Summary
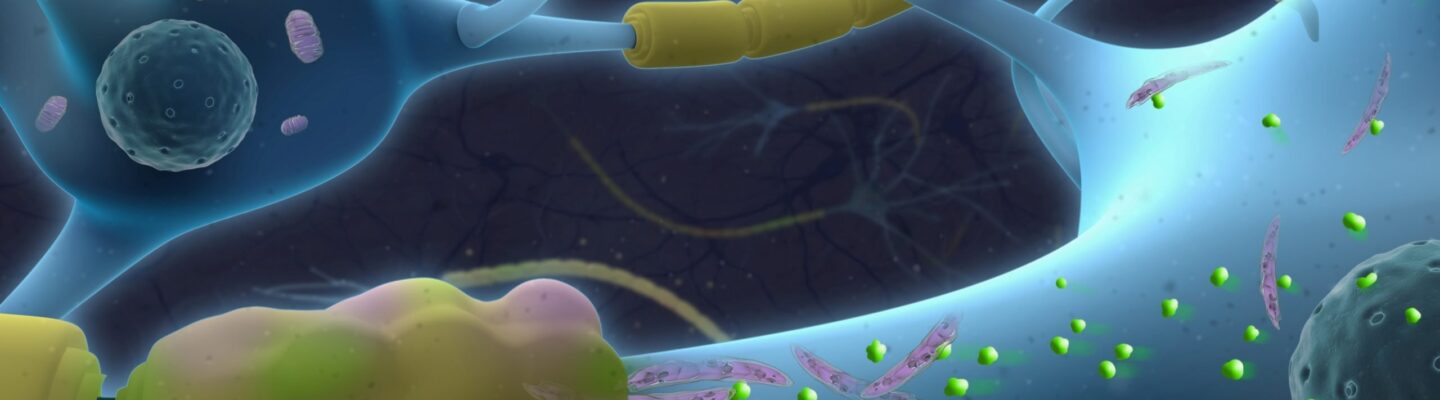
Multiple sclerosis (MS) is a long-term neurological condition affecting the nervous system, particularly the central nervous system (CNS), which includes the brain and spinal cord. In MS, the immune system mistakenly attacks the myelin sheath—a protective covering around nerve fibers. This damage disrupts the normal functioning of nerves and can lead to permanent scarring or degradation of the myelin sheath.
The breakdown of the myelin sheath manifests through various symptoms, such as difficulty walking, numbness in the limbs, vision problems, and more. The severity of these symptoms largely depends on the extent of the damage to the nerves. However, individuals with MS may experience prolonged periods of remission, during which they may not show any symptoms.
Currently, there is no definitive cure for multiple sclerosis. However, several treatment options are available to help manage the condition. The goal of these treatments is to facilitate recovery, slow the progression of the disease, and reduce the impact of symptoms.
Table of Contents
Symptoms of Multiple Sclerosis

One of the defining characteristics of multiple sclerosis is the wide range of symptoms experienced by individuals with the condition. Symptoms can vary significantly from person to person and may change as the disease progresses. However, the most common symptoms of multiple sclerosis include:
- Difficulty with coordination and walking, sometimes accompanied by tremors. Many people with MS experience muscle weakness, balance issues, and a lack of coordination, making walking and movement challenging.
- Numbness or weakness in one or two limbs, typically on one side of the body. This symptom often affects the arms or legs and may result in a reduced ability to perform everyday tasks.
- Neck movement accompanied by an electric-shock sensation, especially when bending the neck forward (Lhermitte Sign). This shock-like sensation is a hallmark symptom of MS and can be triggered by specific movements.
- Partial or complete vision loss, usually in one eye, often with pain during eye movement. Known as optic neuritis, this condition can cause temporary or, in some cases, permanent vision impairment.
- Prolonged double vision and blurred vision. Vision problems, including blurred or double vision, are common and may worsen over time if not managed.
- Anxiety and depression. Mood changes, particularly feelings of anxiety and depression, are frequently reported by those with MS and can impact overall mental health.
- Cognitive issues, such as difficulties with learning and memory. MS can affect cognitive function, leading to challenges in concentration, problem-solving, and remembering information.
- Slurred speech. Known as dysarthria, this can occur due to muscle weakness or coordination issues in the facial and throat muscles.
- Fatigue. Persistent fatigue is one of the most disabling symptoms of MS, often making daily tasks feel overwhelming.
