Summary
Pneumonia is a serious lung infection that can affect anyone, but it is particularly dangerous for older adults, infants, and individuals with weakened immune systems. The severity of the illness can range from mild to life-threatening, depending on the person’s overall health and the cause of the infection.
Pneumonia causes inflammation of the air sacs (alveoli) in the lungs, which can fill with pus or fluid, making it difficult to breathe. This accumulation of fluid prevents oxygen from reaching the bloodstream efficiently, resulting in symptoms like difficulty breathing, chest pain, and fatigue.
Common symptoms of pneumonia include coughing (sometimes producing phlegm), fever, chills, and shortness of breath.
The condition can be treated with antibiotics, antiviral medications, or other therapies, depending on the cause and severity of the infection. Early diagnosis and prompt treatment are essential for preventing complications and ensuring a full recovery.
Table of Contents
Symptoms of Pneumonia

Pneumonia symptoms can vary depending on the cause of the infection (bacterial, viral, or mycoplasma) and the severity of the condition. Identifying these symptoms is key to prompt treatment. Here are the common signs associated with different types of pneumonia:
-
Bacterial pneumonia symptoms:
- Fever. High body temperature is a typical sign, often accompanied by chills.
- Bluish tint to the lips and nails. This occurs due to low oxygen levels in the blood.
- Cough with sputum. The cough may produce green, yellow, or blood-tinged mucus.
- Delirium or confusion. This can occur in older adults due to high fever.
- Excessive sweating. Profuse sweating may accompany the fever.
- Loss of appetite. The illness may cause a significant decrease in appetite.
- Fatigue. Weakness or extreme tiredness is common.
- Rapid, shallow breathing. The body compensates for reduced oxygen intake by breathing quickly.
- Fast heart rate. An elevated pulse can be a response to fever and infection.
- Shortness of breath. Breathing difficulties may occur, especially during physical activity.
- Chest pain. Sharp or stabbing pain may be felt in the chest, especially during deep breathing or coughing.
-
Viral pneumonia symptoms:
- Symptoms may be similar to bacterial pneumonia, but they can also include:
- Headache. A common sign that may appear early in the illness.
- Increased shortness of breath. This may worsen as the infection progresses.
- Muscle pain. Aching in the muscles, often associated with viral infections.
- Extreme fatigue. Feeling very weak or exhausted is more pronounced.
- Worsening cough. The cough may become more persistent or severe over time.
-
Mycoplasma pneumonia symptoms:
- This type often presents with milder symptoms compared to other forms of pneumonia, but may still include:
- Severe cough. A dry or wet cough, often accompanied by mucus production.
- Cold-like symptoms. Mycoplasma pneumonia may start with symptoms similar to a common cold, such as a runny nose or sore throat.
- Mild chest pain. Some people may experience discomfort in the chest area.
Recognizing these symptoms can help in seeking medical care early, which is crucial in preventing complications and ensuring effective treatment.
Types of Pneumonias
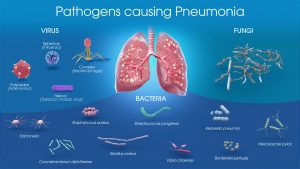
Understanding the different types of pneumonia is essential for proper diagnosis and treatment. The following are the main types of pneumonia:
- Bacterial pneumonia. This type of pneumonia is caused by various bacteria, with Streptococcus pneumoniae being the most common. It frequently affects individuals with weakened immune systems, such as those who are elderly, malnourished, or suffering from other illnesses. The bacteria can easily enter the lungs, causing infection and inflammation. Bacterial pneumonia is often characterized by sudden symptoms such as high fever, chills, chest pain, and productive cough.
- Viral pneumonia. Caused by viruses such as the influenza virus, respiratory syncytial virus (RSV), or the coronavirus, viral pneumonia accounts for about one-third of all pneumonia cases. The symptoms usually develop gradually and may start with a headache, fever, and muscle aches before progressing to a dry cough and difficulty breathing. Viral pneumonia can also make individuals more susceptible to secondary bacterial infections, leading to a mixed type of pneumonia.
- Mycoplasma pneumonia. This type is caused by the bacterium Mycoplasma pneumoniae. It is often referred to as “walking pneumonia” because symptoms are typically milder than other forms of pneumonia. It can affect people of all ages, but it is most common in older children and young adults. Symptoms may include a persistent dry cough, fatigue, sore throat, and headache.
