Summary
The heart is one of the most vital organs in the body. It serves as the center of the cardiovascular or circulatory system, responsible for pumping blood, oxygen, and nutrients throughout the body. Without the heart’s continuous function, vital organs like the brain, kidneys, liver, and lungs would lose their oxygen supply, gradually weaken, and eventually deteriorate.
The heart works tirelessly, beating non-stop, day and night. It is a strong muscle, divided into right and left sides. The right side consists of the right atrium and right ventricle, which are responsible for pumping blood to the lungs. The left side, which includes the left atrium and left ventricle, pumps oxygen-rich blood to the rest of the body.
While the heart is a robust organ, it is not immune to diseases. Damage or issues in any part of the heart can lead to heart disease. Additionally, other parts of the cardiovascular system, such as blood vessels, can also develop problems. In the Philippines, heart disease is one of the leading causes of mortality.
Individuals with heart disease may experience symptoms like chest pain, shortness of breath, irregular heartbeats, dizziness, headaches, paleness, bluish skin, swelling in the abdomen, legs, and feet, and persistent fatigue, among others. The presentation of symptoms can vary depending on the type of heart disease, and some symptoms, such as bluish skin or swelling, may not be present in every case.
Anyone can develop heart disease, regardless of gender or age. Even infants can be affected if they are born with congenital heart defects. Heart disease can also result from an unhealthy lifestyle, including habits like consuming high-salt and high-fat foods, lack of exercise, obesity, smoking, excessive alcohol consumption, and more. In some cases, heart disease develops as a complication of other medical conditions.
Heart disease can pose significant risks, especially if left untreated. However, with timely intervention, its symptoms can be managed or alleviated, improving a patient’s quality of life. Some heart conditions can be treated with medication, while others may require surgical intervention to address underlying problems.
How Does the Heart Work?
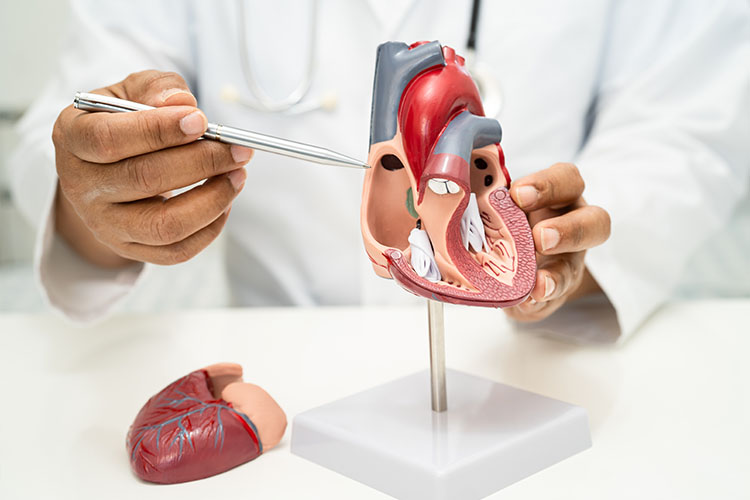
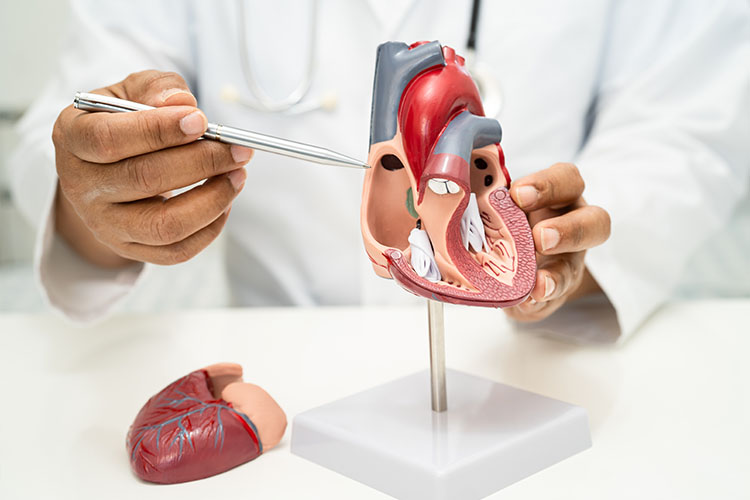
The heart is a vital organ that functions as the body’s central pump, ensuring that blood, oxygen, and essential nutrients circulate throughout the body. It is located slightly to the left of the chest, nestled between the lungs, and is protected by the ribcage. Structurally, the heart is divided into four chambers: two upper chambers called the atria (left and right atrium) and two lower chambers called the ventricles (left and right ventricle). These chambers work in a coordinated manner to pump blood efficiently throughout the body.
