Summary
Tetanus, also known in English as “lockjaw,” is named for one of its early symptoms: stiffness in the jaw and neck. It is a bacterial infection caused by Clostridium tetani, typically contracted through open wounds or cuts that become exposed to the bacteria. These bacteria are often found in soil, dust, and animal waste, and they produce a toxin that affects the nervous system.
When a person contracts tetanus, symptoms usually include stiffness in the neck, jaw, and other muscles. The infection can also cause difficulty swallowing and involuntary muscle contractions throughout the body. In addition, patients may develop a fever as the body responds to the infection.
If left untreated, tetanus can be life-threatening, as the toxin can cause severe muscle spasms and respiratory problems. However, with prompt medical treatment, there is a good chance of recovery. Doctors typically administer treatments like tetanus antitoxin to neutralize the toxin, antibiotics to fight the infection, tetanus toxoid to boost immunity, and muscle relaxants to ease spasms. In severe cases, a ventilator may be required to support breathing. Early intervention is critical to reduce complications and aid in a smoother recovery.
Table of Contents
Symptoms of Tetanus
In the early stages of tetanus, a patient may experience the following symptoms:
- Stiffness in the neck, jaw, and muscles. This stiffness often begins in the jaw, making it difficult to open the mouth fully, hence the term “lockjaw.”
- Involuntary facial muscle contractions or grimacing. Patients may have an uncontrollable muscle spasm in the mouth area, causing a forced smile or grimace.
- Difficulty swallowing. Muscle rigidity in the throat and neck can lead to swallowing issues, which may progress as the infection worsens.
- Fever. A slight fever may occur as the body tries to fight the infection.
- Excessive sweating. The infection and toxin release can trigger excessive sweating as part of the body’s response.
- Involuntary muscle spasms. Muscle contractions throughout the body may occur without warning and are often painful.
- Muscle pain. Due to continuous muscle stiffness and spasms, patients may experience significant muscle pain.
Tetanus symptoms typically appear around 10 days after exposure to Clostridium tetani, although the incubation period can range from a few days to several weeks. Early recognition and prompt treatment are essential to manage symptoms and prevent severe complications.
Types of Tetanus
Tetanus has four main types, each varying in severity and affected areas of the body. These types include:
- Generalized tetanus. This is the most common and severe form of tetanus, affecting the entire body. Initial symptoms typically include stiffness in the face and neck, along with difficulty swallowing. As it progresses, patients may experience tonic spasms, such as arching of the back (opisthotonos) due to severe muscle contractions. Generalized tetanus can lead to life-threatening complications if not treated promptly.
- Neonatal tetanus. This form of tetanus affects newborns and is often acquired when non-sterile instruments are used to cut the umbilical cord. The risk is significantly reduced if the mother has received a tetanus vaccination during pregnancy, which helps protect the infant through passive immunity. Neonatal tetanus can cause rigidity and spasms throughout the infant’s body and is life-threatening without immediate treatment.
- Localized tetanus. This rare form occurs when the tetanus infection remains confined to the area near the wound. It typically affects individuals who have received partial immunity from vaccination but still experience mild symptoms at the injury site. Although less severe, localized tetanus can sometimes progress to generalized tetanus if untreated.
- Cerebral tetanus. Another rare form, cerebral tetanus, usually occurs due to a head injury or brain trauma, allowing the bacteria to affect cranial nerves. It can also develop if middle ear infections (otitis media) are left untreated. Symptoms may include facial muscle spasms, difficulty speaking, and cranial nerve involvement, and it can be life-threatening if not managed properly.
Understanding these types of tetanus helps in identifying symptoms early and administering the correct treatment. Prompt medical care and vaccination can reduce the severity and risk of complications for each form of tetanus.
