 Image Source: toxtutor.nlm.nih.gov
Image Source: toxtutor.nlm.nih.gov
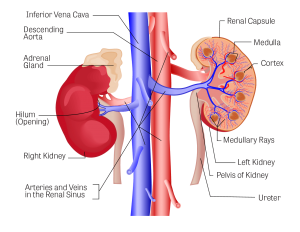
Kidney disease is one of the leading causes of death in the Philippines, reflecting the vital role the kidneys play in maintaining overall health. The kidneys are part of the urinary system, which includes the ureters, bladder, and urethra. Together, these organs help the body remove waste through urine.
The primary function of the kidneys is to filter waste and excess fluids from the blood to produce urine. They also regulate the balance of important minerals such as sodium, potassium, and phosphorus, help control blood pressure through the production of the enzyme renin, and stimulate red blood cell production with the hormone erythropoietin. Additionally, the kidneys activate vitamin D to support healthy bones.
Because the kidneys perform many critical functions, they are susceptible to damage from various causes. Unhealthy lifestyle choices, such as smoking, excessive alcohol consumption, and a diet high in salt and fat, can increase the risk of kidney disease. Complications from other medical conditions can also lead to kidney problems.
When kidney function becomes impaired, it can lead to a range of symptoms such as fatigue, swelling, changes in urine output, and difficulty regulating fluid levels in the body. Depending on the severity of the condition, treatment options may include medications, dialysis, or a kidney transplant.
They are part of the urinary system, which also includes the ureters, bladder, and urethra. Together, these organs play a crucial role in filtering waste and maintaining the body’s fluid and chemical balance.
The kidneys’ primary function is to filter waste products and excess fluid from the blood to form urine. Blood enters the kidneys through the renal arteries, where millions of tiny filtering units called nephrons work to remove toxins, excess salts, and water. This filtered waste, in the form of urine, then flows through the ureters to the bladder, where it is stored until excretion.
Beyond waste filtration, the kidneys perform several other essential functions. They regulate the levels of important electrolytes such as sodium, potassium, and calcium in the blood, ensuring proper nerve and muscle function. The kidneys also help maintain the body’s acid-base balance, which is crucial for keeping pH levels within a healthy range.
The kidneys are also vital in managing blood pressure. They produce an enzyme called renin, which helps regulate blood pressure by controlling fluid balance and blood vessel constriction. Additionally, the kidneys produce a hormone called erythropoietin (EPO), which signals the bone marrow to create red blood cells, ensuring that enough oxygen is delivered to tissues throughout the body.
Another important function of the kidneys is activating vitamin D, which is necessary for the absorption of calcium from food. This process supports healthy bones and prevents conditions like osteoporosis.
When the kidneys are unable to perform their filtering function properly, waste and fluids build up in the body, leading to a variety of health problems. Early signs of kidney dysfunction may include changes in urination, swelling in the legs, fatigue, and high blood pressure. As kidney function continues to decline, more severe symptoms like anemia, electrolyte imbalances, and bone disorders may occur.
If left untreated, kidney disease can progress to kidney failure, also known as end-stage renal disease (ESRD). At this stage, the kidneys can no longer filter waste effectively, and treatment options like dialysis or a kidney transplant are needed to maintain life.
Although the body can function with just one kidney, or with reduced kidney function, maintaining healthy kidneys is essential for overall well-being. Regular checkups, managing conditions like diabetes and high blood pressure, staying hydrated, and maintaining a balanced diet are key steps in protecting kidney health.
The kidneys can develop various types of diseases. While there are many forms of kidney disease, there are common symptoms that patients may experience, such as the following:
Understanding these common symptoms can help individuals recognize the early signs of kidney disease. Early detection and treatment are essential for preventing further complications and maintaining kidney health.
Below are the types of kidney diseases and conditions affecting the urinary system, listed alphabetically:
Kidney disease can take many forms and affect individuals of any age or background. While some conditions are rare or genetic, many are preventable with a healthy lifestyle and regular medical checkups. Early detection and prompt treatment are key to managing kidney disease and preventing complications. By understanding the various types of kidney diseases and their potential impact, individuals can take proactive steps to protect their kidney health and improve their overall quality of life.
Diagnosing kidney disease involves several tests and evaluations to assess kidney function, identify potential damage, and determine the underlying cause. Early detection is crucial to managing kidney disease effectively and preventing further complications. Below are the common diagnostic procedures used to evaluate kidney health:
In a kidney biopsy, a small sample of kidney tissue is taken and examined under a microscope. This procedure is typically used when the cause of kidney disease is unclear or when more specific information about the extent of damage is needed. It helps diagnose conditions such as glomerulonephritis or lupus nephritis.
GFR can be estimated through blood tests, but certain specialized tests may also be performed to measure the rate at which the kidneys filter blood. This helps in staging chronic kidney disease and deciding on the appropriate treatment.
