The liver plays an essential role in maintaining the overall health of the body. However, like other organs, it is vulnerable to various diseases and conditions. When the liver becomes weakened or damaged, it can significantly impair the body’s ability to function properly. In severe cases, liver failure can be life-threatening, underscoring the importance of liver health and timely medical intervention.
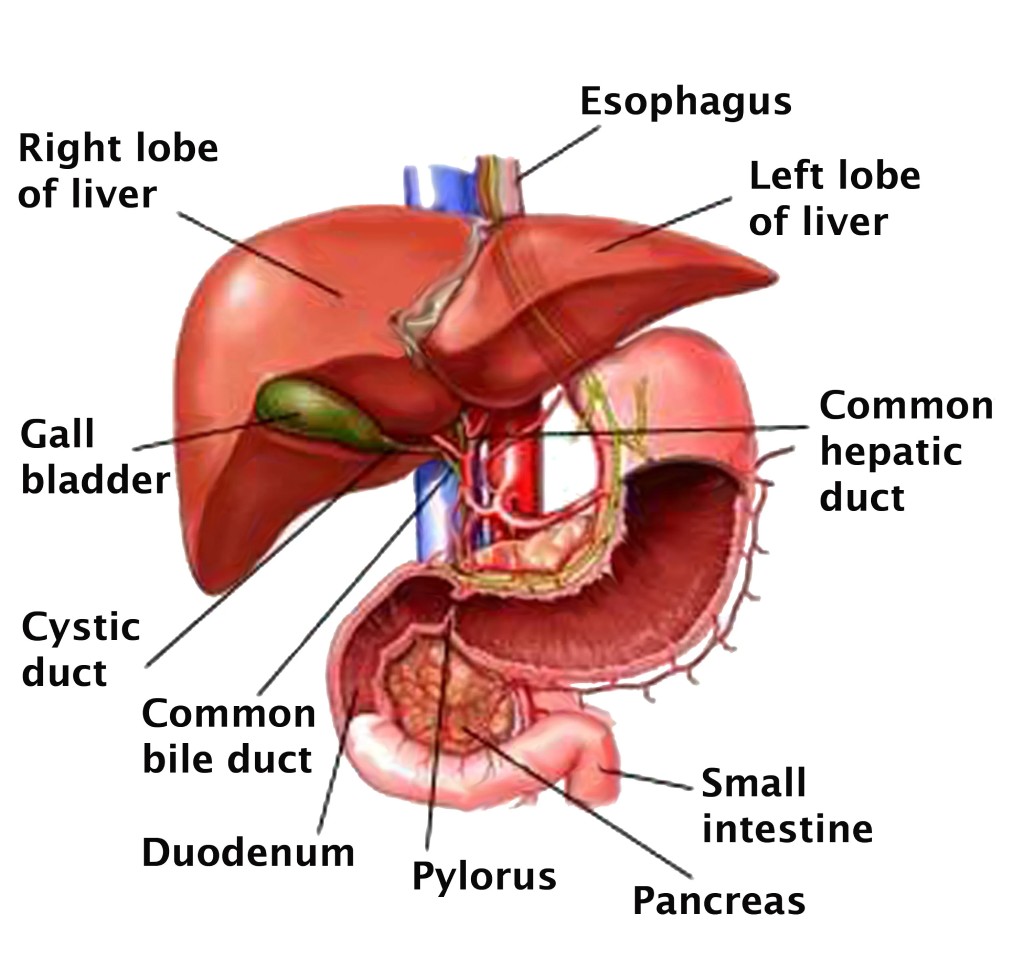
Image Source: www.acs.org
The liver is a large, vital organ located beneath the ribs on the right side of the abdomen. It is a crucial part of the digestive system, working in conjunction with the gallbladder and pancreas to aid in digestion and overall body function.
The liver’s primary function is to filter blood coming from the digestive tract, removing toxins and processing nutrients. It produces bile, a substance that helps break down fats in the small intestine. Bile flows from the liver to the gallbladder, where it is stored until needed during digestion.
In addition to aiding digestion, the liver plays several other key roles:
When the liver becomes diseased or damaged, its ability to perform these essential functions can be compromised. This can lead to a buildup of toxins in the body, issues with digestion, and imbalances in blood and nutrient levels.
Although the liver has an incredible capacity to regenerate, prolonged or severe damage can lead to serious conditions such as cirrhosis or liver failure, which may require significant medical intervention, including liver transplantation.