- Fungal pneumonia. Although less common, fungal pneumonia can occur in individuals who have weakened immune systems, such as those undergoing chemotherapy or living with HIV/AIDS. It can be caused by fungi such as Histoplasma, Coccidioides, and Cryptococcus, which are commonly found in soil or bird droppings. Symptoms may resemble those of bacterial pneumonia but may be more difficult to diagnose due to their rarity.
These different types of pneumonia can vary significantly in terms of symptoms, causes, and treatment. Identifying the specific type of pneumonia helps healthcare providers choose the most effective treatment options.
Diagnostic Procedures for Pneumonia
Diagnosing pneumonia involves a series of evaluations and tests to determine the cause, severity, and type of infection. Here are the common diagnostic procedures used:
- Medical history and physical examination. The doctor will begin by reviewing the patient’s medical history and symptoms, including any recent respiratory infections, chronic illnesses, or risk factors. A physical examination may involve listening to the lungs with a stethoscope for abnormal sounds, such as crackling or wheezing, which can indicate fluid in the lungs.
- Chest X-ray. A chest X-ray is a key diagnostic tool for pneumonia. It can help detect the presence and extent of inflammation or fluid in the lungs and identify which areas are affected. While it may not indicate the specific cause, it provides crucial information about the condition of the lungs.
- Blood tests. Blood tests, such as a complete blood count (CBC), can help determine the presence of an infection and the severity of inflammation. Additionally, blood cultures may be conducted to check for bacteria in the bloodstream, indicating a more severe or widespread infection.
- Sputum test. A sputum sample, or phlegm coughed up from the lungs, can be analyzed to identify the specific microorganism causing the pneumonia, such as bacteria, fungi, or viruses. This test helps guide appropriate antibiotic or antiviral treatment.
- Pulse oximetry. This non-invasive test measures the oxygen saturation level in the blood. Low blood oxygen levels may indicate that the lungs are not transferring enough oxygen to the bloodstream, suggesting a more severe case of pneumonia.
- Computed tomography (CT) scan. A CT scan of the chest may be recommended if the chest X-ray results are inconclusive or if there are complications. It provides a more detailed view of the lungs and can help detect other underlying lung conditions.
- Bronchoscopy. In more complex cases where the cause of pneumonia is unclear, a bronchoscopy may be performed. This procedure involves inserting a thin, flexible tube with a camera into the airways to examine the lungs and collect samples for further analysis.
- Pleural fluid analysis. If there is fluid accumulation around the lungs (pleural effusion), a sample of this fluid may be taken for testing. This can help identify the cause of the infection and determine the most suitable treatment.
These diagnostic procedures help healthcare providers accurately diagnose pneumonia, determine the severity of the infection, and develop an effective treatment plan to improve the patient’s health.
Complications of Untreated Pneumonia
If pneumonia is left untreated, it can lead to serious and potentially life-threatening complications. These complications can significantly impact a person’s health and may require urgent medical attention. Here are some of the common complications associated with untreated pneumonia:
- Respiratory failure. As pneumonia progresses, the inflammation and fluid buildup in the lungs can severely impair oxygen exchange. This can result in respiratory failure, a condition where the lungs cannot provide enough oxygen to the blood or remove enough carbon dioxide from the body, requiring mechanical ventilation or other emergency interventions.
- Sepsis. When the infection causing pneumonia spreads to the bloodstream, it can lead to sepsis, a life-threatening response to infection that causes widespread inflammation in the body. Sepsis can lead to organ failure and, in severe cases, septic shock, which can be fatal if not treated promptly.
- Lung abscess. Untreated pneumonia can lead to the formation of an abscess in the lungs. A lung abscess is a pocket of pus that develops in the lung tissue, often causing symptoms such as persistent cough, fever, and night sweats. Treatment may involve antibiotics or drainage of the abscess.
- Pleural effusion. Pneumonia can cause fluid to accumulate in the pleural space, the area between the lungs and the chest wall. This condition, known as pleural effusion, can make breathing difficult and may require drainage if the fluid becomes infected (a condition called empyema).
- Acute respiratory distress syndrome (ARDS). Severe cases of pneumonia can lead to ARDS, a serious condition where the lungs become inflamed and filled with fluid. ARDS can cause severe breathing difficulties and requires intensive care, including mechanical ventilation.
