Summary
Pulmonary stenosis, or pulmonary valve stenosis, is a heart condition where the pulmonary valve becomes thickened or stiff, restricting blood flow from the right ventricle to the pulmonary artery. This valve controls the flow of blood from the heart to the lungs, and when it narrows, the heart has to work harder to pump blood through, which can strain the right ventricle over time.
Symptoms of pulmonary stenosis include shortness of breath, chest pain, fatigue, dizziness, fainting, and a distinctive “whooshing” sound, known as a heart murmur. These symptoms arise because the pulmonary artery, responsible for transporting blood to the lungs, receives insufficient blood flow.
Pulmonary stenosis is most often congenital, meaning it’s a defect present at birth, but in rare cases, it may develop due to conditions like carcinoid syndrome or rheumatic fever. Treatment options include medications to reduce the heart’s workload, or in severe cases, surgical interventions like valve repair or replacement, or a balloon valvuloplasty to widen the narrowed valve and improve blood flow.
Table of Contents
Symptoms of Pulmonary Stenosis
Pulmonary stenosis can present with a variety of symptoms, especially as the heart and lungs struggle to manage restricted blood flow. Common signs of this condition include:
- Shortness of breath. With pulmonary stenosis, less blood reaches the lungs via the pulmonary artery. Since this artery is responsible for transporting blood to the lungs for oxygenation, restricted flow impacts the patient’s ability to breathe efficiently.
- Chest pain. Patients with pulmonary stenosis may experience chest pain, often due to the heart working harder than usual or from a reduced oxygen supply to the heart and lungs.
- Severe fatigue. Although the heart pumps faster in response to stenosis, the restricted valve limits blood flow. As a result, body cells receive less oxygen and nutrients, leading to significant fatigue and reduced energy levels.
- Dizziness or fainting. Pulmonary stenosis can also affect the brain, as reduced blood and oxygen flow may cause dizziness and, in severe cases, lead to fainting spells.
- Heart murmur. A heart murmur, described as a “whooshing” sound, may be detected in patients with pulmonary stenosis. This sound occurs as blood flows through the narrowed valve and can be heard through a stethoscope.
If a patient displays these symptoms, pulmonary stenosis may be suspected, and further medical evaluation is essential for proper diagnosis and treatment.
Types of Pulmonary Stenosis
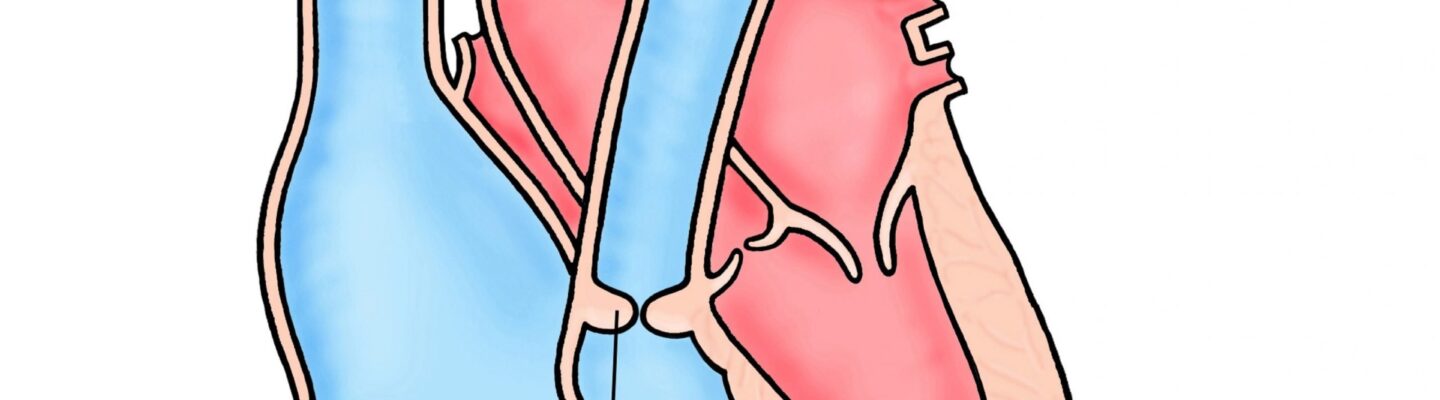
To understand the types of pulmonary stenosis, it’s helpful to first know the function of the pulmonary valve. Located between the right ventricle and the pulmonary artery, the pulmonary valve regulates blood flow from the heart to the lungs. It consists of two leaflets that open and close like a swing-type door, allowing blood to flow smoothly when functioning properly.
