Summary
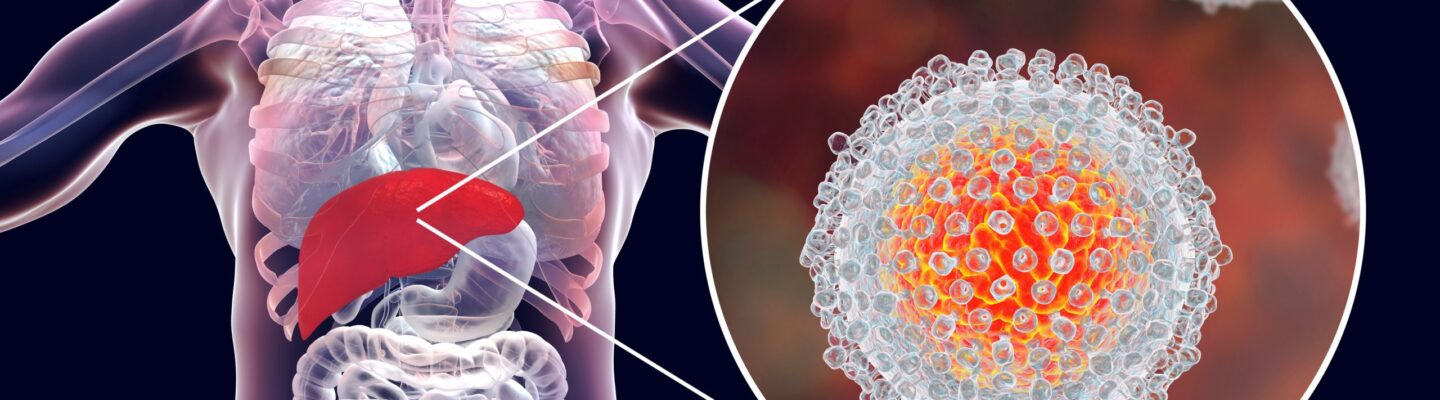
Hepatitis is a condition where the liver becomes inflamed. It comes in multiple types, each with various causes. Hepatitis can stem from viral, bacterial, or parasitic infections. In other cases, it may be caused by heavy alcohol consumption, certain medications or supplements, or autoimmune disorders, where the body mistakenly attacks its own liver cells.
When the liver is affected, some people may show no symptoms. However, if symptoms appear, they can include yellowing of the skin and eyes (jaundice), dark urine, pale or gray stool, fever, abdominal and joint pain, swelling, vomiting, persistent fatigue, drowsiness, and itching. These symptoms occur due to impaired liver function, which disrupts normal body processes.
Treatment depends on the type and severity of hepatitis. Often, medications are given to alleviate symptoms and help manage inflammation. Most patients don’t require hospitalization and can manage the condition with regular follow-ups and medication at home. However, if the hepatitis is severe, hospitalization may be necessary to closely monitor and manage complications, aiming for a more controlled recovery process.
Table of Contents
Symptoms of Hepatitis

Hepatitis presents a variety of symptoms, though the severity and presence of these symptoms can vary widely depending on the type and progression of the disease. While many individuals with hepatitis may experience a mix of signs due to inflammation and impaired liver function, some may notice only mild indicators or none at all in early stages. Below are some of the most common symptoms to look for:
- Yellowing of the Skin and Eyes (Jaundice). High bilirubin in the blood, a liver byproduct, causes yellowing, indicating impaired bile processing and potential liver dysfunction.
- Dark or Deep Yellow Urine. As bilirubin spills into the bloodstream due to liver inflammation, urine may turn unusually dark, reflecting the liver’s inability to filter waste properly.
- Pale or Gray Stool. Inadequate bile flow from the liver affects stool color, making it pale or gray—a clear sign of liver disturbance.
- Fever and Swelling. An inflammatory response in the body can lead to fever and edema, especially in the lower limbs, when the liver is stressed or infected.
- Abdominal and Joint Pain. The liver’s swelling due to hepatitis can cause tenderness in the abdomen, with joint pain often signaling systemic inflammation.
- Vomiting and Diarrhea. Impaired liver function disrupts digestion, often leading to nausea and diarrhea as the body struggles to handle waste and bile properly.
- Fatigue and Drowsiness. With a disrupted metabolism, the body’s energy levels drop significantly, causing persistent tiredness and drowsiness.
- Skin Itching. Accumulation of bile in the bloodstream due to liver issues can lead to persistent itching, a common symptom in advanced liver conditions.
