Summary
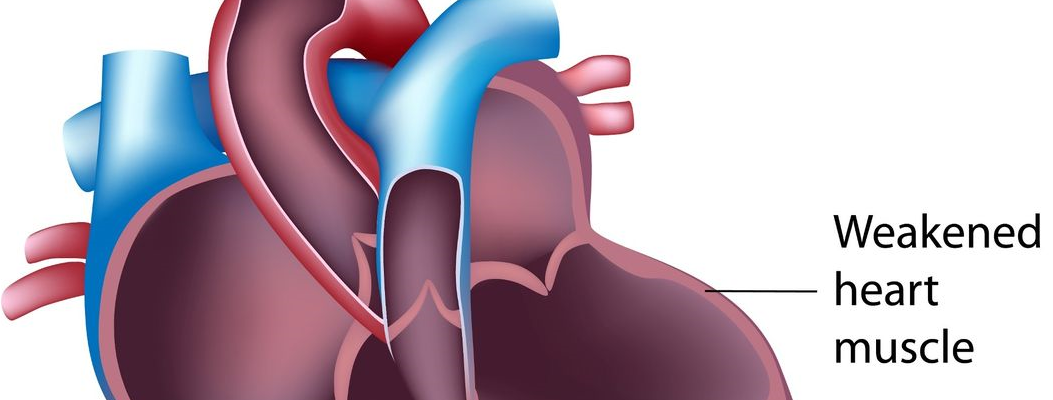
Dilated cardiomyopathy (DCM) is a heart condition where the left ventricle, the heart’s primary pumping chamber, becomes enlarged and weakened, losing its ability to pump blood effectively. This reduced function leads to decreased blood supply to the body, causing symptoms like shortness of breath, fatigue, and swelling, especially in the legs and feet.
DCM can be hereditary, but it also has other potential causes, including excessive alcohol use, high blood pressure, certain medications, and health conditions like coronary artery disease, viral infections, thyroid issues, and diabetes. These factors can damage the heart muscle over time, leading to enlargement and reduced heart function.
Treatment for DCM often involves medications to improve heart performance and, in some cases, surgical options like heart-assisted devices to regulate heart rhythm. In severe cases, a heart transplant may be considered if other treatments are not effective. Early diagnosis and treatment are crucial to help manage symptoms, slow disease progression, and improve quality of life.
Table of Contents
- Symptoms of Dilated Cardiomyopathy
- Types of Dilated Cardiomyopathy
- Diagnostic Procedures for Dilated Cardiomyopathy
- Complications of Untreated Dilated Cardiomyopathy
- Causes of Dilated Cardiomyopathy
- Prevention of Dilated Cardiomyopathy
- Risk Factors for Dilated Cardiomyopathy
- Dilated Cardiomyopathy FAQs
Symptoms of Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) commonly affects people between the ages of 20 and 60. This condition weakens the heart’s ability to pump blood effectively, causing a range of symptoms that impact the body’s blood and oxygen supply.
- Shortness of breath. Individuals with DCM often experience difficulty breathing because the weakened heart cannot supply sufficient blood to the body, which also reduces oxygen levels delivered to tissues and organs.
- Chest tightness. The enlargement of the left ventricle may cause sensations of chest tightness, as the expanded heart begins to press against nearby organs and bones, leading to discomfort.
- Fatigue. Due to the impaired blood flow, the body receives less oxygen and nutrients, leading to persistent fatigue even with minimal exertion.
- Dizziness. Insufficient blood and oxygen flow to the brain can cause dizziness or even fainting spells, especially when standing or moving suddenly.
- Heart palpitations. Irregular or rapid heartbeats are common, as the enlarged heart muscle strains to maintain blood flow, leading to a sensation of a racing or pounding heartbeat.
- Edema or swelling. Swelling, particularly in the abdomen, legs, and feet, occurs because reduced blood flow affects the kidneys’ ability to remove excess fluid. This buildup leads to fluid retention, causing visible swelling in certain areas.
If left unmanaged, these symptoms can worsen, significantly impacting a person’s quality of life. Timely diagnosis and intervention are key in managing DCM and improving overall heart health.