- Dizziness. A sense of vertigo or imbalance is a common issue that can exacerbate coordination difficulties.
- Pain or tingling sensations throughout different parts of the body. Known as neuropathic pain, these sensations may be sharp, burning, or tingling and are caused by nerve damage.
- Sexual dysfunction. MS can impact sexual health, including reduced libido and other difficulties in intimate relations.
- Bladder issues, such as frequent or urgent urination. Many people with MS experience urinary urgency, retention, or incontinence.
- Bowel issues, primarily constipation. Difficulty with bowel movements is common, as MS can affect muscle function in the gastrointestinal tract.
Each individual with MS may experience a unique combination of these symptoms, which can fluctuate in intensity or disappear and return unpredictably.
Understanding the potential range of symptoms can help those affected by MS seek appropriate medical attention and explore management options. Early detection and treatment can play a crucial role in managing the progression of these symptoms.
Types of Multiple Sclerosis
Multiple sclerosis is classified into four main types, each with unique characteristics and progression patterns:
- Clinically Isolated Syndrome (CIS). This type is marked by the initial occurrence of neurological symptoms lasting at least 24 hours. CIS is considered the first episode of MS-related symptoms, but it does not yet meet the criteria for a full MS diagnosis. If further symptoms or lesions appear on MRI scans, a diagnosis of MS may follow.
- Relapse-Remitting Multiple Sclerosis (RRMS). This is the most common form of MS, where individuals experience episodes of new or worsening symptoms, known as relapses. These relapses are typically followed by partial or complete recovery periods (remissions) when symptoms may subside or disappear entirely. RRMS often involves cycles of flare-ups and remissions, which can vary greatly in severity and duration.
- Primary Progressive Multiple Sclerosis (PPMS). In PPMS, symptoms gradually worsen from the onset without periods of remission. Some patients may experience minor improvements or stabilization, but the overall trend is a continuous progression of symptoms over time. PPMS can lead to increased disability, although the rate of progression varies from person to person.
- Secondary Progressive Multiple Sclerosis (SPMS). SPMS usually develops after an initial phase of RRMS. In this type, the condition transitions to a more steadily progressive form, with symptoms worsening gradually. While there may still be occasional relapses, the trend shifts toward a continuous progression rather than distinct episodes of relapse and remission.
Each type of MS impacts individuals differently, and understanding these variations can be essential for effective symptom management and long-term treatment planning.
Diagnostic Procedures for Multiple Sclerosis
Diagnosing multiple sclerosis (MS) can be challenging, as symptoms often mimic those of other neurological conditions. There’s no single test to confirm MS, so a comprehensive diagnostic process is essential. Physicians rely on a combination of clinical evaluations, imaging, and laboratory tests to accurately diagnose MS. Common diagnostic procedures include:
- Magnetic Resonance Imaging (MRI). MRI scans are the primary tool used to diagnose MS, as they can detect lesions or scarring in the brain and spinal cord caused by myelin damage. The use of contrast dye in MRI can help differentiate between active and inactive lesions, giving a clearer picture of disease activity.
- Lumbar Puncture (Spinal Tap). This procedure involves taking a sample of cerebrospinal fluid (CSF) from the lower back to check for signs of inflammation and abnormal immune activity, which are common in MS. Elevated levels of specific antibodies (oligoclonal bands) in the CSF can support an MS diagnosis.
- Evoked Potentials Tests. These tests measure the electrical activity in the brain in response to stimuli, such as visual, auditory, or sensory signals. In people with MS, nerve pathways may be slowed due to demyelination, and these tests can detect these changes in nerve conduction.
- Blood Tests. Although blood tests cannot diagnose MS, they help rule out other conditions that may mimic MS symptoms, such as lupus, vitamin B12 deficiency, or certain infections.
- Neurological Examination. A thorough neurological exam assesses sensory function, muscle strength, coordination, and reflexes to identify areas affected by nerve damage. This evaluation helps build a clinical picture of the disease and track its progression.
- McDonald Criteria. This set of guidelines combines MRI findings, CSF analysis, and clinical evidence to diagnose MS based on lesion location, timing, and spread. The McDonald Criteria are especially useful in identifying MS after a single episode of symptoms, known as clinically isolated syndrome (CIS).
Early diagnosis allows for prompt treatment, which can help slow MS progression, reduce relapses, and improve quality of life. However, MS can vary greatly from person to person, so an individualized approach to diagnosis and ongoing evaluation is crucial for effective management.