- Loss of Appetite. Liver inflammation and metabolic disturbances commonly suppress appetite, as the body directs energy toward healing.
In mild hepatitis cases, symptoms might only include slight yellowing or be absent altogether. Recognizing these symptoms early on can be crucial for prompt treatment, especially in progressive hepatitis types that can worsen over time. For anyone experiencing multiple symptoms, consulting a healthcare professional is essential to determining the cause and appropriate care.
Types of Hepatitis
Hepatitis is generally categorized as either infectious or non-infectious, with each type arising from different causes and carrying specific risk factors.
Infectious Hepatitis
Infectious hepatitis is caused by viruses, bacteria, or parasites that affect liver function:
- Viral Hepatitis. Hepatitis viruses cause liver inflammation, with each type spreading differently.
- Hepatitis A. Transmitted through contaminated food or water.
- Hepatitis B. Spread via bodily fluids, such as sexual contact or shared needles.
- Hepatitis C. Primarily spreads through blood contact.
- Hepatitis D. Only affects those with HBV, requiring HBV to survive in the body.
- Hepatitis E. Contracted through contaminated water, especially in areas with poor sanitation.
- Bacterial Hepatitis. Bacterial infections such as E. coli and Klebsiella pneumoniae can also inflame the liver.
- Parasitic Hepatitis. Liver inflammation may result from parasitic infections, including protozoa and plasmodium.
Non-Infectious Hepatitis
Non-infectious hepatitis arises from non-infectious causes like lifestyle factors, certain medications, or immune responses:
- Alcoholic Hepatitis. Chronic alcohol consumption can damage liver cells and lead to inflammation.
- Toxin and Drug-Induced Hepatitis. Certain medications, supplements, and toxins can overload and damage the liver, particularly with prolonged or high-dose exposure.
- Autoimmune Hepatitis. An immune system disorder where the body attacks its liver cells, causing chronic inflammation, often due to genetic predisposition.
Each form of hepatitis requires specific preventive, diagnostic, and treatment approaches, emphasizing the importance of understanding the type and source.
Diagnostic Procedures for Hepatitis
Diagnosing hepatitis involves several procedures to determine liver health, identify the type of hepatitis, and assess disease severity. Here’s a more detailed breakdown of the steps commonly involved:
- Physical Examination. A thorough physical exam may reveal signs of hepatitis, such as jaundice (yellowing of the skin and eyes) or tenderness in the upper right abdomen, where the liver is located.
- Blood Tests. Blood tests are central to diagnosing hepatitis and include:
- Liver Function Tests (LFTs). These measure levels of liver enzymes, including ALT (alanine aminotransferase) and AST (aspartate aminotransferase), which are elevated when liver cells are inflamed or damaged.
- Viral Hepatitis Serologies. This testing identifies specific antibodies and antigens to determine the presence of hepatitis viruses like A, B, C, D, and E. For example, detecting HBsAg (hepatitis B surface antigen) indicates an HBV infection.
- Autoimmune Markers. In suspected cases of autoimmune hepatitis, blood tests can measure specific immune markers (e.g., ANA, SMA) to determine if the immune system is attacking liver cells.
- Imaging Studies. Imaging provides detailed views of the liver to assess its size, structure, and any signs of inflammation, scarring, or fat buildup:
- Ultrasound. A common, non-invasive test that can identify liver inflammation, swelling, or fatty deposits.
- CT Scans and MRI. These imaging modalities give more detailed cross-sectional images of the liver, useful for detecting fibrosis (scarring) or other liver structural changes.
- Liver Biopsy. If imaging and blood tests are inconclusive or if there’s a need to assess the extent of liver damage, a biopsy may be performed. During a liver biopsy, a small tissue sample is collected via a needle, typically under ultrasound guidance, and examined microscopically to check for inflammation, fibrosis, or cirrhosis.
Complications of Untreated Hepatitis
Untreated hepatitis can lead to severe complications due to prolonged liver damage. Here are some of the most serious outcomes:
- Chronic Liver Disease. Certain types of hepatitis, especially B and C, can progress to chronic hepatitis, causing long-term liver inflammation and damage.
- Cirrhosis. Persistent inflammation can result in cirrhosis, where the liver becomes scarred, stiff, and struggles to function properly.
- Liver Failure. Extensive damage from cirrhosis or advanced hepatitis may lead to liver failure, necessitating a liver transplant.