Diagnostic Procedures for Tetanus
Diagnosing tetanus can be challenging because it relies primarily on clinical symptoms rather than specific lab tests. Early diagnosis is critical to prevent complications and begin treatment promptly. Here are the primary diagnostic procedures used to identify tetanus:
- Physical examination. The diagnosis of tetanus often starts with a physical exam to assess muscle stiffness and spasms. A doctor will check for common symptoms, such as jaw stiffness (lockjaw), muscle rigidity, and difficulty swallowing. These symptoms, particularly if there has been a recent injury or wound, strongly indicate tetanus.
- Medical history review. A doctor will ask about recent injuries, puncture wounds, or other cuts, especially if the wound was exposed to dirt, soil, or unsterilized objects. They may also review the patient’s vaccination history to assess immunity to tetanus.
- Observation of specific muscle responses. In some cases, a doctor may observe muscle reactions to external stimuli, such as touch or noise, which may trigger spasms in a person with tetanus. This response is an indicator of tetanus, as other infections rarely cause similar reflexes.
- Ruling out other conditions. Because tetanus symptoms can resemble other neurological conditions, a doctor may perform tests to exclude conditions like meningitis, rabies, or drug-induced muscle rigidity. Blood tests, imaging scans, or spinal fluid analysis may be ordered to rule out these conditions.
While there is no definitive laboratory test to confirm tetanus, careful evaluation of symptoms and recent history can lead to a reliable diagnosis. Early identification is crucial, as tetanus requires immediate treatment to reduce the severity of symptoms and prevent complications.
Complications of Untreated Tetanus
If tetanus is left untreated, the bacterial toxin released by Clostridium tetani can lead to severe and potentially life-threatening complications. Early treatment is essential to avoid these complications, which can affect multiple organ systems and overall body function. Here are some of the primary complications of untreated tetanus:
- Respiratory failure. Tetanus causes severe muscle stiffness and spasms that can affect the respiratory muscles, making it difficult to breathe. Without treatment, this can lead to respiratory failure, which is life-threatening and requires immediate intervention, often with mechanical ventilation.
- Aspiration pneumonia. Difficulty swallowing and involuntary muscle spasms can cause food, saliva, or stomach contents to enter the lungs, leading to aspiration pneumonia. This lung infection can be severe and requires intensive antibiotic treatment.
- Fractures and muscle tears. Severe, forceful muscle spasms can lead to bone fractures or muscle tears. In particular, spine and rib fractures are common in patients with intense spasms, which can cause additional pain and complicate recovery.
- Autonomic dysfunction. Tetanus can disrupt the autonomic nervous system, leading to symptoms like rapid heart rate, high blood pressure, and sweating. This dysfunction can be difficult to control and increases the risk of heart complications.
- Sepsis. The presence of Clostridium tetani in the body and the resulting infections in wounds can lead to sepsis, a life-threatening condition where the body’s response to infection triggers widespread inflammation. Sepsis can result in multiple organ failure if untreated.
- Death. Due to respiratory complications, autonomic instability, and sepsis, untreated tetanus carries a high risk of death. The mortality rate of untreated tetanus remains significant, especially in severe cases and without access to immediate medical care.
The complications of untreated tetanus emphasize the need for prompt medical intervention, as well as the importance of vaccination to prevent infection in the first place. Regular tetanus boosters, wound care, and early medical treatment for any suspected infection are essential steps to protect against these serious outcomes.
