Summary
Hemochromatosis is a condition characterized by the excessive accumulation of iron in the body. When too much iron builds up, it can poison organs such as the liver, heart, pancreas, and even the joints. If left untreated, this condition can lead to organ failure and pose serious, life-threatening risks to the patient.
Diagnosing hemochromatosis can be challenging because its symptoms often resemble those of other common illnesses. Patients affected by this condition may experience joint pain, extreme fatigue, weakness, unexplained weight loss, and abdominal discomfort.
Hemochromatosis can be inherited, meaning that a person may develop the condition if they inherit the faulty gene from their parents. However, it can also arise as a complication of other health issues like anemia, liver disease, or kidney disease. Frequent blood transfusions can also increase the risk of developing this condition.
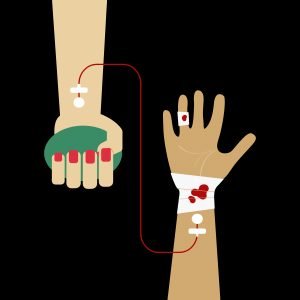
Treatment for hemochromatosis primarily involves phlebotomy, a procedure that removes blood to reduce the body’s iron levels. Patients may also be prescribed medications and given special dietary guidelines to help manage iron intake. Early detection and treatment are essential in preventing the progression of the disease and avoiding serious complications.
Table of Contents
Symptoms of Hemochromatosis
The symptoms of hemochromatosis can often mimic those of other conditions, making it difficult to diagnose in its early stages. However, if a person experiences a combination of the following symptoms, it may be indicative of excessive iron buildup in the body:
- Joint pain. Pain, particularly in the knuckles, is a common early symptom of hemochromatosis, which may later extend to other joints.
- Chronic fatigue. Feeling excessively tired or fatigued even with enough rest is one of the hallmark symptoms of this condition.
- Body weakness. Generalized weakness or lack of physical strength may occur as iron accumulates in muscles and tissues.
- Unexplained weight loss. Individuals with hemochromatosis may lose weight without changes in diet or physical activity.
- Abdominal pain. Discomfort or pain in the upper abdomen, especially around the liver, can signal the liver is being affected by iron overload.
- Loss of libido. Hemochromatosis can interfere with hormone levels, leading to reduced sexual drive in both men and women.
In addition to these symptoms, some individuals may experience skin discoloration, often referred to as “bronzing,” and more advanced cases can lead to conditions like diabetes, heart problems, and liver disease.
To confirm a diagnosis of hemochromatosis, doctors may recommend several diagnostic tests, including blood tests to measure iron levels, DNA testing to identify genetic mutations, and liver biopsy to assess the extent of liver damage. Early detection is crucial to managing symptoms and preventing complications.
Types of Hemochromatosis
There are two main types of hemochromatosis: primary and secondary hemochromatosis. The key differences between these two types are outlined below:
- Primary Hemochromatosis. This type is hereditary and is passed down through families. If one or both parents carry the faulty genes, there is a chance their children may inherit the condition. Primary hemochromatosis is caused by genetic mutations, particularly in the HFE gene, which affects how the body regulates iron absorption. It is the most common form of the condition.
- Secondary Hemochromatosis. This type is not inherited but develops as a complication of other health conditions. Diseases such as anemia, liver disease, or kidney disease can lead to excessive iron buildup in the body. Additionally, individuals who frequently undergo blood transfusions are at higher risk of developing secondary hemochromatosis because the body cannot efficiently eliminate the extra iron introduced through the transfusions.
Understanding the type of hemochromatosis is crucial for determining the appropriate treatment approach, as primary hemochromatosis is managed differently from secondary cases, which require addressing the underlying health issues.
Diagnostic Procedures for Hemochromatosis
Diagnosing hemochromatosis can be challenging due to the non-specific nature of its symptoms, which often resemble other conditions. To confirm the diagnosis and determine the severity of iron overload, several diagnostic tests and procedures are commonly used:
- Blood Tests.
- Serum Ferritin Test. This test measures the level of ferritin, a protein that stores iron in the body. Elevated ferritin levels may indicate iron overload, which is a key marker of hemochromatosis.