- Worsening of underlying conditions. Individuals with pre-existing health conditions, such as chronic obstructive pulmonary disease (COPD), asthma, or heart disease, may experience worsening symptoms and increased risk of complications when pneumonia is not treated.
- Kidney or heart damage. Severe infections like pneumonia can affect other organs, potentially leading to kidney or heart damage. For example, sepsis resulting from untreated pneumonia may cause acute kidney injury or heart-related complications.
Early diagnosis and appropriate treatment are essential in preventing these complications and ensuring a full recovery. Prompt medical care can help reduce the risk of life-threatening outcomes associated with pneumonia.
Causes of Pneumonia
Understanding the causes of pneumonia is crucial for effective treatment. Pneumonia is typically caused by bacteria, viruses, fungi, or other microorganisms that enter the lungs through inhalation. Although the body has natural defenses against these pathogens, there are instances where they can overcome the immune system, leading to infection. In addition to knowing the pathogens responsible, it is important to understand the different ways in which pneumonia can be acquired:
- Community-acquired pneumonia (CAP). This is the most common type of pneumonia and is contracted outside of healthcare settings. It can spread through close contact with an infected person or inhalation of airborne pathogens, such as bacteria (Streptococcus pneumoniae), viruses (influenza or respiratory syncytial virus), or fungi (Histoplasma). The risk increases in crowded places or during outbreaks of respiratory illnesses.
- Hospital-acquired pneumonia (HAP). This type occurs in individuals who are hospitalized for other reasons. It is more likely to involve stronger, antibiotic-resistant bacteria, making it more difficult to treat. Patients on ventilators or those with weakened immune systems are at higher risk for hospital-acquired pneumonia.
- Healthcare-associated pneumonia (HCAP). This form of pneumonia is contracted in long-term healthcare facilities, dialysis centers, or outpatient clinics. Similar to hospital-acquired pneumonia, it is caused by bacteria that may be more resistant to common antibiotics due to the frequent use of antimicrobial agents in these settings.
- Aspiration pneumonia. This occurs when food, liquid, saliva, or vomit is inhaled into the lungs, leading to an infection. The inhaled material can introduce harmful bacteria into the lungs, especially if the person has difficulty swallowing or has a condition that affects the gag reflex. Individuals who have neurological disorders, are sedated, or have a history of excessive alcohol use are at greater risk for aspiration pneumonia.
Identifying the cause of pneumonia helps healthcare providers determine the appropriate treatment plan, as different pathogens and modes of transmission may require different therapeutic approaches.
Prevention of Pneumonia
neumonia can often be prevented through the following measures:
- Vaccination. Getting vaccinated is one of the most effective ways to prevent pneumonia. Vaccines are available for certain types of pneumonia-causing bacteria and viruses, such as Streptococcus pneumoniae and influenza. It is especially important for high-risk groups, including young children, older adults, and individuals with weakened immune systems, to stay up to date with their vaccinations.
- Strengthening the immune system. Maintaining a strong immune system can help the body fight off infections more effectively. This can be achieved by:
- Getting enough sleep. Aim for 7-9 hours of sleep each night to support overall health.
- Eating a balanced diet. Include plenty of fruits, vegetables, whole grains, and lean proteins to ensure adequate nutrition.
- Regular exercise. Engage in physical activities such as walking, jogging, or strength training to boost immune function.
- Practicing proper hygiene. Good hygiene is crucial in reducing the risk of infection. Follow these practices:
- Wash hands regularly. Wash your hands with soap and water for at least 20 seconds, especially after using the bathroom, before eating, or after coughing and sneezing.
- Use hand sanitizer. When soap and water are not available, use an alcohol-based hand sanitizer.
- Clean and disinfect living spaces. Keep the home and workplace clean, especially high-touch surfaces. Use antibacterial sprays or wipes if needed.
- Avoiding smoking. Smoking damages the lungs’ natural defense mechanisms, making it easier for bacteria and viruses to cause infections. Quitting smoking can significantly lower the risk of developing pneumonia and improve overall lung health.
- Limiting exposure to sick individuals. If someone around you is sick with a respiratory infection, try to maintain a safe distance, wear a mask if necessary, and avoid sharing personal items like utensils or towels.
Taking these preventive steps can greatly reduce the risk of pneumonia and help protect against respiratory infections.