When these leaflets or the muscles surrounding the pulmonary valve encounter issues, it can lead to various forms of pulmonary stenosis:
- Valvar pulmonary stenosis. This is the most common type of pulmonary stenosis. In this form, the structure of the pulmonary valve becomes dome-shaped, causing the leaflets to almost fuse together. This narrowing restricts blood flow from the right ventricle to the pulmonary artery, increasing the heart’s workload.
- Subvalvular pulmonary stenosis. In subvalvular pulmonary stenosis, the muscle tissue beneath the pulmonary valve thickens, particularly around the right ventricle. This thickening creates an obstruction just below the valve, restricting blood flow and forcing the heart to pump harder.
- Supravalvular pulmonary stenosis. This type occurs when the area above the pulmonary valve, near the pulmonary artery, thickens. This narrowing above the valve creates resistance, limiting blood flow from the heart to the lungs.
Although each type of pulmonary stenosis affects a different area of the pulmonary valve or its surrounding structures, the symptoms are generally similar across types. However, the severity of the condition depends on the extent of narrowing, which determines how restricted the blood flow is.
Diagnostic Procedures for Pulmonary Stenosis
Diagnosing pulmonary stenosis requires a combination of physical examinations, imaging studies, and specific tests to assess the heart’s structure and blood flow. These diagnostic procedures help confirm the condition and determine its severity.
- Physical examination and heart auscultation. During a physical exam, a healthcare provider listens for a heart murmur, a common indicator of pulmonary stenosis. A murmur, or “whooshing” sound, often occurs as blood flows through the narrowed pulmonary valve.
- Echocardiogram. This ultrasound test is one of the most reliable tools for diagnosing pulmonary stenosis. An echocardiogram provides real-time images of the heart, allowing doctors to measure the valve’s thickness, check for narrowing, and evaluate blood flow across the pulmonary valve. Doppler echocardiography, which assesses blood flow, can determine the severity of stenosis.
- Electrocardiogram (ECG). An ECG records the heart’s electrical activity, helping to detect any irregularities or enlargement in the right side of the heart that could result from pulmonary stenosis.
- Chest X-ray. A chest X-ray may reveal an enlarged right ventricle or pulmonary artery, both of which can indicate the heart’s response to pulmonary stenosis. It also provides a general view of the heart and lungs to help rule out other conditions.
- Cardiac catheterization. In more complex cases, cardiac catheterization may be performed to measure blood pressure within the heart and pulmonary artery. During this procedure, a thin tube is threaded through a blood vessel to the heart to measure pressure and assess blood flow, confirming the severity of the stenosis.
- Magnetic Resonance Imaging (MRI). In some cases, an MRI is used to obtain detailed images of the heart, providing further information on the structure and function of the pulmonary valve, right ventricle, and pulmonary artery.
These diagnostic tools allow healthcare providers to assess the degree of narrowing in the pulmonary valve and make informed decisions about appropriate treatment options. Early diagnosis is essential for effective management and to prevent complications associated with pulmonary stenosis.
Complications of Untreated Pulmonary Stenosis
When left untreated, pulmonary stenosis can lead to a variety of serious complications, as the heart must work harder to pump blood through the narrowed pulmonary valve. Over time, this extra strain can cause further health problems. Here are some of the potential complications:
- Right ventricular hypertrophy. As the right ventricle works harder to push blood through the narrowed valve, its muscle walls thicken. This condition, known as right ventricular hypertrophy, can eventually lead to reduced heart function and increase the risk of heart failure.
- Heart failure. Chronic pressure overload on the right side of the heart can result in heart failure. In this case, the heart can no longer pump blood efficiently, leading to symptoms like shortness of breath, fatigue, fluid retention in the legs and abdomen, and swelling.
- Arrhythmias. The extra strain on the heart caused by pulmonary stenosis can lead to arrhythmias, or irregular heart rhythms. Severe arrhythmias can reduce the heart’s efficiency, leading to fainting spells, dizziness, or even sudden cardiac arrest in extreme cases.
- Cyanosis (low oxygen levels). In severe cases, the reduced blood flow to the lungs can result in low blood oxygen levels, causing a bluish tint to the skin, lips, and fingernails. Cyanosis indicates that oxygen supply to body tissues is inadequate, which can impact organ function.
- Infective endocarditis. Pulmonary stenosis increases the risk of infective endocarditis, a bacterial infection of the heart lining and valves. When blood flow is altered, bacteria are more likely to adhere to the valve, potentially causing life-threatening complications if not treated promptly.