- Liver Cancer. Chronic hepatitis significantly raises the risk of hepatocellular carcinoma, a primary liver cancer.
- Portal Hypertension and Variceal Bleeding. Cirrhosis can elevate blood pressure in the portal vein, increasing the risk of potentially fatal bleeding in the esophagus or stomach.
- Other Organ Complications. Severe hepatitis can also lead to kidney dysfunction, hormonal imbalances, and brain complications like hepatic encephalopathy, where toxin buildup affects brain function.
Addressing hepatitis early with appropriate treatment can help prevent these complications and improve long-term liver health.
Causes of Hepatitis

Hepatitis arises from several key causes, grouped into infectious agents, lifestyle factors, and genetic predispositions. Each factor affects liver health differently, with some forms being more easily preventable than others.
- Microbial Infections. The most common infectious causes include viruses (hepatitis A, B, C, D, E), as well as certain bacteria and parasites. Viral hepatitis can spread through contaminated food or water, shared needles, unprotected sex, and contact with infected bodily fluids such as blood, urine, semen, and vaginal secretions. Hepatitis viruses specifically target the liver, causing inflammation and liver cell damage. Bacterial and parasitic infections are rarer but can also lead to liver inflammation when they spread from other parts of the body.
- Excessive Alcohol Consumption. Long-term, heavy alcohol use can cause alcoholic hepatitis, where toxic compounds from alcohol overwhelm the liver’s capacity to filter them out. This leads to liver cell injury, inflammation, and the buildup of scar tissue over time, increasing the risk of cirrhosis. Chronic alcohol use limits the liver’s ability to regenerate, and ongoing damage can lead to liver failure.
- Genetic Factors and Autoimmune Conditions. Certain types of hepatitis, like autoimmune hepatitis, can have genetic origins. In autoimmune hepatitis, the immune system mistakenly attacks liver cells, causing chronic inflammation and damage. This condition often runs in families, and a family history of autoimmune disorders may increase the risk. Lifestyle factors and environmental triggers may also influence the likelihood of developing autoimmune hepatitis, even in those with genetic predispositions.
Understanding these causes is essential for prevention, early diagnosis, and targeted management of hepatitis. Each type poses unique health risks, but many forms can be controlled or prevented with lifestyle modifications, vaccination, and medical care.
Prevention of Hepatitis

Taking proactive steps is essential to minimize the risk of hepatitis, whether through improved hygiene practices or vaccinations. Here are comprehensive strategies to consider:
- Practice Proper Hygiene. Always wash hands with soap before eating, after using the restroom, or touching potentially contaminated surfaces. This limits the spread of bacteria and viruses that may cause hepatitis.
- Ensure Clean Water and Food. Drink only purified or boiled water. Avoid street food unless you’re confident it was prepared in clean conditions, as unfiltered water and unclean food sources are common causes of hepatitis A and E.
- Avoid Raw or Undercooked Foods. Cook meat and seafood thoroughly to kill any harmful microorganisms. Uncooked or undercooked shellfish, particularly from unsanitary sources, is a common source of hepatitis A.
- Caution with Public Dining and Utensils. When dining in public, especially at informal eateries, confirm that utensils and plates are clean. Using disposable cutlery or carrying personal utensils can provide additional protection.
- Avoid Sharing Personal Items. Items like toothbrushes, razors, and nail clippers can carry microscopic blood particles, increasing the risk of viral hepatitis transmission (e.g., hepatitis B and C) through bodily fluids.
- Practice Safe Needle Use. Never reuse or share needles. This applies to both medical syringes and non-medical needles (e.g., in tattooing). Be aware that reusing needles is a significant hepatitis transmission pathway.
- Tattoo and Piercing Safety. Only go to reputable, licensed tattoo parlors or piercing studios with rigorous sterilization practices to prevent hepatitis B or C infection.
- Safe Sexual Practices. Use condoms consistently and discuss health screenings with partners to reduce the risk of sexually transmitted hepatitis (particularly hepatitis B).
- Separate Personal Items for Infected Individuals. In homes with an infected individual, use designated cups, utensils, towels, and personal care items to prevent accidental transmission. Regularly disinfect common areas and ensure others avoid direct contact with contaminated items.
- Vaccination. Get vaccinated against hepatitis A and B if eligible, as these are effective preventive measures. Check vaccination status regularly for family members, especially for children or anyone at increased risk, such as healthcare workers or travelers.
By following these preventive measures, you can reduce the risk of hepatitis and protect both personal and public health.
