enter the skin and cause inflammation of the lymphatic vessels, leading to swelling, particularly in the legs and feet. Podoconiosis is preventable through proper footwear and improved hygiene practices.
- Genetic or Congenital Elephantiasis. Some cases of elephantiasis are genetic, arising from inherited conditions that impair lymphatic function. Primary lymphedema, for example, is a genetic disorder where the lymphatic vessels do not develop properly, causing chronic swelling and thickened skin. This type can appear in childhood or later in life, depending on the severity of the genetic condition, and often requires lifelong management.
Each type of elephantiasis requires specific treatment and management approaches. While lymphatic filariasis is treated with antiparasitic medications, non-filarial elephantiasis focuses on reducing exposure to environmental irritants. Genetic forms of elephantiasis often rely on physical therapy, compression, and surgery to manage symptoms and improve quality of life.
Diagnostic Procedures for Elephantiasis
Early diagnosis of elephantiasis is essential for managing symptoms and preventing progression. Here are the primary diagnostic procedures used to detect elephantiasis:
- Physical examination. A healthcare provider will typically start with a physical exam, assessing the patient’s symptoms such as swelling, skin thickening, and areas affected. A detailed medical history can also help determine if the patient has been exposed to risk factors associated with elephantiasis.
- Blood tests. Blood tests are essential for diagnosing lymphatic filariasis, the most common cause of elephantiasis:
- Microscopic blood smear. A blood sample is examined under a microscope to detect the presence of Wuchereria bancrofti, Brugia malayi, or Brugia timori larvae. For best results, the sample is often collected at night when the parasites are most active in the blood.
- Antigen detection test. This test identifies specific proteins from the parasite in the blood and can provide a quicker diagnosis than microscopic examination.
- Polymerase Chain Reaction (PCR) test. PCR testing detects the genetic material of the parasite, providing a highly accurate diagnosis. However, this test is usually done in specialized laboratories.
- Ultrasound imaging. In some cases, ultrasound can be used to visualize adult worms in the lymphatic system, particularly in the scrotal area for men. This imaging technique can help confirm the presence of worms and assess the extent of lymphatic damage.
- Lymphoscintigraphy. This imaging test tracks the flow of lymphatic fluid through the body using a small, safe amount of radioactive tracer. It helps identify blockages or abnormalities in the lymphatic system, which are common in advanced cases of elephantiasis.
- Urine tests. In cases where the genitourinary tract is affected, urine tests may be used to detect proteins and other markers indicative of lymphatic filariasis, particularly in men with hydrocele (swelling of the scrotum).
Accurate diagnosis is crucial for effective treatment, as early detection allows for antiparasitic medications and symptom management that can prevent further damage to the lymphatic system.
Complications of Untreated Elephantiasis
If left untreated, elephantiasis can lead to severe and debilitating complications, often resulting in lifelong physical and social challenges. Here are some of the major complications of untreated elephantiasis:
- Chronic swelling and disfigurement. The most visible effect of untreated elephantiasis is extreme swelling in the affected areas, commonly the legs, arms, genitals, or breasts. This swelling can lead to significant disfigurement, limiting mobility and daily function, and increasing the risk of other health issues.
- Frequent bacterial infections. Chronic swelling makes the skin more prone to cracks and sores, providing entry points for bacteria. This can lead to frequent bacterial infections, such as cellulitis and lymphangitis, which can worsen swelling and inflammation and further damage the lymphatic vessels.
- Thickening and hardening of the skin (hyperkeratosis). Over time, untreated elephantiasis causes the skin to become thick, rough, and scaly. This condition, known as hyperkeratosis, is often painful and increases the likelihood of ulcers and other skin complications.
- Mobility impairment. Severe swelling and thickening of the skin can severely limit movement in the affected limbs, leading to reduced mobility, muscle atrophy, and a decline in physical health. This loss of mobility can also increase dependence on others for basic tasks.
- Social and psychological impact. The visible disfigurement and limitations caused by elephantiasis often lead to social stigma and discrimination. Many patients experience psychological distress, including anxiety, depression, and social isolation, which can severely impact their quality of life.
- Increased risk of kidney damage. Chronic lymphatic damage caused by filarial parasites can sometimes extend to the kidneys, leading to proteinuria (excess protein in the urine) and eventually kidney failure if untreated.
- Secondary lymphedema complications. Prolonged lymphatic obstruction can lead to secondary lymphedema, with further accumulation of fluid and increased pressure on tissues, compounding pain, and limiting function in the affected area.
Untreated elephantiasis can profoundly affect a person’s physical, mental, and social well-being. Early intervention, proper treatment, and ongoing care are essential to minimize these complications and improve the patient’s quality of life.
Causes of Elephantiasis
Elephantiasis is caused by parasitic roundworms. A person may contract this disease when bitten by a mosquito carrying the larvae of Wuchereria bancrofti, Brugia malayi, or Brugia timori. Once these larvae enter the human body, they travel to the lymphatic system, where they grow and develop, leading to the onset of symptoms over time.
The lymphatic system comprises lymph nodes and vessels, which play a crucial role in removing waste, toxins, and excess fluids from the body. However, when these pathways become blocked by parasitic larvae or the mature worms they develop into, lymphatic fluid begins to accumulate. This fluid buildup causes significant swelling in various parts of the body, most commonly the legs, but it can also affect the arms, genitals, and other areas.