Although there are different types of conditions that can affect the liver, many of them share similar symptoms. These symptoms often indicate that the liver is not functioning properly and should not be ignored. Below are the most common signs and symptoms associated with liver disease:
Liver disease presents a wide range of symptoms that can affect multiple systems in the body. From jaundice to swelling and chronic fatigue, these signs indicate that the liver is struggling to perform its vital functions. Recognizing these symptoms early and seeking medical advice can help prevent more severe complications and improve outcomes for those with liver di
Here are the various types of liver diseases and a brief description of each.
Liver diseases can range from inherited conditions to those caused by infections or unhealthy lifestyles. While the causes may differ, many of these diseases can lead to severe complications such as cirrhosis or liver failure if left untreated. It is essential to recognize the symptoms early and consult a specialist for proper diagnosis and treatment to prevent the progression of the disease.
Diagnosing liver disease involves a combination of physical examinations, blood tests, imaging studies, and sometimes more invasive procedures. These diagnostic tools help healthcare professionals determine the extent of liver damage, identify the underlying cause, and assess the liver’s overall function.
Blood tests, often referred to as liver function tests (LFTs), are one of the first steps in diagnosing liver disease. These tests measure levels of liver enzymes, bilirubin, proteins, and clotting factors to assess how well the liver is functioning. Elevated liver enzymes, such as alanine transaminase (ALT) and aspartate transaminase (AST), may indicate liver damage or inflammation. Blood tests can also detect infections like hepatitis and monitor the liver’s ability to produce essential proteins.
Imaging studies are crucial for visualizing the liver’s structure and identifying abnormalities such as tumors, scarring (cirrhosis), or fat accumulation. Common imaging procedures include:
In some cases, a liver biopsy may be required to confirm a diagnosis. During this procedure, a small sample of liver tissue is removed using a needle and examined under a microscope. A biopsy can help determine the extent of liver damage, the presence of inflammation, fibrosis, or cirrhosis, and the cause of the disease (such as viral hepatitis or fatty liver disease).
FibroScan is a specialized ultrasound technique that measures liver stiffness, which can indicate fibrosis or scarring. It is a non-invasive alternative to a liver biopsy for assessing the degree of liver damage in conditions like cirrhosis and chronic hepatitis. This test is particularly useful for monitoring the progression of liver disease without the need for repeated biopsies.
An upper endoscopy, also known as an esophagogastroduodenoscopy (EGD), may be performed to examine the esophagus, stomach, and the upper part of the small intestine. This procedure helps detect complications of liver disease, such as esophageal varices, which are swollen veins that can bleed due to portal hypertension caused by cirrhosis.
In cases where liver disease is suspected to be hereditary, genetic testing may be recommended. This test can identify genetic mutations responsible for conditions like hemochromatosis, Wilson’s disease, or alpha-1 antitrypsin deficiency. Identifying these mutations helps guide treatment and manage family members’ risk of developing liver disease.
Diagnosing liver disease requires a combination of tests that assess liver function, detect structural abnormalities, and identify underlying causes. Early diagnosis through these procedures allows for prompt treatment, which is critical to prevent further damage and manage the condition effectively.
Untreated liver disease can lead to a variety of serious complications, many of which can be life-threatening. Below are some of the most common complications:
Cirrhosis occurs when healthy liver tissue is replaced by scar tissue due to long-term damage. This scarring impairs the liver’s ability to function properly, leading to issues such as poor blood filtration, reduced bile production, and nutrient imbalances. Over time, cirrhosis can progress to liver failure, where the liver ceases to function. Once cirrhosis develops, the damage is permanent, and in advanced stages, a liver transplant may be required.
Liver failure is the point at which the liver loses its ability to perform its essential functions, such as filtering toxins, aiding in digestion, and producing proteins necessary for blood clotting. This condition can develop gradually (chronic liver failure) or suddenly (acute liver failure). Symptoms include jaundice, confusion, fluid buildup in the abdomen, and easy bruising. Without immediate medical attention, liver failure can be fatal, and often the only solution is a liver transplant.
Hepatic encephalopathy occurs when toxins that the liver normally filters out of the bloodstream begin to accumulate in the body and reach the brain. This results in neurological symptoms ranging from confusion and mood swings to severe cognitive impairment and coma. If not addressed, hepatic encephalopathy can become life-threatening, as the buildup of toxins will continue to affect brain function and overall health.