- Transferrin Saturation Test. This test assesses how much iron is bound to transferrin, a protein that carries iron through the blood. A high transferrin saturation level suggests that the body is absorbing too much iron.
- Total Iron-Binding Capacity (TIBC). This test evaluates how well iron is being transported in the blood, helping to confirm iron overload.
- Genetic Testing. Since primary hemochromatosis is hereditary, a DNA test can identify mutations in the HFE gene, particularly the C282Y and H63D variants, which are responsible for most cases of hereditary hemochromatosis. Genetic testing is useful for confirming a diagnosis and identifying family members who may be at risk.
- Liver Function Tests (LFTs). These tests assess how well the liver is functioning. Since the liver is one of the primary organs affected by iron overload, abnormal liver enzyme levels may indicate liver damage due to hemochromatosis.
- Liver Biopsy. In some cases, doctors may recommend a liver biopsy to determine the extent of iron buildup and liver damage. A small sample of liver tissue is taken and analyzed under a microscope to assess the level of scarring (fibrosis) or cirrhosis caused by iron overload.
- Magnetic Resonance Imaging (MRI). An MRI scan provides a non-invasive way to measure iron levels in the liver and other organs. It helps determine the severity of iron buildup without needing to perform a biopsy.
- Electrocardiogram (ECG) and Echocardiogram. Since iron overload can affect the heart, these tests may be used to evaluate heart function and detect any signs of heart damage, such as arrhythmias or cardiomyopathy, in individuals with advanced hemochromatosis.
By combining these diagnostic procedures, doctors can confirm whether a patient has hemochromatosis, assess the degree of iron overload, and determine if any organs have been damaged. Early diagnosis is essential for preventing complications and managing the condition effectively.
Complications of Untreated Hemochromatosis
If hemochromatosis is left untreated, the excess iron buildup in the body can lead to serious, potentially life-threatening complications. Over time, this iron overload can damage various organs and tissues, resulting in long-term health problems. Some of the key complications include:
- Liver Damage (Cirrhosis and Liver Cancer). The liver is one of the primary organs affected by iron overload. Over time, untreated hemochromatosis can lead to cirrhosis, or scarring of the liver, which impairs liver function. Cirrhosis also increases the risk of developing liver cancer.
- Heart Problems. Excess iron can accumulate in the heart, leading to conditions like cardiomyopathy (thickening or weakening of the heart muscles), arrhythmias (irregular heartbeats), and heart failure. If the heart becomes unable to pump blood efficiently, it can lead to life-threatening complications.
- Diabetes (Bronze Diabetes). Iron buildup in the pancreas can impair insulin production, leading to diabetes. In severe cases, a distinctive form of the condition known as bronze diabetes can develop, named after the skin discoloration often seen in advanced hemochromatosis.
- Arthritis and Joint Damage. Iron can deposit in the joints, causing arthropathy (joint disease), leading to joint pain, stiffness, and swelling. The most commonly affected joints are those in the hands, particularly the knuckles.
- Hormonal Imbalances. Iron accumulation in the pituitary gland can affect hormone regulation, causing hypogonadism (reduced function of the testes or ovaries). This can result in a loss of libido, impotence in men, irregular menstrual cycles in women, and even infertility.
- Skin Discoloration. One of the noticeable signs of advanced hemochromatosis is skin bronzing, a grayish or bronze tint to the skin caused by excess iron deposits in the skin cells.
- Liver Failure. If cirrhosis progresses, it can lead to liver failure, where the liver can no longer perform its essential functions, such as filtering toxins, producing proteins, and managing nutrients. Liver failure is a life-threatening condition that often requires a liver transplant.
- Increased Risk of Infections. People with hemochromatosis are at a higher risk for certain infections, particularly those caused by iron-loving bacteria, such as Vibrio vulnificus (a bacterium found in seafood and seawater), which can lead to severe, rapidly progressing infections.
The complications of untreated hemochromatosis can be severe, but early diagnosis and treatment can prevent or significantly reduce the risk of these outcomes. Regular blood monitoring, medical interventions like phlebotomy (blood removal), and lifestyle adjustments can help manage iron levels and protect vital organs from damage.