As the worms grow and multiply within the lymphatic system, they continue to disrupt fluid circulation, leading to chronic inflammation and tissue hardening. This prolonged obstruction of the lymphatic vessels results in the characteristic swelling and skin thickening seen in elephantiasis. Early treatment and preventive measures are essential to reduce the spread of infection and minimize damage to the lymphatic system.
Prevention of Elephantiasis

According to the World Health Organization (WHO), approximately 120 million people are affected by elephantiasis, especially those living in tropical climates. To prevent the spread of this disease, the following measures are recommended:
- Keep the home and surroundings clean. Maintaining a clean and well-ventilated home discourages mosquitoes, which tend to hide in dark and cluttered areas. Dispose of any items or trash that could collect stagnant water, as this serves as a breeding ground for mosquitoes.
- Use a mosquito net while sleeping. Ensure the edges of the mosquito net are securely tucked under the bed to prevent mosquitoes from entering. Mosquito nets offer a reliable barrier, especially in areas with high mosquito populations.
- Apply mosquito repellent. Various over-the-counter mosquito repellents are available in pharmacies. These repellents, often in lotion or cream form, are easy to apply to the skin. There are formulas suitable for both children and adults to protect against mosquito bites.
- Wear long clothing. Covering exposed skin helps reduce the chances of mosquito bites. Opt for long-sleeved shirts, pajamas, or pants, especially during peak mosquito activity times.
- Avoid travel to affected areas. Not all tropical regions are equally risky, but it’s wise to avoid traveling to areas with known active cases of elephantiasis or high mosquito activity. If planning a trip to a tropical country, check for any health advisories related to mosquito-borne diseases.
Implementing these preventive strategies significantly reduces the risk of mosquito bites, thereby lowering the chances of contracting diseases like elephantiasis. Mosquito control and personal protective measures are essential, particularly in areas where the disease is prevalent.
Risk Factors for Elephantiasis

Elephantiasis can potentially affect anyone. However, certain factors increase the likelihood of contracting this condition:
- Living in tropical regions. Areas with warm, humid climates, such as Africa, India, South America, and Southeast Asia, are prone to high mosquito populations. These tropical regions create ideal breeding conditions for mosquitoes, including the Aedes and Culex species that can transmit elephantiasis-causing parasites.
- Frequent mosquito bites. Contracting elephantiasis usually requires repeated bites from infected mosquitoes. A single mosquito bite is unlikely to transmit enough larvae to cause the disease. Prolonged exposure to infected mosquitoes, however, increases the chance of parasitic larvae entering the lymphatic system and causing infection.
- Living in unsanitary conditions. Areas with poor sanitation or stagnant water are common breeding grounds for mosquitoes. In communities with limited waste management and drainage systems, mosquitoes can multiply more easily, raising the risk of infection for residents.
Understanding these risk factors highlights the importance of preventive measures, especially in areas with high mosquito activity. Good sanitation, mosquito control, and personal protective strategies are essential to reducing the risk of elephantiasis and other mosquito-borne diseases.
Elephantiasis FAQs
Here are answers to some common questions about elephantiasis, covering its causes, symptoms, prevention, and treatment.
- What is elephantiasis?
Elephantiasis, medically known as lymphatic filariasis, is a disease that causes extreme swelling and thickening of the skin, particularly in the legs, arms, and genitals. This swelling is due to an infection by parasitic worms, usually transmitted through mosquito bites. - How is elephantiasis transmitted?
Elephantiasis is typically transmitted by mosquitoes that carry the larvae of parasitic worms, including Wuchereria bancrofti, Brugia malayi, and Brugia timori. When an infected mosquito bites a person, the larvae enter the bloodstream and settle in the lymphatic system, where they grow and cause blockages over time. - What are the symptoms of elephantiasis?
Symptoms include severe swelling of the limbs, genitals, or breasts; thickened and hardened skin; recurrent bacterial infections; pain; and limited mobility. In its early stages, symptoms may be mild or unnoticeable, but they progress with time and repeated exposure to infection. - Who is at higher risk of contracting elephantiasis?
People living in tropical and subtropical regions, particularly in areas with poor sanitation and high mosquito populations, are at greater risk. These regions include parts of Africa, Southeast Asia, India, and South America. - Is elephantiasis curable?
While there is no complete cure for the physical effects of elephantiasis, early treatment with antiparasitic medications can help eliminate the worms and prevent further lymphatic damage. Treatment of symptoms can improve quality of life and manage complications. - How is elephantiasis treated?
Treatment typically includes antiparasitic medications to kill the worms, antibiotics to prevent secondary infections, and sometimes physical therapy to improve circulation. In advanced cases, surgery may be needed to remove excess tissue or relieve lymphatic obstruction. - Can elephantiasis be prevented?
Yes, prevention includes avoiding mosquito bites by using insect repellents, sleeping under mosquito nets, and wearing protective clothing. In high-risk areas, mass drug administration programs provide antiparasitic medications to reduce transmission rates in the community. - Can elephantiasis be spread from person to person?
No, elephantiasis is not contagious and cannot be spread through person-to-person contact. The disease requires a mosquito to transmit the parasite from one person to another. - What should I do if I suspect I have elephantiasis?
If you suspect you have elephantiasis, consult a healthcare provider. Early diagnosis through blood tests and appropriate treatment can help manage symptoms and prevent complications. - How does elephantiasis impact quality of life?
Elephantiasis can significantly affect quality of life due to physical limitations, social stigma, and psychological distress. Treatment and supportive care are essential to help patients maintain mobility, manage pain, and cope with the emotional impact of the disease.