Ascites is the accumulation of fluid in the abdomen, which is often a result of cirrhosis or severe liver damage. As the liver loses function, it fails to regulate the body’s fluid levels, causing discomfort and making breathing difficult. Ascites can also lead to serious infections, such as spontaneous bacterial peritonitis (SBP), which requires immediate treatment to prevent further complications.
Portal hypertension occurs when blood flow through the liver is obstructed, causing increased pressure in the portal vein, which carries blood to the liver. This pressure leads to the development of swollen veins (varices) in the esophagus and stomach, which can rupture and cause life-threatening internal bleeding. Portal hypertension is a major complication of cirrhosis and requires close medical monitoring.
Jaundice is a common sign of liver dysfunction, characterized by yellowing of the skin and eyes. It happens when the liver is unable to process bilirubin, a waste product formed from the breakdown of red blood cells. While jaundice itself is not life-threatening, it is a clear indication of underlying liver disease that, if untreated, can progress to more serious conditions like liver failure.
Chronic liver diseases, particularly cirrhosis and hepatitis B or C, significantly increase the risk of developing liver cancer, specifically hepatocellular carcinoma (HCC). This type of cancer often develops without symptoms in its early stages and is usually diagnosed at an advanced stage, when treatment options are limited. If left untreated, liver cancer can rapidly spread to other organs, with a poor prognosis.
The liver produces proteins necessary for blood clotting, and when it becomes damaged, the body’s ability to form clots is impaired. This can lead to frequent nosebleeds, easy bruising, and potentially life-threatening internal bleeding. People with advanced liver disease are especially prone to bleeding complications, particularly when combined with conditions like portal hypertension.
Individuals with liver disease have a weakened immune system, which makes them more vulnerable to infections. One common infection in people with ascites is spontaneous bacterial peritonitis (SBP), which is an infection of the abdominal fluid. Infections can accelerate liver damage and may lead to sepsis, a life-threatening response to infection that can cause multiple organ failure.
Untreated liver disease can have serious consequences, affecting not only the liver but also other critical organs and systems in the body. Early detection, regular monitoring, and timely intervention are essential to managing liver disease and preventing the progression to life-threatening complications like liver failure, cancer, or severe infections.
Liver disease can result from a variety of factors, with the most common causes being infections and the accumulation of harmful substances in the liver. Below are some of the primary causes:
Certain parasites and viruses can cause infections in the liver, leading to inflammation and impaired liver function. The most common infectious liver diseases are caused by different types of hepatitis viruses, which include:
These viruses are typically spread through contaminated food and water, blood transfusions from infected individuals, or sexual contact with someone carrying the virus. When the liver becomes infected, it may struggle to perform its critical functions, leading to serious health complications if not treated.
In some cases, the body’s immune system mistakenly attacks healthy liver cells, leading to inflammation and liver damage. Autoimmune diseases affecting the liver include.
Certain inherited genetic mutations can cause harmful substances to build up in the liver, leading to liver damage. These conditions may be passed down from one or both parents and include.
Tumors, polyps, and cancers can develop in the liver or bile ducts, causing significant damage. These growths may interfere with the liver’s ability to filter blood and produce bile, leading to life-threatening complications. Liver cancer, including hepatocellular carcinoma, is one of the most serious outcomes of untreated liver disease.
Excessive alcohol consumption is a well-known cause of liver disease. Over time, heavy drinking leads to liver inflammation and scarring (cirrhosis). Other lifestyle factors, such as consuming a diet high in saturated fats and cholesterol, can also damage the liver by contributing to non-alcoholic fatty liver disease (NAFLD). In this condition, fat accumulates in the liver, which can eventually impair its function.
Liver disease can arise from infections, autoimmune disorders, genetic factors, tumors, and unhealthy lifestyle choices. Recognizing these causes is important for early intervention and treatment to prevent long-term liver damage and complications.
When dealing with liver disease or any liver-related condition, it is essential to consult a specialist known as a hepatologist, who focuses on diagnosing and treating liver disorders.
Some liver diseases are chronic and may not completely go away. However, hepatologists provide guidance on effectively managing symptoms, even for recurrent liver conditions. These recommendations include:
Depending on the specific liver condition, patients may be prescribed the following types of medications:
In severe cases of liver disease, surgery may be required to remove damaged tissue or tumors. For advanced liver failure, a liver transplantation may be necessary if other treatments prove unsuccessful.