Types of Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) is classified based on the primary causes or factors contributing to the condition. These classifications help in understanding how the disease develops and in determining effective treatment approaches.
- Genetic or familial dilated cardiomyopathy. This type is inherited, with mutations in specific genes that are passed down within families. Individuals with a family history of DCM are at higher risk, and genetic testing or regular cardiac screenings are recommended for early detection and management.
- Ischemic dilated cardiomyopathy. This form is caused by reduced blood flow to the heart muscle, typically due to coronary artery disease or previous heart attacks. The lack of oxygenated blood weakens the heart muscle, causing it to enlarge and struggle to pump effectively.
- Alcoholic or toxin-induced dilated cardiomyopathy. Long-term exposure to certain toxins, such as excessive alcohol, specific chemotherapy drugs, or illicit drugs, can damage the heart muscle, leading to DCM. These substances can directly weaken the heart’s structure, causing it to dilate over time.
- Idiopathic dilated cardiomyopathy. In many cases, the exact cause of DCM remains unknown, even after thorough testing. This is classified as idiopathic DCM, meaning the disease arises without a clear underlying cause.
These main classifications of DCM help guide diagnosis, treatment, and prevention strategies tailored to the underlying factors. Early identification of the type of DCM can significantly impact the management and prognosis of the condition.
Diagnostic Procedures for Dilated Cardiomyopathy
Diagnosing dilated cardiomyopathy (DCM) involves a series of tests to evaluate heart function, measure blood flow, and determine the extent of heart muscle enlargement. Here are the primary diagnostic procedures used to identify and assess DCM:
- Physical examination and medical history. The doctor will conduct a physical exam to check for symptoms such as irregular heartbeats, swelling, or abnormal heart sounds. Gathering a thorough medical history, including any family history of heart disease, helps assess risk factors and potential causes.
- Electrocardiogram (ECG). An ECG records the electrical activity of the heart, which helps detect irregular heart rhythms, abnormal heart size, and signs of a weakened heart muscle. This test is often used as a first step in diagnosing DCM.
- Echocardiogram. This ultrasound test provides real-time images of the heart, allowing doctors to see if the heart chambers are enlarged and assess the heart’s pumping efficiency. An echocardiogram is a key diagnostic tool for detecting DCM and determining its severity.
- Chest X-ray. A chest X-ray can show an enlarged heart and detect any fluid buildup in the lungs, which may indicate heart failure—a common complication of DCM. This imaging test helps visualize the overall size and shape of the heart.
- Cardiac MRI. Magnetic resonance imaging (MRI) offers detailed images of the heart muscle, allowing doctors to assess its structure and function. A cardiac MRI can reveal specific areas of damage and measure the heart’s ability to pump blood effectively.
- Stress test. In a stress test, the heart’s response to exercise or medication is monitored to assess how well it functions under strain. This test helps determine the severity of DCM and evaluate blood flow and oxygen supply to the heart muscle.
- Blood tests. Blood tests can check for markers of heart failure, such as B-type natriuretic peptide (BNP), and measure levels of electrolytes, thyroid hormones, and other substances that may indicate underlying causes or complications.
- Coronary angiography. In this procedure, a special dye is injected into the coronary arteries, and X-ray images are taken to check for blockages. This test helps rule out coronary artery disease as a cause of DCM and assesses blood flow in the heart.
Each of these diagnostic procedures plays a critical role in diagnosing DCM and developing an appropriate treatment plan. Early detection through these tests can help manage symptoms and prevent further progression of the disease, improving the patient’s quality of life.
Complications of Untreated Dilated Cardiomyopathy
If left untreated, dilated cardiomyopathy (DCM) can lead to a range of serious health complications. As the heart’s ability to pump blood weakens, multiple organs and body systems can be affected, and life-threatening conditions may develop.
- Heart failure. The most common complication of untreated DCM is heart failure, where the heart becomes too weak to effectively pump blood throughout the body. This can lead to symptoms such as severe fatigue, shortness of breath, and fluid buildup in the lungs, legs, and abdomen.
- Arrhythmias. Untreated DCM can cause irregular heart rhythms, or arrhythmias, which can be mild or severe. Dangerous arrhythmias, such as ventricular tachycardia or fibrillation, can increase the risk of sudden cardiac arrest, requiring immediate medical intervention.
