Summary
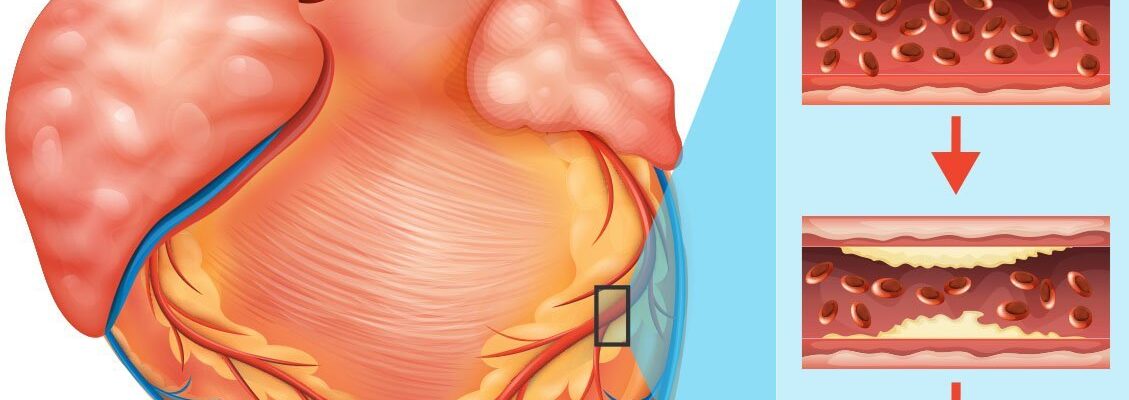
Coronary artery disease (CAD), also known as coronary heart disease (CHD) or ischemic heart disease, is a condition where the coronary arteries that supply oxygen and nutrients to the heart become narrowed or blocked. This restriction is primarily caused by plaque buildup, which limits blood flow and can lead to symptoms such as chest pain (angina), shortness of breath, and, in severe cases, heart attack.
According to the World Health Organization (WHO), CAD is one of the top causes of death globally. Factors contributing to CAD include diets high in fats, lack of exercise, smoking, and excessive alcohol consumption. These behaviors can lead to plaque accumulation, progressively damaging the coronary arteries.
Though CAD is serious, it can be managed through lifestyle changes, medications, and, in advanced stages, surgical procedures. Early diagnosis and proactive treatment can significantly reduce complications and improve heart health.
Table of Contents
- Symptoms of Coronary Artery Disease
- Types of Coronary Artery Disease
- Diagnostic Procedures for Coronary Artery Disease
- Complications of Untreated Coronary Artery Disease
- Causes of Coronary Artery Disease
- Prevention of Coronary Artery Disease
- Risk Factors for Coronary Artery Disease
- Coronary Artery Disease FAQs
Symptoms of Coronary Artery Disease
Coronary artery disease (CAD) presents a variety of symptoms. It is essential to consult a doctor if you experience any of the following:
- Angina. Angina, or chest pain, is the primary symptom of coronary artery disease. It often feels like a heavy pressure or squeezing sensation on the chest and may occur without a clear cause.
- Pain in the jaw, shoulder, arm, or back. Angina can also cause discomfort that radiates to other parts of the body, such as the jaw, shoulders, arms, or back.
- Shortness of breath. Due to restricted blood flow, the heart may struggle to supply enough oxygen to the body, leading to breathlessness, especially during physical activity.
- Cold sweat. Excessive, cold sweating can be an indicator of heart problems, signaling that the body is under stress.
- Dizziness. Dizziness can occur as a result of reduced oxygen and nutrient delivery to the brain, a secondary effect of inadequate blood flow from the heart.
In severe cases, untreated CAD can lead to complications like heart attack, where the heart muscle weakens and temporarily stops pumping blood. During a heart attack, the patient may lose consciousness, requiring immediate chest compressions and emergency medical attention to save their life.
Many people mistakenly dismiss symptoms like angina or chest pain as heartburn or indigestion. While some CAD symptoms can resemble those of less serious conditions, it’s crucial to seek medical advice promptly for accurate diagnosis and timely intervention.
