Summary
Trichomoniasis is one of the most common sexually transmitted infections (STIs), and while it can affect anyone, the symptoms primarily manifest in specific parts of the reproductive system in both men and women.
This infection is caused by a parasitic protozoan called Trichomonas vaginalis. In men, this organism typically resides inside the urethra, while in women, it can be found in various parts of the reproductive system, including the vagina and cervix.
The symptoms of trichomoniasis can resemble those of other STIs. In women, they include pelvic pain, a foul-smelling discharge that may sometimes be tinged with blood, and pain during sexual intercourse. However, many people do not notice these symptoms in the early stages, which can lead to delayed diagnosis.
Trichomoniasis is treated with antibiotics and other medications prescribed by a healthcare professional.
Now, let’s explore how trichomoniasis is discovered, its causes, and how it can be prevented and treated effectively.
Table of Contents
Symptoms of Trichomoniasis
Trichomoniasis can be difficult to detect because many men and women infected with the disease do not show any symptoms in the early stages. This makes it easy for the infection to go unnoticed, often leading to its spread and delayed treatment.
In women, the most common symptoms of trichomoniasis include:
- Foul-smelling vaginal discharge. The discharge may be yellow, green, or white in color and is often accompanied by a strong odor.
- Redness and swelling of the genital area. Inflammation of the vagina (vaginitis) may occur, causing discomfort.
- Itching and burning sensations. Intense itching and burning in the genital area are common, leading to significant discomfort.
- Pain during urination or sexual intercourse. Women may experience a stinging or burning sensation while urinating or pain during sexual activity, which can signal an infection.
In men, symptoms of trichomoniasis are less common, but when they do appear, they may include:
- Itching inside the urethra. Men may experience irritation or itching inside the penis, which can cause discomfort.
- Burning sensation during urination or ejaculation. Painful urination or ejaculation is a key symptom in men who show signs of infection.
- Foul-smelling discharge from the penis. Men may notice an unusual discharge with an unpleasant odor.
Although anyone can contract trichomoniasis, certain individuals have a higher risk of getting infected. Understanding these symptoms and seeking timely treatment is essential for preventing further complications.
Types of Trichomoniasis
There is only one type of trichomoniasis, but its characteristics vary between men and women.
In Men
In men, the parasitic organism Trichomonas vaginalis typically resides in the urethra—the tube that connects the bladder to the opening of the penis and carries both urine and semen. Because of this, symptoms are usually localized to the urethra.
However, it’s important to note that most men with trichomoniasis do not show symptoms, or the symptoms are very mild. This makes it difficult for women to know if their male partner is infected, as the condition often goes unnoticed in men.
When left untreated, trichomoniasis in men can lead to several complications, including:
- Infertility. The infection can affect sperm production and motility, potentially leading to infertility.
- Prostatitis. Inflammation of the prostate gland can result from trichomoniasis, causing discomfort and urinary issues.
- Epididymitis. The infection can spread to the epididymis, the tube that carries sperm, leading to painful swelling and inflammation.
- Orchitis. Trichomoniasis can cause orchitis, or inflammation of one or both testicles, leading to pain and swelling.
- Increased susceptibility to HIV. Having trichomoniasis can make men more susceptible to contracting HIV due to the damage it causes to the urethra and genital tissues.
- Risk of prostate cancer. Some studies suggest that chronic trichomoniasis infections may increase the risk of developing prostate cancer, though more research is needed to confirm this link.
In Women
In women, trichomoniasis symptoms tend to be more apparent and can range from mild to severe. The infection primarily affects the vaginal area, but it can lead to more serious conditions like pelvic inflammatory disease (PID). Women with trichomoniasis may experience vaginal discharge that is foul-smelling, frothy, and sometimes blood-tinged.
Other symptoms in women include:
- Pelvic pain. Pain in the lower abdomen or pelvis is common, especially if the infection progresses or spreads to other parts of the reproductive system.
- Itching and burning. The vaginal area often becomes irritated, causing itching and a burning sensation.
- Pain during intercourse. Women with trichomoniasis frequently experience discomfort or pain during sexual activity due to vaginal inflammation.
Understanding the differences in how trichomoniasis affects men and women can help with early diagnosis and effective treatment, preventing the complications associated with the infection.
Diagnostic Procedures for Trichomoniasis
Diagnosing trichomoniasis involves a combination of physical examination, laboratory tests, and in some cases, advanced diagnostic techniques to detect the presence of the Trichomonas vaginalis parasite. Here are the common diagnostic procedures used by healthcare providers:
- Physical examination. A doctor will first conduct a thorough physical examination, especially if symptoms such as vaginal discharge, itching, or pain are present. In women, this usually involves a pelvic exam to check for signs of infection in the reproductive organs, including any abnormal discharge or vaginal inflammation.
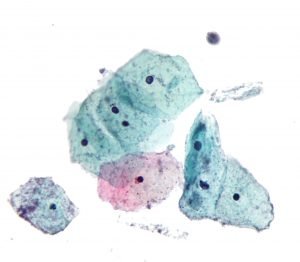
- Microscopic examination of discharge. A sample of vaginal or urethral discharge can be taken and examined under a microscope to detect the presence of Trichomonas vaginalis. This is one of the most direct and quick methods of diagnosis. The parasite is often visible in a wet mount preparation, where the discharge is placed on a slide with a saline solution and observed for the motile (moving) trichomonads.