The process begins when oxygen-depleted blood returns from the body to the right atrium. From there, it flows into the right ventricle, which then pumps the blood into the lungs through the pulmonary arteries. In the lungs, the blood picks up oxygen and releases carbon dioxide—a process known as gas exchange. This freshly oxygenated blood then travels back to the heart, entering the left atrium. The left atrium pushes the blood into the left ventricle, which is the most muscular chamber of the heart, responsible for pumping oxygen-rich blood through the aorta and into the body’s systemic circulation.
The heart operates continuously, maintaining a steady rhythm through electrical impulses that originate from a specialized group of cells known as the sinoatrial (SA) node, often referred to as the heart’s natural pacemaker. These electrical impulses cause the heart’s chambers to contract and relax in a synchronized way, creating a heartbeat. The SA node initiates the signal, causing the atria to contract and push blood into the ventricles. Next, the signal moves to the atrioventricular (AV) node and then to the bundle of His and Purkinje fibers, prompting the ventricles to contract and pump blood to the lungs and the rest of the body.
The heart’s ability to adjust its rate and strength is influenced by several factors, such as physical activity, emotional stress, and overall health. For instance, during exercise, the heart beats faster to deliver more oxygen-rich blood to the muscles. At rest, the heart rate slows down to maintain a steady supply of blood to vital organs. Additionally, hormones like adrenaline can temporarily increase heart rate in response to stress or danger.
Valves within the heart ensure that blood flows in the correct direction. The tricuspid valve separates the right atrium and right ventricle, while the mitral valve separates the left atrium and left ventricle. On the other hand, the pulmonary valve regulates blood flow from the right ventricle to the lungs, and the aortic valve controls blood flow from the left ventricle to the aorta. These valves open and close with each heartbeat, preventing backflow and ensuring efficient circulation.
In summary, the heart functions as a powerful and efficient pump, driven by electrical signals and controlled by valves that ensure proper blood flow. It supplies oxygenated blood to the entire body while removing waste products like carbon dioxide. This continuous process is crucial for sustaining life, as it keeps tissues and organs nourished, enabling them to perform their functions.
Symptoms of Heart Disease
Different types of heart disease often present with similar symptoms, as they all affect the cardiovascular or circulatory system. However, heart disease can also impact other parts of the body due to the interconnected nature of the circulatory system. Each organ receives its blood supply through a network of vessels, making the entire body susceptible to changes when the heart is not functioning properly.
Here are some common symptoms associated with heart disease:

- Chest pain. This pain can feel like a sharp stabbing sensation, a crushing pressure, heaviness, or tightness in the chest. It often signals an underlying issue with the heart’s blood flow.
- Shortness of breath. Difficulty breathing may occur, especially during physical activity or even at rest, indicating the heart’s inability to pump blood efficiently.
- Irregular heartbeats. Patients may experience a rapid heartbeat, a slowed heart rate, or even abnormal sounds (murmurs) when listened to with a stethoscope.
- Dizziness. Feeling lightheaded or faint can occur due to insufficient blood flow to the brain.
- Headaches. Some heart conditions, especially those affecting blood pressure, can cause frequent headaches.
- Paleness. A lack of adequate blood flow may cause a pale or ashen complexion.
- Bluish or darkened skin. Known as cyanosis, this symptom can occur when there is a significant drop in oxygen levels in the blood. It is often seen in patients with congenital heart defects, such as a hole in the heart.
- Swelling in the abdomen, legs, and feet. Fluid retention due to poor circulation or weakened heart function can cause swelling in these areas.
- Easily fatigued. Even simple activities may leave a person feeling extremely tired, as the heart struggles to supply the muscles and tissues with enough oxygen-rich blood.
Some of these symptoms may not manifest in every individual. For example, cyanosis, or the bluish tint to the skin, is more common in those with congenital heart defects. Swelling, on the other hand, might be absent if the kidneys are functioning properly, as they help regulate fluid levels in the body.