- Blood clots. Due to poor blood flow, untreated DCM can increase the risk of blood clots forming in the heart. These clots may travel to other parts of the body, potentially leading to a stroke or a pulmonary embolism, which can be life-threatening.
- Mitral valve regurgitation. As the heart enlarges, it can affect the mitral valve, which separates the left atrium from the left ventricle. This valve may not close properly, allowing blood to leak backward into the left atrium. Mitral valve regurgitation further weakens the heart and worsens symptoms.
- Sudden cardiac arrest. In severe cases, DCM can lead to sudden cardiac arrest, a life-threatening condition where the heart suddenly stops beating. This requires immediate medical attention, as it can result in death if not treated promptly.
These complications highlight the importance of early diagnosis and treatment of DCM. Managing the condition with medications, lifestyle changes, and, in some cases, surgery can help prevent these serious outcomes and improve quality of life.
Causes of Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) can develop due to various direct causes that weaken and enlarge the heart muscle. Here are some of the primary causes known to directly contribute to this condition:
- Genetic inheritance. DCM can be inherited, with certain gene mutations directly affecting heart muscle function. If a close family member has DCM, there is an increased chance of developing the condition due to genetic factors.
- Alcohol toxicity. Chronic excessive alcohol intake can directly damage the heart muscle, leading to a condition known as alcoholic cardiomyopathy. The toxic effects of alcohol weaken the heart’s pumping ability and contribute to the development of DCM.
- Medications and toxins. Certain drugs are directly toxic to the heart muscle. Chemotherapy drugs like doxorubicin and daunorubicin, used in cancer treatment, are known to cause heart damage with prolonged use. Recreational drugs such as cocaine and amphetamines can also severely damage heart muscle, directly contributing to DCM.
- Viral infections. Certain viral infections can lead to myocarditis, an inflammation of the heart muscle that weakens it. Persistent damage from infections like coxsackievirus and cytomegalovirus can result in the development of DCM.
- Other medical conditions. Some diseases directly impact heart function and can lead to DCM. For example, thyroid disease can alter metabolism in ways that strain the heart, while diabetes can lead to high blood sugar levels that damage blood vessels and the heart muscle.
Addressing these direct causes through appropriate medical management, lifestyle changes, and preventive care can be key in managing DCM and protecting overall heart health.
Prevention of Dilated Cardiomyopathy
Most heart diseases, including dilated cardiomyopathy (DCM), can often be prevented by adopting a healthy lifestyle. Here are some effective ways to reduce the risk of developing DCM:
- Eat a nutritious diet. Focus on balanced meals that are low in saturated fats and sodium. Avoid excessive consumption of fatty and salty foods, which can strain the heart and blood vessels.
- Exercise daily and maintain a healthy weight. Regular physical activity strengthens the heart and helps maintain a healthy weight. If you are overweight, gradual weight loss through exercise and diet can benefit heart health significantly.
- Avoid harmful habits. Limit or eliminate alcohol consumption, and avoid smoking. Both alcohol and tobacco have toxic effects on the heart and can increase the risk of DCM.
- Manage stress and get adequate rest. Reducing stress through relaxation techniques, adequate sleep, and regular breaks can lower the risk of heart complications. Chronic stress can strain the heart and affect overall cardiovascular health.
- Treat underlying health conditions. Manage any existing medical conditions, such as high blood pressure or diabetes, to prevent complications that could lead to DCM. Proper treatment of these conditions is essential in protecting the heart.
- Schedule regular check-ups. Even if you feel healthy, regular check-ups with your doctor are crucial for early detection of any heart-related issues. Since DCM can sometimes be asymptomatic in its early stages, routine exams can help identify potential problems before symptoms arise.
By following these preventative measures, individuals can greatly reduce their risk of developing DCM and other heart conditions. Regular medical consultations play an important role in early detection and treatment, helping to maintain long-term heart health.