Risk Factors for Hepatitis

Hepatitis can affect anyone, but certain factors can increase susceptibility. Below are some of the primary risk factors:
- Poor Sanitation. Areas with limited access to sanitation can expose individuals to contaminated water and food, leading to higher hepatitis A and E risks.
- Lack of Clean Water and Food. Contaminated resources are key transmission sources for hepatitis, especially in regions with inadequate sanitation infrastructure.
- Living with Infected Individuals. Sharing a household with someone who has hepatitis, especially hepatitis B or C, raises the risk through contact with bodily fluids.
- Multiple Sexual Partners. High-risk sexual activity increases exposure to hepatitis B and C, particularly without protection.
- Men Who Have Sex with Men. Men engaging in sexual activity with other men have a heightened risk for hepatitis B and C, partly due to increased exposure to bodily fluids.
- Use of Illicit Drugs. Sharing needles or other drug paraphernalia can transmit hepatitis B and C due to blood exposure.
- Travel to High-Risk Regions Without Vaccination. Visiting areas with prevalent hepatitis without vaccination increases exposure risk.
- Eating Raw or Undercooked Seafood. Particularly in areas where water sanitation is poor, raw seafood may carry hepatitis A.
- Improper Handwashing. Consistent hand hygiene reduces contamination risks, a critical factor in hepatitis A prevention.
- Healthcare Occupation. Frequent contact with blood or bodily fluids puts healthcare workers at higher hepatitis exposure risk.
- Tattoos and Piercings. Using unsterilized equipment can lead to hepatitis B or C transmission.
- Nail and Hair Services. Pedicures, manicures, and haircuts at facilities without proper sanitation can increase risk if tools are not sterilized between clients.
- Sharing Personal Items. Items like razors, toothbrushes, and nail clippers may carry small blood traces and increase risk of hepatitis transmission if shared.
Avoiding these risk factors, practicing good hygiene, and seeking vaccination when available can significantly reduce hepatitis risk.
Hepatitis FAQs
Hepatitis is a complex condition, leading many to have questions about its causes, symptoms, treatment, and prevention. This section aims to address common concerns, providing clear and concise answers to help you better understand the condition and its impact on health.
- What is hepatitis?
Hepatitis refers to liver inflammation, often caused by viral infections, excessive alcohol use, toxins, or autoimmune disorders. - How is hepatitis transmitted?
Transmission occurs through contaminated food or water (hepatitis A, E), contact with infected blood (hepatitis B, C, D), unprotected sexual contact, and sharing needles. - Can hepatitis be cured?
Some types, such as hepatitis A and E, often resolve on their own, while others, like hepatitis B and C, can be managed or cured with antiviral therapies. Treatment success varies based on the type and severity. - Who is at higher risk?
Those at higher risk include healthcare workers, travelers to high-risk areas, individuals with multiple sexual partners, people who use injectable drugs, and those who engage in tattooing or piercing with unsterilized equipment. - Can hepatitis be prevented?
Prevention is possible through vaccination (for hepatitis A and B), safe sexual practices, avoiding sharing needles, and maintaining proper hygiene. For those at risk, vaccination is one of the most effective preventive measures. - What are the symptoms of hepatitis?
Symptoms may vary but often include jaundice (yellowing of the skin and eyes), fatigue, abdominal pain, dark urine, pale stool, fever, and loss of appetite. Some individuals may not experience symptoms, especially in early stages. - When should I see a doctor?
You should consult a healthcare professional if you exhibit symptoms of hepatitis or have been exposed to risk factors, such as contaminated food, shared needles, or unprotected sexual contact with an infected person. - Is hepatitis life-threatening?
While some cases resolve without treatment, untreated hepatitis can lead to serious complications such as liver failure, cirrhosis, or liver cancer, especially with chronic hepatitis B or C. - How is hepatitis diagnosed?
Diagnosis typically involves blood tests to check liver function and identify the specific virus, imaging studies such as ultrasound or MRI to assess liver damage, and sometimes a liver biopsy to evaluate the extent of inflammation or scarring. - Are there long-term effects?
Chronic hepatitis, especially B and C, can cause long-term liver damage, leading to cirrhosis, liver failure, or even liver cancer. Early diagnosis and treatment can significantly reduce the risk of these complications.
Understanding the answers to these frequently asked questions can help in making informed decisions about hepatitis prevention, diagnosis, and treatment. If you have more specific concerns, it is always best to seek advice from a healthcare professional.