The type and severity of chest pain can also vary. Patients may describe it as a sharp, stabbing pain, a heavy weight on their chest, or a squeezing sensation. Irregular heartbeats may cause a patient to feel palpitations, such as a rapid or slow heartbeat, or abnormal sounds heard through a stethoscope. Recognizing these symptoms early can be crucial in diagnosing and managing heart disease effectively.
Types of Heart Diseases
Heart disease can come in many forms, each affecting different parts of the heart, its muscles, blood vessels, or the overall cardiovascular system. Understanding the various types of heart disease can help in better identifying the symptoms and finding appropriate treatments. Here is a breakdown of the main categories of heart disease:
-
Cardiovascular Diseases (CVD)
These diseases affect the cardiovascular system, including the heart itself, coronary arteries, and other blood vessels. This category is broad and includes conditions that impair blood flow, heart function, and structural integrity:
- Angina
- Acute coronary syndrome
- Aortic aneurysm
- Aortic dissection
- Aortic regurgitation
- Aortic stenosis
- Arrhythmia (irregular heartbeat)
- Atherosclerosis (narrowing of arteries due to plaque build-up)
- Heart failure (inability of the heart to pump blood effectively)
- Hypertrophic cardiomyopathy (thickening of the heart muscle)
- Dilated cardiomyopathy (enlargement and weakening of the heart)
-
Cardiac Electrophysiology Disorders
This category includes conditions that affect the heart’s electrical system, leading to issues with how the heart beats or conducts signals:
- Atrioventricular block (AV Block)
- Atrial fibrillation (AFib)
- Brugada syndrome
- Long QT syndrome
- Wolff-Parkinson-White syndrome
- Bundle branch block
- Ventricular tachycardia (rapid heartbeats originating in the lower heart chambers)
- Heart block (disrupted electrical signals in the heart)
-
Congenital heart disease refers to heart conditions that are present from birth. These defects may affect the heart’s structure, function, or rhythm:
- Aortic coarctation (narrowing of the aorta)
- Atrial septal defect (hole in the wall between the heart’s upper chambers)
- Tetralogy of Fallot (combination of four heart defects)
- Ventricular septal defect (hole in the heart’s lower chambers)
- Hypoplastic left heart syndrome (underdeveloped left side of the heart)
- Transposition of the great arteries (incorrectly connected arteries)
- Patent ductus arteriosus (persistent opening between the aorta and pulmonary artery)
-
Ischemic Heart Disease
In ischemic heart disease, the heart receives insufficient oxygen due to reduced blood flow, often caused by narrowed or blocked arteries:
- Angina pectoris (chest pain due to reduced blood flow)
- Heart attack (acute myocardial infarction)
- Chronic ischemic heart disease (long-term reduced blood flow to the heart)
-
Valvular Heart Disease
This category encompasses conditions that affect the heart’s valves, which regulate blood flow within the heart chambers:
- Aortic insufficiency (aortic valve fails to close properly)
- Mitral valve prolapse (valve bulges into the left atrium)
- Mitral stenosis (narrowing of the mitral valve)
- Tricuspid valve stenosis (narrowing of the tricuspid valve)
- Pulmonary valve stenosis (narrowing of the pulmonary valve)
- Regurgitation of the mitral, tricuspid, or pulmonary valves (valves fail to close properly, leading to backflow of blood)
While heart disease remains a leading cause of death worldwide, many of these conditions can be managed or treated with early intervention. Close communication with healthcare providers and adherence to treatment plans are crucial for managing symptoms and improving the quality of life for those living with heart disease.
Diagnostic Procedures for Heart Disease
Accurate diagnosis is crucial for managing heart disease, and doctors use a variety of tests to evaluate heart function, identify abnormalities, and determine the severity of conditions. Here are some of the most common diagnostic procedures for heart disease:
-
Electrocardiogram (ECG or EKG)
An electrocardiogram records the heart’s electrical activity through electrodes placed on the chest and limbs, producing a graph of the heart’s rhythm and electrical impulses. This test helps detect abnormal heart rhythms (arrhythmias), signs of a heart attack, or other heart conditions by revealing irregularities in the heart’s electrical signals.