Risk Factors for Dilated Cardiomyopathy
Certain groups are more likely to develop dilated cardiomyopathy (DCM) due to various factors, including age, gender, family history, and existing health conditions. Here are some of the main risk groups:
- People aged 20 to 60 years. Individuals within this age range are at a higher risk of DCM. Lifestyle choices, which are often established in this age group, can greatly impact heart health and contribute to the risk of developing DCM if unhealthy habits are adopted.
- Men. Men are more likely to develop DCM compared to women, partially due to higher rates of alcohol consumption. Excessive alcohol intake is a known factor that weakens the heart muscle and increases the likelihood of cardiomyopathy.
- Family history of DCM. If a close family member has DCM, the risk of developing the condition is higher due to genetic factors. However, adopting a healthy lifestyle can still help mitigate the inherited risk.
- Heavy alcohol drinkers. Regardless of gender, individuals who consume excessive alcohol are at risk of DCM. Alcohol not only raises blood pressure but also weakens the heart muscle over time, making it a significant risk factor.
- People with high blood pressure. Chronic high blood pressure can cause the left ventricle to enlarge as it works harder to pump blood. Over time, the increased workload leads to an enlargement of the heart muscle, resulting in DCM.
- Individuals who are overweight. Those with excess body weight are more likely to develop DCM, as obesity often contributes to high blood pressure—a major factor in heart enlargement and strain.
- People with other medical conditions. Health issues such as coronary artery disease, viral infections affecting the heart, thyroid disorders, and diabetes also increase the risk of DCM. When these conditions are unmanaged, they can lead to complications that damage the heart muscle.
By understanding and managing these risk factors, individuals can reduce their likelihood of developing DCM. Regular check-ups and lifestyle adjustments are essential for those at higher risk to maintain heart health and prevent the progression of this condition.
Dilated Cardiomyopathy FAQs
Understanding dilated cardiomyopathy (DCM) can be challenging, and patients often have questions about symptoms, causes, treatments, and lifestyle changes. Here are answers to some frequently asked questions to help clarify this condition.
- What is dilated cardiomyopathy?
DCM is a condition in which the heart’s main pumping chamber, the left ventricle, becomes enlarged and weakened. This makes it harder for the heart to pump blood efficiently, leading to symptoms like fatigue, shortness of breath, and swelling in the legs. - What causes DCM?
DCM can have various causes, including genetic mutations, excessive alcohol consumption, viral infections, certain medications, and conditions like high blood pressure, diabetes, and thyroid disorders. In some cases, the exact cause remains unknown. - Is dilated cardiomyopathy hereditary?
Yes, DCM can be inherited. If there is a family history of DCM, there may be a higher risk of developing the condition. Genetic testing and regular heart monitoring can help those at risk identify and manage the disease early. - What are the symptoms of DCM?
Common symptoms include shortness of breath, fatigue, swelling in the legs, chest pain, and heart palpitations. However, some people may not experience symptoms until the disease progresses to a more advanced stage. - How is DCM diagnosed?
DCM is diagnosed through several tests, such as an echocardiogram, ECG, chest X-ray, blood tests, and sometimes cardiac MRI. These tests help determine the heart’s size, function, and blood flow. - Can DCM be cured?
There is no cure for DCM, but the condition can be managed effectively with lifestyle changes, medications, and sometimes surgical options. With proper treatment, many people with DCM can live long, active lives. - What are the treatment options for DCM?
Treatment often includes medications to improve heart function and relieve symptoms, lifestyle changes, and in some cases, surgery. Options like pacemakers, implantable cardioverter-defibrillators (ICDs), and even heart transplants may be considered for severe cases. - How can I manage DCM at home?
Managing DCM involves adopting a heart-healthy lifestyle: eating a balanced diet, exercising within safe limits, reducing salt intake, avoiding alcohol and smoking, managing stress, and monitoring symptoms regularly. Following medical advice closely can help improve quality of life. - Can DCM cause complications?
Yes, untreated DCM can lead to serious complications, including heart failure, arrhythmias, blood clots, mitral valve regurgitation, and even sudden cardiac arrest. Early treatment is essential to prevent these outcomes. - How often should I see my doctor if I have DCM?
Regular follow-ups are crucial to monitor the condition. Typically, patients should see their doctor every 3 to 6 months or as recommended, depending on the severity of their symptoms and response to treatment.