Types of Coronary Artery Disease
Coronary artery disease (CAD) is categorized based on the nature of the artery blockage and its impact on heart function. The main types of CAD are as follows:
- Stable Angina. Stable angina is characterized by chest pain or discomfort that occurs predictably, typically with physical exertion or emotional stress. It is caused by partial blockages in the coronary arteries that limit blood flow. Symptoms are usually relieved by rest or medication and are considered more manageable and predictable than other forms of CAD.
- Unstable Angina. Unstable angina is a more dangerous and unpredictable form of angina that can occur suddenly, even at rest. It is often a sign of worsening blockages and an increased risk of heart attack. Unlike stable angina, unstable angina may not improve with rest or medication and typically requires immediate medical attention.
- Prinzmetal’s Angina (Variant Angina). Prinzmetal’s angina is a rare form of CAD that results from spasms in the coronary arteries, temporarily reducing blood flow to the heart. Symptoms generally occur at rest and can be severe. Unlike other types, this angina is not caused by plaque buildup but by artery spasms, which may be triggered by stress or exposure to cold.
- Silent Ischemia. Silent ischemia refers to reduced blood flow to the heart that occurs without noticeable symptoms, such as chest pain. This condition is often discovered incidentally during an electrocardiogram (ECG) or stress test. Silent ischemia is common in people with diabetes and can increase the risk of heart attack or other complications.
- Acute Coronary Syndrome (ACS). ACS is an umbrella term that includes both heart attacks (myocardial infarction) and high-risk unstable angina. ACS results from a sudden blockage in a coronary artery and can lead to life-threatening complications if not treated promptly. Symptoms include severe chest pain, shortness of breath, and dizziness.
Each type of coronary artery disease requires a unique approach to treatment. Recognizing the signs and understanding the risks of each type can help in seeking timely medical intervention. Regular check-ups and lifestyle changes are critical to managing CAD and supporting heart health.
Diagnostic Procedures for Coronary Artery Disease
Diagnosing coronary artery disease (CAD) involves a variety of tests and evaluations aimed at understanding the extent of coronary blockage, assessing heart function, and identifying any potential complications. These procedures can provide detailed insight into heart health and guide appropriate treatment plans.
- Electrocardiogram (ECG or EKG). This test records the heart’s electrical activity, revealing any irregular heart rhythms or evidence of a past heart attack. An ECG can be conducted at rest or during exercise (stress test) to assess heart performance under different conditions.
- Stress Test. During a stress test, the heart’s function is evaluated while the patient exercises on a treadmill or stationary bike. For those unable to exercise, medications can be given to simulate the effects of physical activity. This test helps in detecting abnormal heart rhythms, assessing blood flow, and identifying possible blockages.
- Echocardiogram. This ultrasound test provides a moving image of the heart, allowing doctors to assess its size, shape, and function. Echocardiograms can detect areas with poor blood flow, heart valve issues, and the overall health of the heart muscle.
- Coronary Angiography. Often considered the gold standard for diagnosing CAD, coronary angiography involves injecting a special dye into the coronary arteries. X-rays then capture images of blood flow, revealing any narrow or blocked arteries and the severity of blockages.
- CT Coronary Angiography. A less invasive alternative to traditional angiography, this procedure uses a CT scanner to capture detailed 3D images of the heart and coronary arteries. It’s especially useful for detecting early plaque buildup and diagnosing CAD in patients with atypical symptoms.
- Blood Tests. Blood tests can measure cholesterol levels, triglycerides, and markers of inflammation, all of which contribute to CAD risk. Troponin levels may also be checked if a recent heart attack is suspected, as this protein is released when heart muscle cells are damaged.
- Nuclear Heart Scan. This test uses a small amount of radioactive material to produce detailed images of blood flow to the heart muscle. A nuclear heart scan, such as a myocardial perfusion scan, can help detect regions with insufficient blood supply and assess the heart’s pumping efficiency.
Each of these diagnostic procedures plays a vital role in diagnosing CAD and assessing its severity. Depending on individual health profiles and symptoms, doctors may recommend one or more of these tests to accurately determine the best treatment approach.