-
Echocardiogram
This test uses ultrasound waves to create real-time images of the heart, showing its chambers, valves, and blood flow. A handheld device called a transducer is placed on the chest, producing sound waves that bounce back to form a moving picture of the heart. It is commonly used to assess heart valve function, detect heart defects, and evaluate conditions like cardiomyopathy.
-
Stress Test
A stress test evaluates how the heart performs under physical exertion, usually involving exercise on a treadmill or stationary bike while heart activity is monitored. For those unable to exercise, medication may be used to mimic the effects of exercise. It is especially useful for detecting coronary artery disease, arrhythmias, and determining the heart’s ability to supply oxygen during increased activity levels.
-
Holter Monitor
A Holter monitor is a portable device worn for 24 to 48 hours that continuously records the heart’s electrical activity as the patient goes about their daily activities. It helps detect intermittent irregular heart rhythms that may not show up during a standard ECG, providing a broader picture of heart health over a longer period.
-
Cardiac Catheterization
This invasive procedure involves threading a thin tube (catheter) through a blood vessel to the heart, allowing doctors to inject a special dye visible on X-rays. This process provides detailed images of the coronary arteries and heart chambers, helping to identify blockages, measure pressures, and assess heart function. It is often used when planning treatments like angioplasty or stenting.
-
Coronary Angiography
Typically done as part of cardiac catheterization, coronary angiography uses X-ray imaging to examine the heart’s blood vessels. A dye is injected into the coronary arteries, highlighting any narrowing or blockages. This procedure is vital for assessing the severity of coronary artery disease and deciding on interventions like stenting or bypass surgery.
-
Magnetic Resonance Imaging (MRI)
A cardiac MRI uses magnetic fields and radio waves to produce detailed images of the heart and its structures. Patients lie in a scanner while images are taken to visualize the heart’s anatomy and assess conditions like heart muscle diseases, congenital heart defects, or tissue damage after a heart attack. It provides high-resolution images that are valuable for complex cases.
-
Computed Tomography (CT) Scan
A cardiac CT scan takes cross-sectional images of the heart and blood vessels, often using contrast dye for enhanced visibility. It is particularly effective for detecting blockages in the coronary arteries, evaluating the heart’s structure, and diagnosing conditions like aortic aneurysms. This non-invasive test provides detailed 3D images that aid in diagnosis.
-
Blood Tests
Blood tests measure levels of enzymes and proteins released into the bloodstream when the heart is damaged, such as troponin, which is often elevated during a heart attack. Other tests include measuring cholesterol, blood sugar, and BNP (B-type natriuretic peptide) levels, which help assess heart failure and overall cardiovascular health.
-
Chest X-ray
A chest X-ray provides images of the heart, lungs, and surrounding areas, helping doctors identify abnormalities like an enlarged heart, fluid accumulation around the heart (pericardial effusion), or lung conditions that can affect the heart. It is often used as a preliminary tool in diagnosing heart and lung issues.
-
Nuclear Cardiology (e.g., PET Scan, MUGA Scan)
Nuclear cardiology involves injecting a small amount of radioactive tracer into the bloodstream, which is then detected using a special camera to produce images of the heart. This helps identify areas of poor blood flow, assess heart function after a heart attack, and monitor heart failure. It provides valuable information about the heart’s efficiency in pumping blood.
These diagnostic procedures offer a comprehensive view of heart health, allowing doctors to pinpoint specific issues and develop a tailored treatment plan. Early detection through these tests can significantly improve outcomes, ensuring that appropriate interventions are applied to manage or even treat heart conditions effectively.
Complications of Untreated Heart Disease
Heart disease, when left untreated, can lead to a range of serious complications that affect not only the heart but other vital organs as well. These complications can significantly diminish a person’s quality of life and, in severe cases, become life-threatening. Understanding these risks emphasizes the importance of early diagnosis, ongoing treatment, and lifestyle changes.
- Heart Failure. This is one of the most common complications of untreated heart disease. It occurs when the heart becomes too weak or stiff to pump blood effectively, leading to the accumulation of fluid in the lungs and other parts of the body. Symptoms include severe shortness of breath, persistent fatigue, swelling in the legs and abdomen, and difficulty performing daily activities.
- Heart Attack (Myocardial Infarction). Untreated conditions like coronary artery disease (CAD) can lead to a heart attack, where blood flow to a part of the heart is blocked, often by a blood clot. This blockage causes damage to the heart muscle, which can be irreversible if not treated promptly. A heart attack can lead to complications like arrhythmias, heart failure, and even sudden death.