Complications of Untreated Multiple Sclerosis
When multiple sclerosis (MS) goes untreated, the disease can progress and lead to a range of complications that significantly impact quality of life. While the rate of progression varies among individuals, untreated MS often results in worsening symptoms and increased disability over time. Common complications include:
- Mobility and Coordination Issues. As MS advances, untreated inflammation and nerve damage can lead to severe muscle weakness, loss of coordination, and balance problems. This can increase the risk of falls and injuries, eventually requiring the use of mobility aids, such as canes or wheelchairs.
- Chronic Pain and Muscle Spasms. Untreated MS can lead to chronic pain due to muscle stiffness (spasticity), nerve pain, and uncontrollable muscle spasms. These symptoms can become increasingly severe, reducing physical comfort and function in everyday activities.
- Cognitive Decline. MS affects the brain’s ability to process information, leading to memory problems, poor concentration, and difficulties with problem-solving. Without intervention, cognitive issues may worsen and can eventually interfere with work, social life, and personal relationships.
- Emotional and Mental Health Issues. Depression, anxiety, and mood swings are common in MS due to both the direct effects of the disease on the brain and the emotional toll of living with a chronic illness. Left untreated, these mental health challenges can compound the physical impacts of MS and reduce overall well-being.
- Bladder and Bowel Dysfunction. MS can interfere with the signals between the brain and the bladder or bowel, leading to incontinence, urinary tract infections, and constipation. These issues can worsen without treatment, affecting personal comfort and quality of life.
- Increased Fatigue. Fatigue is one of the most disabling symptoms of MS, and it often worsens as the disease progresses untreated. Persistent fatigue can make it challenging to carry out everyday tasks and lead to reduced independence.
- Sexual Dysfunction. Damage to the central nervous system in untreated MS can disrupt sexual function, including reduced libido, difficulty achieving arousal, or physical discomfort during sexual activity.
- Progressive Disability. MS is often a progressive disease, and untreated cases may experience a continuous worsening of symptoms, eventually leading to more severe physical disability. This can result in complete loss of independence and the need for full-time care.
Treating MS early can help manage symptoms, reduce the frequency and severity of relapses, and slow disease progression. Early intervention is essential for maintaining physical and mental health, enhancing quality of life, and minimizing the risk of these long-term complications.
Causes of Multiple Sclerosis
The exact cause of multiple sclerosis remains unknown. However, doctors and researchers believe it results from a combination of genetic and environmental factors. MS is also classified as an autoimmune disease, meaning the immune system mistakenly attacks the body’s healthy cells.
In autoimmune diseases like MS, the immune system targets the body’s own tissues—in this case, the myelin sheath that insulates nerve fibers. Myelin plays a crucial role in facilitating the smooth transmission of nerve impulses along nerve pathways. Think of myelin as the insulation around an electrical wire; when it becomes damaged, signals can’t travel efficiently or accurately. Similarly, if the myelin sheath is compromised, communication between the brain and different parts of the body is disrupted.
This breakdown in communication is what leads to the symptoms of multiple sclerosis. Beyond interrupted or misdirected nerve impulses, significant myelin damage can also cause the nerve fibers themselves to deteriorate permanently.
Prevention of Multiple Sclerosis

Since the origins and progression of multiple sclerosis (MS) are still not fully understood, there is no proven method for preventing the disease. However, certain lifestyle choices may help reduce the risk factors associated with MS:
- Avoid smoking. Smoking has been linked to an increased risk of developing MS and can exacerbate symptoms in those already diagnosed.
- Take vitamin D supplements. Low levels of vitamin D are associated with a higher risk of MS. Regular sunlight exposure or taking vitamin D supplements may support immune function and potentially lower MS risk.
- Practice intermittent fasting. Emerging research suggests that fasting may positively affect immune health, which could play a role in managing autoimmune diseases like MS.
- Consume moderate amounts of red wine. Moderate red wine consumption has been linked to potential anti-inflammatory effects, although this should be discussed with a doctor to ensure it aligns with personal health needs.
For individuals at higher risk of MS, one of the most critical steps is to stay attuned to any unusual symptoms and report them promptly to a healthcare provider. Early attention to symptoms can help in timely diagnosis and management, potentially slowing the progression of the disease.
Risk Factors for Multiple Sclerosis

Although the exact cause of multiple sclerosis (MS) is still unknown, certain risk factors are known to increase the likelihood of developing the condition:
- Age. MS is most commonly diagnosed between the ages of 16 and 55, though it can occur at any age.