Complications of Untreated Coronary Artery Disease
If left untreated, coronary artery disease (CAD) can lead to serious health complications. These issues arise from the ongoing restriction of blood flow to the heart, which can weaken heart muscles and affect overall circulation, ultimately threatening life.
- Heart Attack. Blocked arteries can cut off blood flow to portions of the heart muscle, causing a heart attack. This leads to the death of heart tissue, which can result in permanent heart damage and, if severe, death.
- Heart Failure. Over time, CAD can weaken the heart muscle, making it less effective at pumping blood. This condition, known as heart failure, can lead to symptoms such as fatigue, shortness of breath, and fluid buildup in the lungs and other parts of the body.
- Arrhythmia. Reduced blood flow or damage to the heart muscle can lead to arrhythmias, or irregular heart rhythms. Some arrhythmias are minor, while others can increase the risk of sudden cardiac arrest.
- Angina. Untreated CAD can lead to frequent episodes of angina, which is chest pain resulting from restricted blood flow to the heart. This pain can limit physical activity and affect quality of life.
- Stroke. CAD can also lead to blood clots that may travel to the brain, causing a stroke. A stroke can lead to permanent disability or death, depending on the severity of the blockage in the brain’s blood vessels.
- Sudden Cardiac Arrest. In severe cases, CAD can cause the heart to stop suddenly, leading to sudden cardiac arrest. This condition is life-threatening and requires immediate medical attention.
The complications of untreated CAD can severely impact a person’s health, often with life-threatening outcomes. Early diagnosis and treatment are crucial to prevent these serious complications, improve quality of life, and prolong life expectancy.
Causes of Coronary Artery Disease
The primary cause of coronary artery disease (CAD) is the buildup of plaque within the coronary arteries, which restricts blood flow to the heart muscle. This buildup, known as atherosclerosis, is the direct cause of CAD and is driven by several physiological processes:
- Cholesterol and lipid deposits. Plaque forms when cholesterol, fats, and other substances accumulate on the inner walls of the coronary arteries. Over time, these deposits harden and narrow the arteries, reducing or blocking blood flow.
- Inflammation of artery walls. Inflammation can damage the inner lining (endothelium) of the coronary arteries, making it easier for cholesterol and other substances to adhere to the walls and form plaque. Chronic inflammation is a direct contributor to the development and progression of atherosclerosis.
- Blood clot formation. Plaque buildup can sometimes rupture, causing a blood clot to form at the site. When a blood clot partially or completely blocks a coronary artery, it restricts blood flow, leading to symptoms like chest pain or, in severe cases, a heart attack.
- Calcification of plaque. As plaque accumulates, calcium deposits may also build up within the artery walls, causing them to stiffen. This process, known as arterial calcification, further narrows the arteries and impairs blood flow to the heart.
These direct causes lead to a narrowing or blockage of the coronary arteries, reducing blood and oxygen supply to the heart. Over time, untreated CAD can lead to serious complications, including heart attacks and heart failure.
Prevention of Coronary Artery Disease
To help prevent coronary artery disease (CAD), it’s recommended to adopt the following lifestyle practices:
- Eat nutritious foods. Choosing a healthy diet helps reduce risk factors associated with CAD, such as high blood pressure, obesity, and diabetes. Focus on eating plenty of vegetables, fruits, and fish rich in omega-3 fatty acids (healthy fats). Limit fatty cuts of meat and foods high in saturated fats to prevent elevated cholesterol levels.
- Exercise daily. Engaging in at least 30 minutes of exercise each day can help maintain a healthy weight. Regular physical activity also lowers cholesterol levels, reduces blood pressure, and strengthens heart health.
- Quit smoking. Smoking is a major contributor to heart disease, as well as lung diseases and many other health problems. Quitting smoking lowers the risk of CAD and helps improve overall health.
- Limit alcohol intake. Excessive alcohol consumption can raise blood pressure, increasing the risk of CAD. If you choose to drink, it’s best to do so in moderation and ideally only on special occasions.
Adopting these healthy lifestyle practices significantly lowers the risk of developing coronary artery disease. However, if you experience any symptoms of CAD, it’s important to seek medical advice promptly to prevent the condition from progressing.