- Stroke. Heart disease significantly increases the risk of stroke, particularly in those with conditions like atrial fibrillation (irregular heartbeat). When the heart does not pump blood efficiently, clots can form and travel to the brain, causing a blockage and leading to a stroke. Strokes can cause long-term disability, affecting speech, movement, and cognitive abilities.
- Arrhythmias. Conditions such as atrial fibrillation, if left unmanaged, can cause the heart to beat irregularly, which increases the risk of blood clots and stroke. Severe arrhythmias can lead to cardiac arrest, a condition where the heart suddenly stops beating, requiring immediate medical intervention to prevent death.
- Peripheral Artery Disease (PAD). PAD occurs when plaque builds up in the arteries that supply blood to the limbs, usually the legs. It often develops alongside coronary artery disease and can cause pain, numbness, and in severe cases, tissue death due to lack of blood flow. If untreated, PAD can lead to gangrene and may require limb amputation.
- Kidney Damage or Failure. The heart and kidneys are closely connected through the circulatory system. Untreated heart disease can impair blood flow to the kidneys, leading to chronic kidney disease (CKD) or kidney failure. This condition reduces the kidneys’ ability to filter waste from the blood, leading to a buildup of toxins and the need for dialysis.
- Liver Congestion. Heart failure can cause blood to back up into the liver, leading to a condition known as congestive hepatopathy. Over time, this can cause liver damage, scarring, and impaired liver function, contributing to further complications and making heart disease management even more challenging.
- Pulmonary Hypertension. This condition occurs when high blood pressure affects the arteries in the lungs and the right side of the heart. Untreated heart conditions, especially those involving the heart’s valves or left-sided heart failure, can cause increased pressure in the pulmonary arteries, leading to shortness of breath, dizziness, and in severe cases, heart failure.
- Sudden Cardiac Arrest. One of the most severe complications of untreated heart disease is sudden cardiac arrest, where the heart’s electrical system malfunctions, causing it to stop beating altogether. This condition requires immediate medical attention and can be fatal if not treated within minutes using defibrillation and cardiopulmonary resuscitation (CPR).
- Aneurysms. Heart disease can weaken the walls of arteries, leading to the formation of aneurysms, which are abnormal bulges or ballooning in the walls of blood vessels. An aneurysm can occur in any artery but is most dangerous in major arteries like the aorta. If an aneurysm ruptures, it can cause life-threatening internal bleeding.
- Complications During Pregnancy. Women with untreated heart disease may experience complications during pregnancy, such as preeclampsia (high blood pressure), arrhythmias, or even heart failure. These conditions pose serious risks to both the mother and the unborn child, making careful monitoring and management essential.
- Depression and Anxiety. Living with untreated heart disease can have a significant impact on mental health, leading to feelings of hopelessness, depression, and anxiety. These emotional challenges can further complicate physical symptoms, creating a cycle that makes managing heart health even more difficult.
Heart disease is a progressive condition, and without timely treatment, the risk of these complications increases substantially. Recognizing symptoms early, maintaining regular check-ups, and adhering to prescribed treatments can make a significant difference in managing the condition and improving long-term outcomes.
Causes of Heart Disease
Heart disease can develop due to several underlying conditions or defects that directly impair heart function. Here are some key causes:
- High Blood Pressure (Hypertension). Persistent high blood pressure forces the heart to pump blood with more effort than usual. Over time, this extra strain can cause the heart muscle to thicken, become less efficient, or weaken, leading to conditions like heart failure and increased risk of heart attack.
- Atherosclerosis (Plaque Buildup in Arteries). Atherosclerosis occurs when cholesterol, fat, and other substances build up in the walls of the arteries, forming plaques. These plaques can narrow the arteries and restrict blood flow to the heart muscle, which may result in chest pain (angina) or a heart attack if a plaque ruptures and forms a blood clot.
- Diabetes-Related Vascular Damage. High blood sugar levels can damage the walls of blood vessels over time, making them more prone to plaque buildup. Additionally, diabetes can affect how the heart functions, making it a significant cause of heart disease, especially when poorly managed.