Causes of Hemochromatosis
Hemochromatosis occurs when the body accumulates excess iron, which it is unable to properly process or eliminate. This excess iron can build up in various organs and tissues, leading to toxicity and damage. The main causes of hemochromatosis include:
- Inherited faulty gene. The primary cause of hemochromatosis is a genetic mutation inherited from parents. When both parents carry a defective gene, there is a high likelihood that their children will develop the condition. This form of the disease is known as primary (hereditary) hemochromatosis, and it’s most commonly caused by mutations in the HFE gene. The most common mutations linked to hemochromatosis are C282Y and H63D.
- Anemia-related iron overload. Although anemia typically involves a deficiency in red blood cells or iron, certain types of anemia can lead to iron overload, especially when inflammation is present. In cases of chronic anemia, the body tries to absorb more iron to compensate, but if the underlying condition involves inflammation, the body may be unable to use the stored iron properly, leading to an accumulation.
- Liver disease. Liver conditions, such as cirrhosis or hepatitis, impair the liver’s ability to process and eliminate excess minerals like iron. When the liver is damaged, it can no longer effectively remove iron from the bloodstream, which can lead to iron overload and eventually hemochromatosis.
- Kidney disease. In severe cases of kidney disease, especially in patients undergoing dialysis, the body’s ability to regulate and eliminate minerals like iron becomes compromised. The inability to remove iron effectively can result in iron overload and increase the risk of developing hemochromatosis.
- Frequent blood transfusions. Blood transfusions are rich in iron, and individuals who frequently undergo transfusions for conditions such as sickle cell disease or thalassemia are at higher risk of iron overload. This condition, known as secondary hemochromatosis, occurs because the body is unable to eliminate the extra iron from the transfused blood, leading to its buildup over time.
In addition to these causes, conditions that affect the body’s iron regulation mechanisms or treatments that involve the regular introduction of iron-rich materials (such as blood) can increase the risk of hemochromatosis. Understanding these causes is essential for early diagnosis and effective management of the disease.
Prevention of Hemochromatosis
While hereditary hemochromatosis cannot be prevented due to its genetic nature, there are steps that can be taken to reduce the risk of developing secondary hemochromatosis, which occurs as a result of other health conditions or treatments. Here are some preventive measures:
- Exercise regularly. Engaging in daily exercise helps maintain good blood circulation and overall cardiovascular health. Regular physical activity can reduce the risk of developing blood-related disorders, which can lead to secondary hemochromatosis.
- Take care of your liver. Since liver disease can lead to iron overload, it is essential to prioritize liver health. Avoid excessive alcohol consumption and limit the intake of fatty foods, as these can damage the liver over time. Maintaining a healthy liver can help prevent conditions that may contribute to iron buildup in the body.
- Maintain kidney health. Keeping your kidneys healthy can help prevent iron overload. Drink plenty of water to support proper kidney function and to help flush out toxins and waste products through urination. This also reduces the risk of urinary tract infections and helps keep the kidneys functioning efficiently. Additionally, avoid consuming excessive amounts of salty foods, which can strain the kidneys.
- Use iron and vitamin C supplements with caution. If you take iron or vitamin C supplements, follow the recommended dosage carefully. Avoid taking more than the prescribed amount, as excessive intake can lead to an overload of iron in the body. Vitamin C can enhance iron absorption, so it is important not to exceed the advised dosage of these supplements.
By adopting a healthy lifestyle and taking preventive measures to protect the liver, kidneys, and blood health, the risk of developing secondary hemochromatosis can be minimized. Proper management of any underlying conditions, such as liver or kidney disease, is also key to avoiding complications related to iron overload.
Risk Factors for Hemochromatosis
Hemochromatosis can potentially affect anyone, but certain factors can increase the likelihood of developing the condition. These key risk factors include:
- Race or ethnicity. Hemochromatosis is more common in individuals of Caucasian and Northern European descent. It is less frequently seen in African-American, Hispanic, Asian, and American Indian populations.