- Exercise intolerance. Due to reduced blood flow and oxygen supply, individuals with untreated pulmonary stenosis may struggle to tolerate physical activities. This can lead to diminished quality of life, as even light exertion can cause fatigue, breathlessness, or chest pain.
The complications associated with untreated pulmonary stenosis can greatly impact both heart health and overall well-being. Timely diagnosis and treatment are essential for preventing these complications and ensuring optimal long-term health outcomes.
Causes of Pulmonary Stenosis
Pulmonary stenosis occurs when the pulmonary valve, which regulates blood flow from the right ventricle to the pulmonary artery, becomes thickened, stiff, or otherwise obstructed. Here are the main direct causes of this condition:
- Congenital malformation of the pulmonary valve. The most common cause of pulmonary stenosis is a congenital heart defect where the pulmonary valve does not form correctly during fetal development. This malformation can result in a valve that has only one or two leaflets (instead of the usual three) or is misshapen in a way that restricts blood flow. Such structural defects in the valve directly cause narrowing, limiting the blood’s passage from the heart to the lungs and putting extra strain on the right ventricle.
- Thickening of the valve tissue. In some cases, the tissue of the pulmonary valve becomes abnormally thick. This thickening (fibrosis) causes the valve to become stiff and less flexible, reducing its ability to open fully during each heartbeat. The narrowed valve opening restricts blood flow and forces the right ventricle to work harder to push blood through, directly leading to the symptoms of pulmonary stenosis.
- Fusion of the valve leaflets. Another direct cause is the fusion or partial fusion of the valve leaflets (the flaps that open and close to regulate blood flow). When the leaflets are fused together, the valve cannot open completely, creating a restricted passageway for blood. This fusion can occur due to developmental abnormalities in the heart or from scarring of the valve tissue.
- Damage from carcinoid syndrome. In rare cases, pulmonary stenosis can result from carcinoid syndrome, a condition in which hormone-like substances released by carcinoid tumors cause fibrosis and thickening of heart valves, including the pulmonary valve. These substances cause direct structural changes in the valve, leading to stiffness and narrowing.
- Scarring from rheumatic fever. Although uncommon, rheumatic fever can cause direct damage to the pulmonary valve through inflammation and scarring. Rheumatic fever, caused by a streptococcal bacterial infection, can lead to long-term damage in heart valves, including thickening and stiffening of the pulmonary valve, restricting blood flow and resulting in stenosis.
Each of these direct causes leads to a narrowing or obstruction of the pulmonary valve, making it difficult for blood to flow efficiently from the heart to the lungs. The heart must then work harder to compensate for the restricted flow, which can result in symptoms like shortness of breath, chest pain, and fatigue.
Prevention of Pulmonary Stenosis
If a patient is born with a congenital defect affecting the pulmonary valve, pulmonary stenosis may be unavoidable. However, to prevent acquired pulmonary stenosis caused by complications from other conditions, the following practices can help keep the heart healthy:
- Eat foods rich in omega-3, phytonutrients, and fiber. These nutrients support heart health and reduce the risk of heart diseases. Omega-3 fatty acids, found in fish like salmon, tuna, sardines, and mackerel, help protect against inflammation. Phytonutrients and fiber, abundant in most fruits and vegetables, promote healthy cholesterol levels and blood vessel function.
- Avoid salty and fatty foods. Excess salt and fat can lead to high blood pressure, which forces the heart to work harder. Over time, this increased workload can damage heart structures, including the pulmonary valve. Reducing salt and saturated fat intake helps prevent hypertension and eases strain on the heart.
- Drink enough water daily. Staying hydrated helps flush excess sodium from the body. It is recommended to drink at least eight glasses of water per day to maintain proper fluid balance and support cardiovascular health.
- Exercise daily. Aim for at least 30 minutes of exercise each day. Regular physical activity helps maintain a healthy weight, prevents high blood pressure, and strengthens the heart. Exercise routines can include activities like brisk walking, cycling, or swimming.
- Avoid smoking and excessive alcohol consumption. Smoking and heavy drinking expose the heart to harmful toxins, raising blood pressure and increasing the risk of heart damage. Quitting smoking and moderating alcohol intake can significantly benefit heart health and lower the chances of developing heart-related complications.
- Prioritize rest and manage stress. Get adequate sleep every night to give the heart and body the rest they need. Chronic fatigue and stress can raise blood pressure and strain the heart. Good sleep hygiene and stress management can improve overall heart function.
Pulmonary stenosis, particularly if severe, can be life-threatening. Regular consultations with a healthcare provider can help monitor heart health and detect early signs of potential issues, ensuring prompt intervention when needed.