Causes of Tetanus
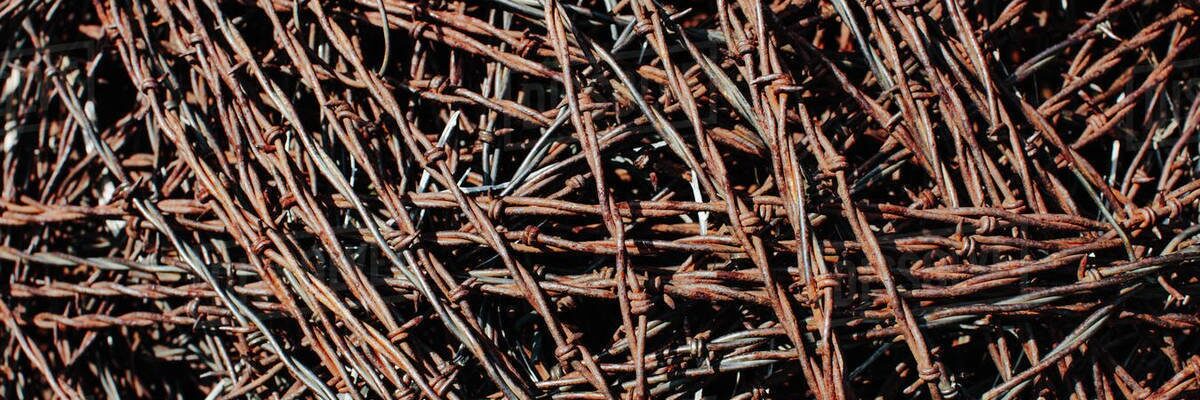
 Image Source: commons.wikimedia.org
Image Source: commons.wikimedia.org
Tetanus is directly caused by the bacterium Clostridium tetani, which releases a potent neurotoxin called tetanospasmin upon entering the body. This bacterium is found primarily in soil, dust, and animal feces and can survive for long periods as spores. When these spores enter the body through specific types of injuries, they activate, multiply, and release the toxin, leading to the symptoms of tetanus.
Here are the direct causes of tetanus:
- Contamination of open wounds by Clostridium tetani spores. The primary cause of tetanus is when Clostridium tetani spores enter deep puncture wounds or cuts that come into contact with contaminated soil, dust, or feces. Examples include stepping on a rusty nail or a cut that is exposed to the ground, allowing spores to enter and create an environment for the bacteria to grow.
- Exposure through non-sterile medical or body modification procedures. Tetanus can occur if Clostridium tetani spores enter the body during procedures like ear piercing, tattooing, or injection with non-sterile needles. Non-sterile equipment or environments create a direct route for bacterial spores to enter the bloodstream.
- Introduction of bacteria through severe burns or damaged tissue. Burn injuries or crushed tissue provide the ideal anaerobic (low-oxygen) environment for Clostridium tetani to thrive, especially if the wound is not properly cleaned and debrided.
These direct causes emphasize the importance of proper wound cleaning, hygiene, and sterile practices to prevent Clostridium tetani spores from entering the body and producing the toxin that leads to tetanus. Regular vaccination also provides crucial protection against this bacteria’s severe effects.
Prevention of Tetanus
 Image Source: www.medicaleconomics.com
Image Source: www.medicaleconomics.com
Doctors advise that tetanus should never be taken lightly, as it is a life-threatening condition. Fortunately, tetanus is highly preventable. Here are some recommended steps to avoid contracting tetanus:
- Vaccination against tetanus. This is the most effective way to prevent tetanus. The tetanus vaccine is typically given to infants starting at six weeks of age. Additionally, doctors recommend booster shots, especially for pregnant women, to ensure continued immunity and protect both mother and child.
- Wearing shoes or slippers. Footwear provides a barrier against cuts and injuries, especially from sharp objects on the ground. Protecting your feet minimizes the risk of exposure to Clostridium tetani spores that can enter through puncture wounds.
- Regular brushing of teeth. Keeping teeth and gums healthy can prevent oral injuries that could allow bacteria to enter. Good dental hygiene reduces the likelihood of tooth decay or damage that could indirectly introduce bacteria.
- Frequent hand washing. Washing hands regularly helps remove bacteria that may be present on the skin. Clean hands are essential, especially when touching open wounds, as they help prevent infection.
- Immediate wound cleaning. Clean any wound promptly, even minor ones. Use soap and water to remove dirt and reduce the risk of bacterial contamination.
By following these preventive steps, individuals can significantly reduce their risk of tetanus. Regular vaccinations, hygiene practices, and wound care play essential roles in protecting against this serious yet preventable infection.