Like many other diseases, prevention is the most effective way to maintain liver health and overall well-being. Here are some key steps that can help prevent liver disease:

Limit alcohol consumption to moderate levels. For men, this means no more than two alcoholic drinks per day, while women should limit it to one drink per day. Excessive alcohol intake is a leading cause of liver disease.
Steer clear of using injectable drugs and never share needles or syringes. Engage in safe sex practices, such as using condoms, to prevent the transmission of infections like hepatitis. If you plan to get a tattoo, ensure that the instruments used are sterile and clean.
Consult your doctor about vaccinations to protect against hepatitis viruses, particularly hepatitis A and B. Vaccination strengthens your immunity and significantly reduces the risk of contracting these infections.
Always take prescription and non-prescription medications as directed by your doctor. Avoid mixing medications with alcohol, as this can severely damage the liver. Overuse of certain medications, especially pain relievers like acetaminophen, can lead to liver toxicity.
Hepatitis can be transmitted through direct contact with infected blood or bodily fluids. If you work in a healthcare setting or come into contact with these fluids, always use protective equipment to minimize your risk.
Air fresheners, insecticides, and other household chemicals contain substances that may harm the liver. Ensure proper ventilation when using these products, and consider wearing a mask to avoid inhaling harmful fumes. Avoid direct contact with these substances on the skin.
Obesity is a major risk factor for developing non-alcoholic fatty liver disease (NAFLD), a condition where fat builds up in the liver and leads to damage. Regular exercise and a balanced diet can help you maintain a healthy weight and protect your liver.
Taking proactive steps to prevent liver disease is vital for protecting your liver and maintaining overall health. By moderating alcohol intake, practicing safe behaviors, getting vaccinated, and maintaining a healthy lifestyle, you can significantly reduce your risk of liver disease. Preventive measures are always easier and more effective than treating advanced liver conditions, so it’s important to incorporate these habits into your daily life.
Several factors can increase the likelihood of developing liver disease. These risk factors include behaviors, medical conditions, and environmental exposures that affect liver health. Below are the most common risk factors for liver disease:
Using needles that have been previously used by others, especially for injecting drugs, significantly increases the risk of contracting infections like hepatitis B and C, both of which can lead to liver disease.
Tattoos performed with unsterilized or unclean needles can introduce viruses such as hepatitis into the bloodstream, putting you at risk for liver infections.
Jobs that involve handling blood or body fluids (such as healthcare workers or emergency responders) pose a higher risk for contracting viral infections, including hepatitis, if proper precautions are not taken.
Engaging in sexual activities without proper protection, particularly with partners whose health history is unknown, increases the risk of sexually transmitted infections, including hepatitis B, which can lead to liver damage.
People with diabetes or elevated cholesterol levels are at a higher risk of developing non-alcoholic fatty liver disease (NAFLD), which can progress to more serious liver conditions like cirrhosis if left untreated.
Being overweight or obese contributes to the buildup of fat in the liver, leading to conditions like non-alcoholic fatty liver disease (NAFLD), which can worsen over time and result in liver damage or failure.
Frequent exposure to toxic chemicals, such as pesticides or industrial solvents, can cause liver damage. These substances are processed by the liver, and repeated exposure can overwhelm the organ, leading to inflammation or toxicity.
Consuming large amounts of certain herbal supplements, especially those not regulated for safety, can lead to liver toxicity. Some herbs can interfere with liver function or interact negatively with medications.
Combining medications, particularly pain relievers or other drugs, with alcohol can severely strain the liver and lead to liver toxicity. This dangerous mix increases the risk of liver failure, especially when medications are taken in larger doses than recommended.
Taking medications in amounts exceeding the recommended dosage can damage the liver over time, especially drugs like acetaminophen (paracetamol) that, in high doses, are known to cause acute liver failure.
Understanding the risk factors for liver disease is crucial for prevention. By avoiding risky behaviors, such as sharing needles or mixing medications with alcohol, and maintaining a healthy lifestyle, individuals can significantly reduce their risk of developing liver disease. Regular monitoring of conditions like diabetes, cholesterol levels, and obesity, along with limiting exposure to toxic chemicals, can further protect liver health.
This article was written by Mediko.PH staff under the medical supervision and review of Dr. Anthony C. So, BSPT, MD, FPARM. This article is intended to provide accurate and reliable health-related information. However, this is not official and personalized medical advice, nor is it a diagnosis or prescription. Readers are advised to consult a doctor for proper care.