- Nucleic acid amplification test (NAAT). NAAT is one of the most accurate tests for diagnosing trichomoniasis. It detects the DNA of the Trichomonas vaginalis parasite. This test can be done using samples of vaginal or urethral discharge, urine, or cervical swabs. Due to its high sensitivity, NAAT is commonly used in modern STI screening.
- Rapid antigen tests. Rapid antigen testing is another method for diagnosing trichomoniasis, where specific proteins (antigens) from the parasite are detected in vaginal or urethral samples. These tests offer quick results but are slightly less accurate than NAAT.
- Urine test. In both men and women, a urine sample can be tested for the presence of Trichomonas vaginalis. This test is often used for men who may not exhibit symptoms, as it helps identify the infection in cases where physical symptoms are absent.
- Culture test. A culture test involves growing the parasite in a special medium to detect its presence. While not as commonly used due to more advanced options like NAAT, this test can still be useful in some clinical settings.
Early detection and treatment of trichomoniasis are important to prevent complications and the spread of the infection. If diagnosed, trichomoniasis is typically treated with antibiotics, such as metronidazole or tinidazole. Regular testing, especially for sexually active individuals, helps ensure prompt identification and treatment of sexually transmitted infections (STIs).
Complications of Untreated Trichomoniasis
If trichomoniasis is left untreated, it can lead to several serious complications, some of which can affect long-term health. Here are the main complications associated with untreated trichomoniasis:
- Increased risk of HIV infection. Untreated trichomoniasis causes genital inflammation, which makes it easier for the HIV virus to enter the body if exposed. It also increases the likelihood of transmitting HIV to sexual partners.
- Pelvic inflammatory disease (PID) in women. Women with untreated trichomoniasis are at risk of developing PID, which is an infection of the upper reproductive organs. PID can cause chronic pelvic pain, damage to the fallopian tubes, and lead to infertility or ectopic pregnancy.
- Pregnancy complications. Pregnant women with trichomoniasis are at a higher risk of complications such as premature birth, low birth weight, and premature rupture of membranes. There is also a chance of transmitting the infection to the baby during delivery.
- Prostatitis in men. In men, untreated trichomoniasis can lead to prostatitis, which is an inflammation of the prostate gland. This can cause pain, difficulty urinating, and in some cases, fertility issues.
- Epididymitis. Men may also experience epididymitis, which is the inflammation of the tube that carries sperm. This condition can cause swelling, pain, and may lead to infertility if not treated.
- Ongoing transmission to sexual partners. Trichomoniasis can be transmitted even when no symptoms are present. Untreated individuals can unknowingly spread the infection to their sexual partners, increasing the likelihood of further complications for others.
- Higher risk of other STIs. Trichomoniasis weakens the body’s defenses, making individuals more susceptible to other sexually transmitted infections (STIs), including gonorrhea, chlamydia, and syphilis.
Treating trichomoniasis early with antibiotics is crucial to prevent these complications. Regular STI testing and safe sex practices help reduce the risk of contracting and spreading trichomoniasis and other infections.
Causes of Trichomoniasis
Trichomoniasis is caused by a parasitic protozoan known as Trichomonas vaginalis, which is primarily transmitted through sexual contact with an infected person. The parasite can be passed between sexual partners, even if the infected individual does not show any symptoms.
In women, the most commonly affected areas are the vagina, vulva, cervix, and urethra. The parasite thrives in these parts of the reproductive system, leading to discomfort and infection.
In men, Trichomonas vaginalis typically infects the urethra, the tube inside the penis that carries urine and semen. The infection can cause irritation and other mild symptoms, though many men may not experience any noticeable signs of infection.
Here’s how the parasite spreads during sexual contact:
- Male-to-female transmission. During vaginal intercourse, the parasite can move from an infected man’s penis to the woman’s vagina, causing infection.
- Female-to-male transmission. The parasite can also spread from the infected woman’s vagina to the man’s penis during sexual contact, leading to urethral infection.
- Female-to-female transmission. Trichomoniasis can be transmitted between women through genital contact during sexual activity. The parasite can spread from one woman’s vagina to another’s, making it a concern for women who have sex with women as well.
It’s important to note that even if an infected person does not display any symptoms, they can still pass the infection on to their sexual partners. This silent transmission is one reason why regular testing is crucial, especially for sexually active individuals.
Now that we understand the causes, let’s look at the symptoms and how to recognize trichomoniasis in its early stages.
Prevention of Trichomoniasis

Preventing trichomoniasis is relatively simple. Like other sexually transmitted infections (STIs), trichomoniasis can be avoided by abstaining from any type of sexual activity. However, for those who are sexually active, the following steps can help reduce the risk of contracting trichomoniasis:
- Engage in a long-term relationship with one partner. Limiting sexual activity to one mutually faithful partner who has tested negative for trichomoniasis and other STIs can significantly lower the risk of infection.