- Gender. Studies show that men are more commonly affected by primary hemochromatosis than women. However, women may still develop the condition, particularly after menopause, when they stop losing iron through menstruation.
- Age. While hemochromatosis can occur in younger individuals, the likelihood increases with age, particularly between the ages of 40 to 60. This is because iron accumulates gradually over time, and symptoms often appear later in life as iron levels become excessive.
- Family history of hemochromatosis. If one or both parents have hemochromatosis, there is a higher chance that their children may inherit the faulty gene responsible for this condition, significantly increasing their risk of developing the disorder.
- Excessive alcohol consumption. Heavy drinking can damage the liver, impairing its ability to filter out excess iron from the body. This can worsen the iron overload associated with hemochromatosis, particularly in individuals who are genetically predisposed to the condition.
Recognizing these risk factors can help in the early detection and management of hemochromatosis, especially for those with a family history or higher susceptibility due to ethnicity or lifestyle factors like alcohol consumption. Regular health check-ups and screening are essential for individuals at risk.
Hemochromatosis FAQs
Here are some frequently asked questions about hemochromatosis, its causes, symptoms, and management:
- What is hemochromatosis?
Hemochromatosis is a condition where the body absorbs and stores too much iron. This excess iron builds up in organs such as the liver, heart, pancreas, and joints, potentially causing damage if not managed properly. - What causes hemochromatosis?
The primary cause of hemochromatosis is a genetic mutation that affects how the body regulates iron absorption. This is known as primary hemochromatosis and is inherited from one or both parents. Secondary hemochromatosis can develop as a result of other conditions, such as anemia, liver disease, or frequent blood transfusions. - What are the symptoms of hemochromatosis?
Symptoms of hemochromatosis often develop slowly and may resemble those of other conditions. Common symptoms include joint pain, chronic fatigue, weakness, abdominal pain, unintentional weight loss, and loss of libido. In advanced cases, it can lead to liver disease, diabetes, or heart problems. - How is hemochromatosis diagnosed?
Hemochromatosis is diagnosed through blood tests that measure serum ferritin (iron storage) and transferrin saturation (how much iron is carried in the blood). Genetic testing can confirm the presence of mutations in the HFE gene, which is linked to hereditary hemochromatosis. In some cases, a liver biopsy or MRI may be used to assess iron levels in the liver. - Can hemochromatosis be treated?
Yes, the main treatment for hemochromatosis is phlebotomy (regular blood removal), which helps reduce iron levels in the body. Patients may also be advised to avoid iron supplements, limit alcohol intake, and make dietary changes. In some cases, medications like iron chelators are prescribed to help the body eliminate excess iron. - Is hemochromatosis life-threatening?
If diagnosed early and managed properly, hemochromatosis is not usually life-threatening. However, if left untreated, it can cause serious complications, including liver disease (cirrhosis), heart problems, diabetes, and joint damage. - Who is at risk for hemochromatosis?
Individuals with a family history of hemochromatosis, especially those of Northern European descent, are at higher risk. Men are more likely to develop symptoms earlier than women, as women naturally lose iron through menstruation before menopause. - Can hemochromatosis be prevented?
While hereditary hemochromatosis cannot be prevented, secondary hemochromatosis can be minimized by managing underlying health conditions, avoiding excessive iron or vitamin C supplements, and reducing alcohol intake, which can damage the liver. - Can diet help manage hemochromatosis?
Yes, dietary management is important for people with hemochromatosis. Patients are usually advised to avoid iron-rich foods (especially red meat), limit vitamin C intake (as it enhances iron absorption), and avoid alcohol. Regular blood donation through phlebotomy is also an effective way to reduce iron levels. - When should I see a doctor for hemochromatosis?
If you have a family history of hemochromatosis or experience symptoms such as unexplained fatigue, joint pain, or skin discoloration, it’s important to see a doctor. Early diagnosis and treatment can prevent serious complications.
These FAQs provide an overview of key concerns about hemochromatosis, from its causes to treatment options. If you suspect you may have hemochromatosis, consulting with a healthcare provider for proper testing and guidance is essential.