- Heart Valve Disorders. Conditions that affect the heart valves, such as valve stenosis or valve regurgitation, can disrupt normal blood flow through the heart. This forces the heart to work harder, which can eventually lead to heart enlargement, weakening, and heart failure.
- Congenital Heart Defects. Some people are born with structural heart problems that result from abnormal heart development in the womb. These defects might involve incomplete formation of heart chambers, faulty valves, or holes in the heart walls, leading to abnormal circulation and heart function.
- Myocardial Infarction (Heart Attack). A heart attack occurs when a part of the heart muscle doesn’t receive enough oxygen-rich blood due to a blocked coronary artery. This damage to the heart muscle can impair the heart’s ability to pump effectively and may lead to chronic heart conditions.
- Infections Affecting the Heart (e.g., Endocarditis). Infections such as endocarditis, which is an inflammation of the heart’s inner lining, can damage the heart valves and heart muscle. This condition is often caused by bacteria that enter the bloodstream and reach the heart.
These causes directly affect the heart’s structure or its ability to function properly, leading to the development of various heart conditions. Identifying these underlying causes early can help in managing the disease and preventing complications.
Treatment for Heart Disease
Treating heart disease requires a combination of medications and medical procedures, depending on the type and severity of the condition. Below are some common treatments and procedures for patients with heart disease:
Medications for Heart Disease
Medications are often the first line of defense in managing heart disease. They aim to control symptoms, prevent blood clots, manage cholesterol levels, and improve overall heart function. Here are some of the most commonly prescribed medications:
- Blood Thinners. These medications, like aspirin, help prevent blood clots from forming, reducing the risk of blockages in the arteries. This helps keep blood flowing smoothly through the heart and reduces the risk of heart attacks and strokes.
- Anti-Platelet Drugs. For patients who cannot take aspirin, doctors may prescribe anti-platelet medications such as clopidogrel, prasugrel, or ticagrelor. These drugs prevent platelets from sticking together, which helps reduce the risk of clot formation.
- Anti-Coagulants. These medications, including warfarin and newer oral anticoagulants (NOACs), work similarly to blood thinners but are often stronger. They can help dissolve existing clots, making them beneficial for patients at risk of deep vein thrombosis or pulmonary embolism.
- Blood Pressure Medications. High blood pressure is a significant contributor to heart disease, so controlling it is crucial. Medications like ACE inhibitors, angiotensin II receptor blockers (ARBs), and beta-blockers are commonly used to lower blood pressure, reducing strain on the heart and blood vessels.
- Cholesterol-Lowering Drugs. Statins are a standard choice for reducing LDL cholesterol levels, which can help prevent the buildup of plaque in the arteries. Keeping cholesterol in check is key to preventing further heart complications.
- Anti-Anginal Medications. These drugs, like nitrates, help alleviate chest pain or tightness (angina) by relaxing the blood vessels and improving blood flow to the heart. They provide relief for patients experiencing frequent chest discomfort.
Procedures and Surgeries for Heart Disease
When medications alone are not sufficient, certain medical procedures and surgeries may be necessary to restore normal heart function or address blockages and defects. These include:
- Open-Heart Surgery. This involves opening the chest to directly access the heart for repairs. It is typically reserved for severe cases or when other, less invasive methods are not viable. It can address a range of conditions, from repairing damaged heart valves to correcting structural defects.
- Angioplasty. A less invasive procedure, angioplasty involves inserting a balloon catheter through an artery (usually from the groin) to reach the blocked coronary arteries. Once in place, the balloon is inflated to press the blockage against the artery walls, improving blood flow. In some cases, a stent (a small metal mesh) is placed to keep the artery open.
- Coronary Artery Bypass Grafting (CABG). This surgery creates a new pathway for blood to flow around a blocked or narrowed coronary artery. Surgeons use a healthy blood vessel from another part of the body to redirect blood flow, helping to restore proper circulation.
- Valve Repair or Replacement Surgery. For issues with heart valves, doctors may perform a valve repair surgery to fix the existing valve. If the damage is too severe, valve replacement surgery is needed, using either a mechanical valve or one made from animal tissue (such as from pigs or cows).
- Pacemaker. A pacemaker is a small device implanted near the heart or in the abdomen. It helps regulate the heartbeat by sending electrical signals when the heart’s natural rhythm is too slow or irregular. It is especially beneficial for patients with arrhythmias, helping maintain a steady heart rate.