For patients with a family history of kidney disease or conditions like polycystic kidney disease (PKD), genetic testing can help identify inherited disorders that may affect kidney function.
Timely diagnosis of kidney disease is essential to preventing irreversible damage and improving outcomes. With a combination of blood tests, urine analysis, imaging, and, when necessary, biopsy, doctors can accurately assess kidney health and develop a suitable treatment plan. Regular checkups and early intervention are key to managing kidney disease effectively.
Untreated kidney disease can lead to a range of severe and potentially life-threatening complications. Early detection and treatment are crucial to preventing these outcomes. Below are the most common complications associated with untreated kidney disease:
Chronic kidney failure, or end-stage renal disease (ESRD), occurs when the kidneys lose the ability to filter waste and fluids effectively. At this stage, the kidneys can no longer support the body’s needs, requiring dialysis or a kidney transplant to sustain life. Without treatment, ESRD is fatal, as waste and toxins build up to dangerous levels in the body.
Kidney disease significantly increases the risk of cardiovascular problems such as heart attack, stroke, and heart failure. Damaged kidneys cause high blood pressure and fluid retention, which strain the heart and blood vessels. Cardiovascular disease is one of the leading causes of death in patients with chronic kidney disease.
When the kidneys fail to remove excess fluid, it accumulates in the body, leading to swelling (edema) in the legs, ankles, feet, and even the face. In severe cases, fluid can build up in the lungs, causing pulmonary edema, which makes breathing difficult and can be life-threatening.
Untreated kidney disease often leads to uncontrolled high blood pressure, which further damages the kidneys in a vicious cycle. Hypertension can lead to other serious health problems, including heart disease, stroke, and worsening kidney function. Managing blood pressure is essential to slowing the progression of kidney disease.
Kidneys produce the hormone erythropoietin (EPO), which signals the body to produce red blood cells. Damaged kidneys produce less EPO, leading to anemia—a condition where the body lacks sufficient red blood cells to carry oxygen. Anemia causes fatigue, weakness, and shortness of breath, greatly reducing a person’s quality of life.
Kidney disease affects the body’s ability to regulate calcium and phosphorus levels, leading to weakened bones (renal osteodystrophy). This can result in bone pain, fractures, and an increased risk of osteoporosis. Over time, untreated bone disease can lead to chronic pain and mobility issues.
Healthy kidneys balance electrolytes in the body, such as potassium, sodium, and phosphorus. When kidney function is compromised, dangerous imbalances can occur. For example, high potassium levels (hyperkalemia) can cause irregular heartbeats, leading to heart failure or sudden cardiac arrest.
Uremia occurs when the kidneys are no longer able to filter out waste products, leading to the accumulation of toxins in the bloodstream. Symptoms include nausea, vomiting, fatigue, confusion, and itching. Without treatment, uremia can lead to seizures, coma, and death, making it a medical emergency that often requires dialysis.
People with kidney disease are more susceptible to infections due to a weakened immune system. Infections, such as urinary tract infections (UTIs) or sepsis, can spread quickly and become life-threatening if not treated promptly, especially in patients undergoing dialysis.
Untreated kidney disease leads to serious complications that affect not only the kidneys but also the heart, bones, immune system, and overall well-being. Many of these complications are life-threatening and require immediate medical intervention. Early detection and treatment of kidney disease can help prevent these complications, preserve kidney function, and improve quality of life.
Kidney disease can develop due to a variety of factors, many of which are related to lifestyle, existing medical conditions, or even genetics. Below are the most common causes:
An unhealthy lifestyle is one of the primary contributors to kidney disease. Habits that are particularly harmful to the kidneys include:
Kidney disease can also result from other medical conditions or health issues, including:
Prolonged use of certain medications can damage the kidneys over time, not just the liver. Medications that are particularly harmful to kidney health include:
Kidney damage can occur due to accidents or physical trauma. Burns, stab wounds, or even complications from surgery can lead to kidney injuries, which may cause long-term damage or kidney disease.
Kidney disease can also be hereditary. Some of the common genetic conditions affecting the kidneys include:
In some cases, individuals are born with kidney problems due to poor nutrition during fetal development. Babies can be born with only one functioning kidney, kidneys that do not function properly, or kidneys that are positioned lower than normal, which may impair their function.
Recognizing these risk factors is essential for both preventing and managing kidney disease. Maintaining a healthy lifestyle and monitoring existing medical conditions can reduce the likelihood of kidney problems and promote long-term kidney health.
Here are the common medications prescribed by doctors to relieve the symptoms of kidney disease:
These medications are used to lower the patient’s blood pressure, which helps prevent further damage to the kidneys.
Diuretics help the body expel excess fluid by increasing urination, which is crucial for patients with kidney disease who may retain water.
EPO is a hormone that should normally be produced by the kidneys. If the kidneys are damaged, artificial EPO injections may be needed to stimulate the production of new red blood cells.