Risk Factors for Tetanus
 Image Source: www.npr.org
Image Source: www.npr.org
Both children and adults can contract tetanus, but certain groups are at higher risk of infection. Here are the groups with a greater likelihood of developing tetanus:
- Adults aged 20 to 64. Statistics show that people within this age range are more frequently affected by tetanus, largely because they are more active outside the home and more exposed to potential injuries. These adults are more likely to engage in activities that could lead to cuts or puncture wounds, increasing their risk of infection.
- Individuals with diabetes. People with diabetes are at a higher risk of infections, including tetanus, because of a generally weakened immune system. Additionally, diabetics may experience skin wounds or ulcers, especially on their feet, which can become entry points for the bacteria that cause tetanus.
- People who frequently inject medications. Those who regularly use injections, such as diabetic patients or others who self-administer medications, have a higher risk of tetanus. Repeated injections create puncture wounds that, if not done with sterile techniques, could expose the person to Clostridium tetani bacteria, especially if injections are administered in less sanitary conditions.
Understanding these higher-risk groups is essential for preventive care. Regular tetanus vaccinations, proper wound care, and sterile injection practices are especially important for those more susceptible to infection.
Tetanus FAQs
Tetanus, commonly known as “lockjaw,” is a serious bacterial infection that affects the nervous system, causing severe muscle stiffness and spasms. Caused by Clostridium tetani, tetanus is most often contracted through wounds contaminated with bacteria from soil, dust, or animal waste. While tetanus can be life-threatening, it is preventable with proper care and vaccination. Here are some frequently asked questions to help you understand tetanus, its symptoms, prevention, and treatment.
1. What is tetanus?
Tetanus is a bacterial infection caused by Clostridium tetani, which produces a powerful toxin affecting the nervous system. This toxin leads to painful muscle stiffness and spasms, particularly in the jaw and neck.
2. How is tetanus transmitted?
Tetanus bacteria enter the body through cuts, punctures, or wounds contaminated with spores from soil, dust, or animal feces. Common sources include stepping on a nail, cuts from sharp objects, or injuries involving dirt or rust.
3. What are the symptoms of tetanus?
Symptoms include stiffness in the jaw (lockjaw), neck, and other muscles, difficulty swallowing, fever, sweating, muscle spasms, and body pain. Symptoms typically appear 3 to 21 days after exposure.
4. Can tetanus be prevented?
Yes, tetanus can be effectively prevented with vaccination. The tetanus vaccine is often given as part of a combined shot, such as the DTaP or Tdap vaccine, which protects against tetanus, diphtheria, and pertussis. Regular booster shots every 10 years are also recommended.
5. Who is at risk of tetanus?
While anyone can get tetanus, it is more common in individuals who handle soil, work outdoors, or use non-sterile needles. People with certain conditions, such as diabetes, are also at higher risk due to potential skin wounds or weakened immunity.
6. How is tetanus diagnosed?
Doctors diagnose tetanus through a physical examination, assessing symptoms like muscle stiffness, spasms, and jaw lock. They may also ask about recent injuries or exposure to potential sources of Clostridium tetani.
7. What treatments are available for tetanus?
Treatment includes administering tetanus antitoxin to neutralize the toxin, antibiotics to control the infection, muscle relaxants, and, in severe cases, mechanical ventilation to assist breathing. Prompt treatment is essential to reduce complications.
8. Is tetanus contagious?
No, tetanus is not contagious and cannot be spread from person to person. It requires direct bacterial entry through a wound to cause infection.
9. Can you get tetanus more than once?
Yes, unlike many other infections, having tetanus once does not provide immunity. Vaccination and booster shots are still necessary to protect against future infections.
10. What should I do if I get a wound that might expose me to tetanus?
If you get a wound that might be at risk for tetanus, immediately clean the wound thoroughly with soap and water, apply antiseptic, and seek medical advice. A tetanus booster shot may be recommended if your vaccination is not up to date.