These treatments, whether through medications or surgical interventions, aim to manage symptoms, improve the quality of life, and prevent the progression of heart disease. Close coordination with healthcare providers and adherence to prescribed therapies are essential for achieving the best outcomes in managing heart conditions.
Prevention of Heart Disease
Maintaining a healthy heart involves adopting a lifestyle that supports cardiovascular health. To reduce the risk of developing heart disease, consider following these key practices:
- Eat a Balanced and Nutritious Diet. Focus on consuming fruits, vegetables, whole grains, lean proteins, and healthy fats. Avoid foods high in salt, saturated fats, and trans fats, as these can contribute to high blood pressure and elevated cholesterol levels, both of which increase the risk of heart disease.
- Exercise Regularly. Aim for at least 30 minutes of moderate exercise daily, such as walking, jogging, or swimming. Regular physical activity helps strengthen the heart, improve circulation, and maintain a healthy weight. It also helps manage stress, which can contribute to heart issues.
- Maintain a Healthy Weight. Keeping a weight within the recommended range for your height and age reduces the strain on your heart and lowers the risk of conditions like hypertension and high cholesterol. This can be achieved through a combination of a healthy diet and regular exercise.
- Quit Smoking. Smoking introduces harmful chemicals into the body that damage blood vessels and raise blood pressure. Quitting smoking not only improves lung health but also significantly reduces the risk of heart disease, heart attacks, and strokes.
- Limit Alcohol Intake. Drinking alcohol in excess can lead to high blood pressure and other heart-related issues. It’s best to consume alcohol in moderation—no more than one drink per day for women and two drinks per day for men.
- Get Regular Health Check-Ups. Regular visits to the doctor allow for early detection of risk factors such as high blood pressure, high cholesterol, or diabetes. Early intervention can help prevent the onset or progression of heart disease.
- Seek Medical Advice for Any Symptoms. If you experience symptoms like chest pain, shortness of breath, or irregular heartbeats, consult a doctor immediately. Start with a general practitioner or an internist for initial evaluations. If heart disease is suspected, they may refer you to a cardiologist for specialized care.
By making these lifestyle adjustments and prioritizing regular health monitoring, you can significantly lower the risk of heart disease and promote a healthier, more resilient heart. Prevention is key, and early lifestyle changes can have a lasting impact on overall cardiovascular health.
Risk Factors for Heart Disease
Heart disease can affect anyone, but certain factors can increase the risk of developing it. Understanding these risk factors is essential for prevention and early intervention. Here are some of the most common factors that can elevate the likelihood of heart disease:
- Age. As people get older, their heart and blood vessels become less flexible and more prone to damage. This makes older adults more susceptible to heart disease compared to younger individuals.
- Gender. While heart disease is common in both men and women, men are generally at a higher risk earlier in life. Women’s risk increases after menopause due to changes in hormonal levels.
- Family History. Genetics play a role in heart health. If close family members, such as parents or siblings, have a history of heart disease, the likelihood of developing similar conditions increases.
- High Blood Pressure (Hypertension). Chronic high blood pressure can cause arteries to become stiff and narrow, forcing the heart to work harder to pump blood. This added strain can contribute to various heart conditions over time.
- Unhealthy Lifestyle Choices. Lifestyle habits greatly impact heart health. Risk is higher among individuals who:
- Consume a diet high in salt and unhealthy fats. Regular consumption of salty and fatty foods can contribute to hypertension and blockages in blood vessels.
- Do not engage in regular physical activity. Lack of exercise can lead to weight gain and the buildup of fat in blood vessels, which can hinder blood flow and strain the heart.
- Smoke cigarettes. The chemicals in cigarettes, such as nicotine and carbon monoxide, can thicken the blood, making clots more likely and increasing the risk of blocked arteries.
- Consume excessive alcohol. Heavy drinking can raise blood pressure levels, which over time can contribute to the weakening of the heart and blood vessels.
- Being Overweight or Obese. Carrying extra weight forces the heart to work harder to supply blood throughout the body, increasing the risk of hypertension and heart strain.
- Underlying Health Conditions. Conditions like diabetes can increase the risk of heart disease, as high blood sugar levels over time can damage blood vessels and the nerves that control the heart.