This vaccine is commonly given to patients undergoing dialysis to protect them from hepatitis B, a liver disease that dialysis patients may be more susceptible to.
Iron supplements are prescribed to prevent anemia, which occurs when the patient’s body lacks enough red blood cells.
Phosphate binders help prevent the weakening of bones by reducing phosphate levels in the blood. They also help alleviate symptoms like itching and muscle weakness.
This is often given to prevent complications in the heart by balancing the body’s acid levels.
Statins help lower cholesterol levels in the body, reducing the risk of heart-related complications that often accompany kidney disease.
Patients with kidney disease often have weak bones. Doctors may prescribe vitamin D supplements to strengthen the bones and support overall bone health.
In addition to these medications, patients with more severe conditions may require the following treatments:
Hemodialysis, commonly known as dialysis, uses a machine to filter and clean the blood when the kidneys can no longer perform this function. This procedure is typically done three times a week, depending on the patient’s condition, with each session lasting about four hours.
This type of dialysis is performed more quickly than hemodialysis. Instead of using a machine, a tube is inserted into the patient’s abdominal cavity (peritoneal cavity), where a cleansing fluid called dialysate is passed through. The blood is then cleaned inside the body without the need for an external machine.
If a suitable donor is found, the patient may undergo a kidney transplant. This surgery involves replacing the damaged kidney with a healthy one. It is important to note that a person can live with just one functioning kidney.

Kidney disease is often considered a lifestyle-related illness, meaning it can be largely attributed to unhealthy habits and behaviors. To reduce the risk of developing kidney disease, it’s essential to adopt a healthy lifestyle. Below are some recommendations:
Smoking is a significant risk factor for kidney disease. It damages blood vessels and reduces blood flow to the kidneys, impairing their ability to function properly. Quitting smoking can significantly improve kidney health and overall well-being.
Excessive alcohol intake can lead to dehydration, raise blood pressure, and damage the kidneys over time. Reducing alcohol consumption helps maintain the balance of fluids in the body and prevents kidney strain.
Aim for at least 30 minutes of physical activity each day. Regular exercise helps maintain healthy blood pressure, supports heart health, and promotes overall kidney function. Activities like brisk walking, swimming, or cycling can be effective.
High-sodium and high-fat diets contribute to high blood pressure and cholesterol levels, both of which can lead to kidney disease. Opt for a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Limit processed foods, which are often high in salt and unhealthy fats.
Being overweight or obese increases the risk of kidney disease, particularly if it leads to other conditions like diabetes or hypertension. Keeping your weight in check through a balanced diet and regular exercise helps reduce this risk.
High blood pressure is one of the leading causes of kidney disease. Regular monitoring and managing your blood pressure through lifestyle changes or prescribed medications can help protect your kidneys from damage.
Drinking adequate water supports kidney function by helping flush out toxins and waste products. However, avoid overhydration, which can stress the kidneys. The right amount of water intake depends on individual needs, so it’s best to consult a doctor.
If you experience any symptoms of kidney disease, such as swelling, changes in urine, or persistent fatigue, consult a doctor immediately. Early detection is key to preventing further complications. For more specialized care, consult a nephrologist, a doctor who specializes in kidney health.
By incorporating these healthy habits into your daily routine, you can significantly lower your risk of developing kidney disease. Prevention starts with taking control of your health and making mindful lifestyle choices that support kidney function.
Several factors can increase the likelihood of developing kidney disease. These include:
As people age, the kidneys become more fragile, making it harder for them to function properly. This increases the risk of kidney disease in older adults.
Children are also at risk for kidney disease, particularly infections. This is often due to holding in urine or consuming too much salty food or junk food, which can strain the kidneys.
Research shows that certain ethnic groups, such as African-Americans, Native Americans, and Asians, are more likely to develop kidney disease.
Diabetes and high blood pressure are the leading causes of kidney disease. If these conditions are not managed well, they often result in complications, including kidney problems.
People with heart disease are also at a higher risk of developing kidney disease. Heart problems can reduce blood flow, oxygen, and nutrients to the kidneys, impairing their function.
Individuals who lead unhealthy lifestyles are more likely to experience kidney disease. This includes those who are overweight, consume salty and fatty foods, smoke, drink alcohol excessively, and do not exercise regularly.
Having a family history of kidney disease also increases the likelihood of developing the condition.
Recognizing these risk factors is important for taking preventive measures and adopting lifestyle changes that can protect kidney health. Regular checkups and managing underlying conditions like diabetes or high blood pressure are crucial steps in reducing the risk of kidney disease.
This article was written by Mediko.PH staff under the medical supervision and review of Dr. Anthony C. So, BSPT, MD, FPARM. This article is intended to provide accurate and reliable health-related information. However, this is not official and personalized medical advice, nor is it a diagnosis or prescription. Readers are advised to consult a doctor for proper care.