Risk Factors for Coronary Artery Disease
The risk of developing coronary artery disease (CAD) is higher for individuals in the following groups:
- Those with high blood pressure and high cholesterol. One of the primary risk factors for CAD is elevated blood pressure and cholesterol levels. People with a blood pressure consistently at or above 140/80 mmHg or with cholesterol levels exceeding 240 mg/dL are at increased risk of CAD.
- Individuals who are overweight. People who are overweight or obese are at higher risk for CAD due to the presence of excess body fat, particularly saturated fats, which can contribute to arterial blockages.
- Those who frequently consume high-fat foods. Even individuals who are not overweight can still be at risk for CAD if they frequently consume foods high in saturated fats. These foods can raise blood pressure and cholesterol levels, increasing the likelihood of artery blockage.
- Smokers. Individuals who smoke heavily (more than one pack per day) face a significantly higher risk of CAD. The toxic chemicals in cigarettes promote blood clots, which can lead to blocked coronary arteries.
- Heavy drinkers. Excessive alcohol consumption raises blood pressure and weakens heart muscles, increasing the risk of coronary artery disease.
- People with other medical conditions. Individuals with diabetes or sleep apnea, for instance, have an increased risk of CAD, as these conditions can lead to complications that contribute to the narrowing or blockage of coronary arteries.
These risk factors contribute to the buildup of plaque in the coronary arteries, reducing blood flow to the heart. By managing these conditions and making healthy lifestyle choices, individuals can lower their risk of developing CAD.
Coronary Artery Disease FAQs
Coronary artery disease (CAD) can be a complex condition to understand, and patients often have many questions about its causes, symptoms, treatments, and more. Here are answers to some frequently asked questions to provide clarity on CAD and how it affects heart health.
- What causes coronary artery disease?
CAD is primarily caused by the buildup of plaque—consisting of cholesterol, fat, and other substances—in the coronary arteries. This buildup, known as atherosclerosis, restricts blood flow to the heart, potentially leading to heart attacks, angina, and other complications. - What are the symptoms of CAD?
Common symptoms include chest pain (angina), shortness of breath, fatigue, and discomfort in the shoulders, arms, or jaw. However, some people may not experience symptoms until the disease has progressed significantly, increasing the risk of a sudden heart attack. - How is CAD diagnosed?
CAD is typically diagnosed using various tests, including an electrocardiogram (ECG), stress test, echocardiogram, coronary angiography, and blood tests. A healthcare provider will choose the appropriate tests based on symptoms, risk factors, and medical history. - Can coronary artery disease be cured?
While CAD cannot be completely cured, it can be effectively managed. Lifestyle changes, medications, and surgical procedures like angioplasty or bypass surgery can help control symptoms, reduce risk, and improve quality of life. - What lifestyle changes can help manage CAD?
Important lifestyle changes include quitting smoking, maintaining a healthy weight, following a heart-healthy diet, exercising regularly, and managing stress. These changes can slow disease progression and help prevent complications. - What are common treatments for CAD?
Treatment options vary based on disease severity but may include medications to lower blood pressure and cholesterol, manage angina, and reduce blood clots. In advanced cases, procedures like angioplasty or coronary artery bypass surgery may be recommended. - Is CAD hereditary?
Yes, a family history of CAD can increase a person’s risk of developing the disease. However, lifestyle factors, such as diet, exercise, and smoking, also play a significant role in the risk of developing CAD. - Can women experience different CAD symptoms than men?
Yes, women may experience less typical CAD symptoms, such as nausea, fatigue, shortness of breath, or discomfort in the neck or jaw. This difference in symptoms can sometimes delay diagnosis and treatment in women. - How does stress affect CAD?
Chronic stress can increase CAD risk by contributing to high blood pressure, poor lifestyle habits (such as overeating or smoking), and increased inflammation. Managing stress through exercise, mindfulness, or relaxation techniques can be beneficial. - How often should I see a doctor if I have CAD?
Routine follow-ups are essential for managing CAD. The frequency depends on individual health, risk factors, and treatment plans. Typically, patients with CAD should see a healthcare provider every 3 to 6 months or as recommended.