Risk Factors for Pulmonary Stenosis
Certain factors can increase the likelihood of developing pulmonary stenosis. Here are some of the primary risk factors:
- Family history of congenital heart defects. If there is a history of congenital heart defects in the family, especially in immediate relatives, a baby may be at higher risk of being born with pulmonary stenosis. This risk can be compounded if the mother has poor nutrition during the early stages of pregnancy, which can impact heart development.
- Carcinoid syndrome. Carcinoid syndrome is a condition where hormone-secreting tumors release substances into the bloodstream, affecting various organs, including the heart. Over time, these substances can cause thickening and stiffening of heart valves, potentially leading to complications like pulmonary stenosis.
- Rheumatic fever. Caused by a streptococcal bacterial infection, rheumatic fever primarily affects children and can lead to joint pain and high fever. If left untreated, the infection can spread to the heart, causing inflammation and rapid heartbeat, which can damage heart valves over time, including the pulmonary valve, and result in pulmonary stenosis.
- Noonan syndrome. Noonan syndrome is a genetic disorder that can affect physical appearance and heart function. Individuals with Noonan syndrome often have widely spaced eyes, low-set ears, a short neck, and a small jaw. They are also at higher risk of being born with pulmonary stenosis due to structural abnormalities in the heart associated with this condition.
- Previous heart surgery. Although heart surgeries aim to improve heart function, they can sometimes lead to scarring or complications in the heart tissue. If scar tissue develops around the pulmonary valve and is not well-managed, it can lead to structural changes that may result in pulmonary stenosis over time.
While these risk factors do not guarantee that a person will develop pulmonary stenosis, they indicate an elevated risk. Regular monitoring and early intervention, particularly for those with genetic predispositions or past heart surgeries, can help manage and mitigate potential complications related to pulmonary stenosis.
Pulmonary Stenosis FAQs
Pulmonary stenosis can be a complex condition to understand. Here are some frequently asked questions to help clarify the basics:
- What is pulmonary stenosis?
Pulmonary stenosis is a heart condition where the pulmonary valve, which allows blood flow from the right ventricle to the lungs, becomes thickened or narrowed. This narrowing restricts blood flow and causes the heart to work harder to pump blood through the valve. - Is pulmonary stenosis a congenital condition?
Most cases of pulmonary stenosis are congenital, meaning they are present from birth due to improper development of the pulmonary valve during fetal growth. However, in rare cases, it can also develop later in life due to other health conditions. - What are common symptoms of pulmonary stenosis?
Symptoms vary depending on the severity but may include shortness of breath, chest pain, fatigue, dizziness or fainting, and a “whooshing” sound (heart murmur) detectable by a healthcare provider. - How is pulmonary stenosis diagnosed?
Pulmonary stenosis is typically diagnosed through a combination of a physical exam, where a heart murmur may be detected, and imaging tests such as an echocardiogram, ECG, and sometimes cardiac catheterization to assess blood flow and valve function. - Can pulmonary stenosis be treated?
Yes, treatment depends on the severity of the stenosis. Mild cases may only need regular monitoring, while moderate to severe cases may require interventions such as balloon valvuloplasty (to widen the valve) or surgery to repair or replace the valve. - What is balloon valvuloplasty?
Balloon valvuloplasty is a minimally invasive procedure used to widen a narrowed pulmonary valve. During this procedure, a balloon-tipped catheter is inserted and inflated at the valve site to increase the valve opening, improving blood flow. - Can pulmonary stenosis lead to other complications?
Yes, if left untreated, pulmonary stenosis can lead to complications such as right ventricular hypertrophy (thickening of the heart muscle), heart failure, arrhythmias, and an increased risk of infective endocarditis. - Is pulmonary stenosis a life-threatening condition?
While mild cases may not impact life expectancy, severe pulmonary stenosis can be life-threatening if left untreated. Early diagnosis and treatment are essential for managing symptoms and preventing serious complications. - Can lifestyle changes help manage pulmonary stenosis?
While lifestyle changes alone won’t cure pulmonary stenosis, maintaining a heart-healthy diet, staying physically active (within doctor-recommended limits), and avoiding smoking or excessive alcohol can support overall heart health and complement medical treatment. - Will I need lifelong monitoring if I have pulmonary stenosis?
Yes, even after treatment, individuals with pulmonary stenosis typically require regular check-ups with a cardiologist. Lifelong monitoring helps ensure that any changes in heart function are detected early, and appropriate care is provided.