Risk Factors for Pneumonia
While bacterial pneumonia can affect people of all ages, certain factors can increase the risk of developing the condition. The following factors are associated with a higher likelihood of contracting pneumonia:
- Age.
- Children under 2 years old. Infants and young children have immature immune systems, making them more susceptible to pneumonia.
- Adults 65 years and older. Older adults often have weakened immune defenses, increasing their risk of serious infections.
- Weakened immune system. Conditions such as HIV/AIDS, cancer treatments (chemotherapy), or use of immunosuppressive drugs can impair the immune system’s ability to fight infections, raising the risk of pneumonia.
- Smoking. Tobacco smoke damages the lungs and weakens their ability to clear mucus and bacteria, making smokers more vulnerable to respiratory infections.
- Excessive alcohol consumption. Heavy drinking can impair the immune system and increase the risk of aspiration pneumonia, where stomach contents enter the lungs.
- Recent surgery or hospitalization. Having a surgical procedure, especially on the chest or abdomen, can increase the risk of developing pneumonia due to reduced lung function or prolonged bed rest.
- Chronic lung diseases. Conditions such as chronic obstructive pulmonary disease (COPD), bronchiectasis, or cystic fibrosis can make it easier for infections to develop in the lungs.
- Viral infections. Recent viral infections like the flu or respiratory syncytial virus (RSV) can weaken the lungs and make them more susceptible to bacterial pneumonia.
- Asthma. Individuals with asthma may be at increased risk of pneumonia, especially if the condition is not well-managed.
- Use of a ventilator in the intensive care unit (ICU). Being on a ventilator can increase the risk of ventilator-associated pneumonia (VAP), a serious lung infection that occurs in patients receiving mechanical ventilation.
Understanding these risk factors can help identify individuals who may be more vulnerable to pneumonia and guide preventive measures, such as vaccination, smoking cessation, and timely medical treatment.
Pneumonia FAQs
- What is pneumonia?
Pneumonia is an infection that inflames the air sacs (alveoli) in one or both lungs. The alveoli may fill with fluid or pus, causing symptoms such as cough, fever, chills, and difficulty breathing. It can be caused by bacteria, viruses, fungi, or other microorganisms. - What are the symptoms of pneumonia?
Common symptoms include cough (often with phlegm), fever, chills, shortness of breath, chest pain when breathing or coughing, fatigue, and headache. Symptoms can range from mild to severe, depending on the type of pneumonia and the individual’s overall health. - What causes pneumonia?
Pneumonia can be caused by various pathogens, including bacteria (e.g., Streptococcus pneumoniae), viruses (e.g., influenza, RSV), fungi (e.g., Histoplasma), and mycoplasma bacteria. It can also occur from inhaling irritants or foreign substances, leading to aspiration pneumonia. - Who is at risk of developing pneumonia?
While anyone can develop pneumonia, certain groups are at higher risk, including infants and young children, adults aged 65 or older, people with weakened immune systems, those with chronic lung conditions, smokers, and individuals who have recently been hospitalized. - Is pneumonia contagious?
Yes, pneumonia can be contagious, especially if caused by bacteria or viruses. It can spread through respiratory droplets when an infected person coughs or sneezes. However, fungal pneumonia and aspiration pneumonia are not contagious. - How is pneumonia diagnosed?
Diagnosis typically involves a physical examination, chest X-ray, blood tests, and sometimes a sputum test to identify the specific cause. In more severe cases, a CT scan or bronchoscopy may be required for further evaluation. - How is pneumonia treated?
Treatment depends on the cause. Bacterial pneumonia is usually treated with antibiotics, while antiviral medications may be used for viral pneumonia. Rest, hydration, and fever-reducing medications are also recommended to help alleviate symptoms. Severe cases may require hospitalization and oxygen therapy. - Can pneumonia be prevented?
Yes, pneumonia can often be prevented with vaccines, such as the pneumococcal vaccine and the flu shot. Practicing good hygiene, quitting smoking, and maintaining a healthy lifestyle can also reduce the risk. - How long does it take to recover from pneumonia?
Recovery time can vary depending on the type of pneumonia and the individual’s health. Mild cases may resolve in one to two weeks, while more severe cases can take several weeks to a few months for full recovery. - When should I see a doctor if I think I have pneumonia?
It is important to seek medical attention if you experience symptoms such as persistent cough, high fever, chest pain, difficulty breathing, or worsening symptoms. Early diagnosis and treatment can help prevent complications.