- Have only one sexual partner at a time. Maintaining monogamy during the course of a relationship helps minimize exposure to potential infections, including trichomoniasis.
- Ensure your partner is tested. Before becoming sexually active with a new partner, both individuals should get tested for trichomoniasis and other STIs. This ensures that any infections are detected and treated early, preventing transmission.
- Use latex condoms correctly and consistently. Using latex condoms every time you have sex can greatly reduce the risk of contracting trichomoniasis. Condoms act as a barrier, preventing the parasite from being transmitted between partners.
- Communicate openly about sexual health. Having honest conversations with your partner about STIs is crucial when entering a new relationship. Knowing your partner’s sexual health status helps make informed decisions about your sexual relationship and reduces the risk of infection.
- Consult healthcare professionals. If you have questions or concerns about trichomoniasis or other sexually transmitted infections, seek advice from a healthcare provider or an STI specialist. Regular checkups and open discussions with medical experts can help ensure you’re taking the right precautions to protect your health.
By following these preventive measures, individuals can significantly reduce the chances of contracting trichomoniasis and other sexually transmitted infections. Safe sexual practices and regular testing are key to maintaining sexual health and preventing the spread of infections.
Risk Factors for Trichomoniasis
Several factors can increase the likelihood of contracting trichomoniasis. These risk factors include:
- Engaging in unprotected sex. Having sexual intercourse without using protection, such as condoms, significantly raises the risk of contracting trichomoniasis. Condoms act as a barrier that helps prevent the transmission of the Trichomonas vaginalis parasite.
- Having multiple sexual partners. The more sexual partners you have, the higher the chances of being exposed to an infected individual. This increases the risk of contracting trichomoniasis and other sexually transmitted infections (STIs).
- History of sexually transmitted infections (STIs). Individuals who have previously contracted STIs are at a greater risk of contracting trichomoniasis, as they may already have weakened defenses or compromised genital health.
- Previous infection with trichomoniasis. If you have had trichomoniasis before, you are more likely to contract it again, especially if preventive measures are not followed. Reinfection is possible even after successful treatment.
Now that we’ve covered the risk factors, let’s look into the complications that trichomoniasis can cause if left untreated. Understanding these risks can help in preventing long-term health issues.
Trichomoniasis FAQs
Here are some frequently asked questions about trichomoniasis, providing essential information on symptoms, transmission, and treatment:
- What is trichomoniasis?
Trichomoniasis is a common sexually transmitted infection (STI) caused by a parasitic protozoan called Trichomonas vaginalis. It primarily affects the genital area in both men and women. - How is trichomoniasis transmitted?
Trichomoniasis is transmitted through sexual contact with an infected person, including vaginal, anal, and oral sex. The parasite spreads through the exchange of bodily fluids during sexual activity. - What are the symptoms of trichomoniasis?
Symptoms in women may include foul-smelling vaginal discharge, itching, redness, and pain during urination or intercourse. Men often have milder symptoms, such as irritation inside the penis, burning during urination or ejaculation, and penile discharge. However, many individuals with trichomoniasis may not show any symptoms at all. - Can trichomoniasis go away on its own?
No, trichomoniasis does not go away on its own. It requires treatment with antibiotics, usually metronidazole or tinidazole. If left untreated, the infection can persist and lead to complications. - How is trichomoniasis diagnosed?
Trichomoniasis is diagnosed through a physical exam, a microscopic examination of vaginal or urethral discharge, or more advanced tests like a nucleic acid amplification test (NAAT). A urine test may also be used to detect the parasite. - How is trichomoniasis treated?
Trichomoniasis is treated with antibiotics, typically metronidazole or tinidazole. Both partners should be treated to prevent reinfection, even if one partner is not showing symptoms. It’s important to complete the full course of antibiotics to ensure the infection is fully cleared. - Can I get trichomoniasis again after being treated?
Yes, reinfection is possible. Even after successful treatment, you can contract trichomoniasis again if exposed to an infected partner. To avoid reinfection, it’s crucial to practice safe sex and ensure that all sexual partners are treated. - How can trichomoniasis be prevented?
Trichomoniasis can be prevented by using condoms during sexual intercourse, limiting the number of sexual partners, and getting regular STI screenings. Open communication with your partner about sexual health is also key to prevention. - Can trichomoniasis cause complications if left untreated?
Yes, untreated trichomoniasis can lead to serious complications, especially in women. It can cause pelvic inflammatory disease (PID), increase the risk of contracting or spreading HIV, and lead to complications during pregnancy, such as premature birth or low birth weight. - Should I get tested for trichomoniasis if I don’t have symptoms?
Yes, even if you don’t have symptoms, it’s a good idea to get tested if you’re sexually active, especially if you have multiple partners or suspect that your partner may be infected. Many people with trichomoniasis don’t experience symptoms, but they can still spread the infection.
Understanding trichomoniasis and how to prevent and treat it is essential for maintaining sexual health and preventing the spread of sexually transmitted infections. If you suspect that you have trichomoniasis or have been exposed, consult a healthcare provider for testing and treatment.