- Gender. Women are significantly more likely to develop MS than men, particularly the relapse-remitting type.
- Family history. If a close relative, such as a parent or sibling, has MS, the risk of developing it is higher.
- Ethnicity. MS predominantly affects Caucasians, especially those of Northern European descent, while people of Asian, African, and Native American descent have a lower risk.
- Specific infections. Certain infections, particularly the Epstein-Barr virus (the cause of mononucleosis), are linked to an increased risk of MS.
- Other autoimmune diseases. Individuals with autoimmune conditions like type 1 diabetes, thyroid disorders, or inflammatory bowel disease are at higher risk for developing MS.
- Climate. MS is more prevalent in countries with colder climates, especially those farther from the equator, where less sunlight exposure may contribute to lower vitamin D levels.
- Vitamin D levels. Low levels of vitamin D and limited exposure to sunlight are associated with an increased risk of MS, as vitamin D supports immune function.
- Smoking. Smokers who experience an initial MS episode (clinically isolated syndrome) are more likely to progress to relapse-remitting MS (RRMS) than non-smokers.
Understanding these risk factors can help individuals and healthcare providers remain vigilant, especially for those with higher risk. While these factors don’t guarantee an MS diagnosis, they can influence susceptibility to the disease and potentially its progression.
Multiple Sclerosis FAQs
Here are some frequently asked questions about multiple sclerosis (MS) to help clarify common concerns and provide valuable information for those affected by the condition.
- What is multiple sclerosis?
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, particularly the brain and spinal cord. The immune system mistakenly attacks the myelin sheath, a protective covering around nerve fibers, leading to nerve damage and a wide range of symptoms, including mobility issues, pain, vision problems, and fatigue. - What causes multiple sclerosis?
The exact cause of MS remains unknown, but it’s believed to result from a combination of genetic and environmental factors. Certain infections, vitamin D deficiency, and smoking are also associated with an increased risk of developing MS. - Who is most at risk for multiple sclerosis?
MS can affect anyone, but it’s more common in people between the ages of 16 and 55, particularly women and those of Northern European descent. Having a family history of MS or other autoimmune diseases may also increase the risk. - What are the main symptoms of multiple sclerosis?
MS symptoms vary widely but commonly include muscle weakness, difficulty walking, numbness, vision problems, fatigue, and cognitive issues. Symptoms can differ in intensity and may come and go, depending on the type of MS. - How is multiple sclerosis diagnosed?
MS is diagnosed through a combination of neurological exams, MRI scans, lumbar puncture (spinal tap), and evoked potential tests. Physicians use the McDonald Criteria, which combines these findings to identify MS and distinguish it from other neurological conditions. - Is there a cure for multiple sclerosis?
Currently, there is no cure for MS, but treatments are available to help manage symptoms, slow disease progression, and reduce relapses. Early intervention and regular monitoring can significantly improve quality of life for those with MS. - What treatments are available for MS?
Treatment options for MS include disease-modifying therapies (DMTs), corticosteroids for relapse management, physical therapy, and medications to address specific symptoms. Lifestyle changes, such as regular exercise and a balanced diet, can also help manage MS symptoms. - Can MS be prevented?
While there is no known way to prevent MS, certain lifestyle choices, like not smoking, maintaining healthy vitamin D levels, and managing autoimmune conditions, may reduce the risk of developing MS or help manage its symptoms. - What are the types of multiple sclerosis?
MS is classified into four main types: Clinically Isolated Syndrome (CIS), Relapse-Remitting MS (RRMS), Primary Progressive MS (PPMS), and Secondary Progressive MS (SPMS). Each type has distinct characteristics and progression patterns. - What complications can occur if MS is left untreated?
Untreated MS can lead to a range of complications, including chronic pain, severe mobility issues, cognitive decline, bladder and bowel dysfunction, and, ultimately, progressive disability. Early treatment is crucial to slow disease progression and manage symptoms. - How does MS affect daily life?
The impact of MS on daily life varies by individual and disease progression. While some may experience mild symptoms, others may face more significant physical and cognitive challenges. With treatment and support, many people with MS can lead fulfilling lives, although adjustments in lifestyle and work may be necessary. - What should I do if I suspect I have MS symptoms?
If you experience symptoms like unexplained numbness, vision issues, or muscle weakness, consider consulting a healthcare provider. Early diagnosis and treatment can help manage the disease and improve long-term outcomes.