- Congenital Heart Defects. Some individuals are born with structural heart issues, known as congenital heart defects, which can affect heart function from an early age and require lifelong management.
By understanding these risk factors, individuals can make more informed choices about their health and work with healthcare providers to reduce their risk of heart disease. Regular check-ups, a balanced diet, exercise, and avoiding harmful habits like smoking and excessive alcohol consumption are crucial steps in maintaining heart health.
Heart Disease FAQs
- What is heart disease?
Heart disease refers to a broad range of conditions that affect the heart’s ability to function properly. It includes issues with the heart’s blood vessels (cardiovascular disease), rhythm problems (arrhythmias), congenital defects (those present at birth), and conditions that involve the heart muscle or its valves.
- What are the main symptoms of heart disease?
Common symptoms include chest pain or discomfort, shortness of breath, irregular heartbeats, fatigue, swelling in the legs or abdomen, and sometimes dizziness or fainting. Depending on the type of heart disease, symptoms may vary or be more severe.
- What causes heart disease?
Heart disease can result from various factors, including unhealthy diet, lack of exercise, smoking, excessive alcohol consumption, and genetic predisposition. Conditions like high blood pressure, high cholesterol, and diabetes also increase the risk of developing heart disease.
- Can heart disease be prevented?
Yes, many types of heart disease can be prevented through lifestyle changes. Eating a balanced diet, exercising regularly, maintaining a healthy weight, quitting smoking, and limiting alcohol intake can reduce the risk. Regular medical check-ups are also important for early detection of risk factors.
- Who is at risk for heart disease?
Anyone can develop heart disease, but certain groups are more at risk, such as older adults, those with a family history of heart disease, individuals with high blood pressure, high cholesterol, or diabetes, and those with unhealthy lifestyle habits like smoking and physical inactivity.
- How is heart disease diagnosed?
Doctors may use a variety of diagnostic tests, including electrocardiograms (ECG), echocardiograms, stress tests, blood tests, and imaging tests like CT or MRI scans. In some cases, cardiac catheterization or angiography may be needed to get a closer look at the heart’s structure and blood flow.
- What are the common treatments for heart disease?
Treatment varies depending on the type and severity of the heart condition. It may include lifestyle changes, medications like blood thinners or cholesterol-lowering drugs, and medical procedures such as angioplasty, stenting, or even heart surgery like a bypass. Some patients may also require implanted devices like pacemakers.
- Is heart disease the same as a heart attack?
No, heart disease is a broad term that includes a variety of heart conditions, while a heart attack (myocardial infarction) specifically refers to a blockage in the blood supply to part of the heart muscle, causing tissue damage. A heart attack is often a result of coronary artery disease, one of the many types of heart disease.
- Can stress cause heart disease?
Chronic stress can contribute to heart disease. It may lead to high blood pressure, which strains the heart over time. Stress can also encourage unhealthy habits like overeating, smoking, or drinking alcohol, which further increase the risk of heart disease.
- Can young people get heart disease?
Yes, although heart disease is more common in older adults, young people can develop it too, especially if they have congenital heart defects, genetic predispositions, or unhealthy lifestyle habits like poor diet and lack of physical activity. Early prevention is important, regardless of age.
- What is the role of diet in heart health?
Diet plays a crucial role in maintaining heart health. Eating foods low in saturated fats, trans fats, and cholesterol while increasing fiber intake helps keep cholesterol levels in check. A diet rich in fruits, vegetables, whole grains, and lean protein supports overall heart function and reduces the risk of developing heart disease.
- How does exercise benefit the heart?
Regular physical activity strengthens the heart muscle, improves blood flow, helps maintain a healthy weight, and lowers blood pressure. It also boosts good cholesterol (HDL) and reduces bad cholesterol (LDL), which helps prevent the buildup of plaque in the arteries.
- Can heart disease be cured?
While some heart conditions can be managed or treated effectively, many types of heart disease, especially those related to structural changes or genetic issues, cannot be fully cured. However, with proper treatment and lifestyle modifications, symptoms can be managed, and the risk of complications can be reduced.
- When should I see a doctor about heart disease?
If you experience symptoms like persistent chest pain, shortness of breath, irregular heartbeats, or sudden dizziness, it’s important to consult a doctor. Early diagnosis and treatment can significantly improve the outlook for many heart conditions.