Summary
The heart cannot begin to beat without receiving an electrical signal from the sinus node, a part of the heart located in the upper right chamber or right atrium. The sinus node functions as the heart’s natural pacemaker, regulating the proper rhythm and speed of each heartbeat. Damage to the sinus node can lead to a condition known as atrioventricular (AV) block, also referred to as heart block.
In AV block, the electrical signal is delayed or blocked from traveling between the upper chambers (atria) and lower chambers (ventricles) of the heart. This interruption can occur if the patient has certain underlying health conditions, such as idiopathic fibrosis, sclerosis, ischemic heart disease, congenital heart defects, and others. These conditions disrupt the heart’s electrical pathways, making it difficult for the heart to maintain a regular rhythm.
Patients with AV block may experience symptoms such as irregular heartbeat, shortness of breath, dizziness or fainting, chest tightness, and fatigue. Treatment options for AV block may include medication to manage symptoms or, in more advanced cases, the implantation of an artificial pacemaker to help maintain a steady heart rhythm.
Table of Contents
- Symptoms of Atrioventricular Block (Heart Block)
- Types of Atrioventricular Block (Heart Block)
- Diagnostic Procedures for Atrioventricular Block (Heart Block)
- Complications of Untreated Atrioventricular Block (Heart Block)
- Causes of Atrioventricular Block (Heart Block)
- Prevention of Atrioventricular Block (Heart Block)
- Risk Factors for Atrioventricular Block (Heart Block)
- Atrioventricular Block (Heart Block) FAQs
Symptoms of Atrioventricular Block (Heart Block)
If a patient experiences the following symptoms, they may have AV block:
- Irregular heartbeat. In AV block, not all signals from the sinus node reach the ventricles, leading to an irregular heartbeat. This often results in a slower heart rate, with skipped or delayed beats.
- Shortness of breath. AV block can cause the heart to beat too slowly to supply sufficient blood and oxygen to the lungs, resulting in shortness of breath, especially during physical activity.
- Dizziness and fainting. The brain, like the lungs, requires a constant supply of blood and oxygen. When the heart cannot pump effectively due to AV block, the reduced blood flow can cause dizziness or even fainting spells.
- Chest tightness. Like other heart conditions, AV block may lead to chest discomfort or tightness, which can worsen with physical exertion as the heart struggles to meet the body’s demands.
- Fatigue. Due to the slower heart rate and reduced blood flow, the body’s organs and muscles may not receive adequate nutrients and oxygen, leading to frequent and easy fatigue.
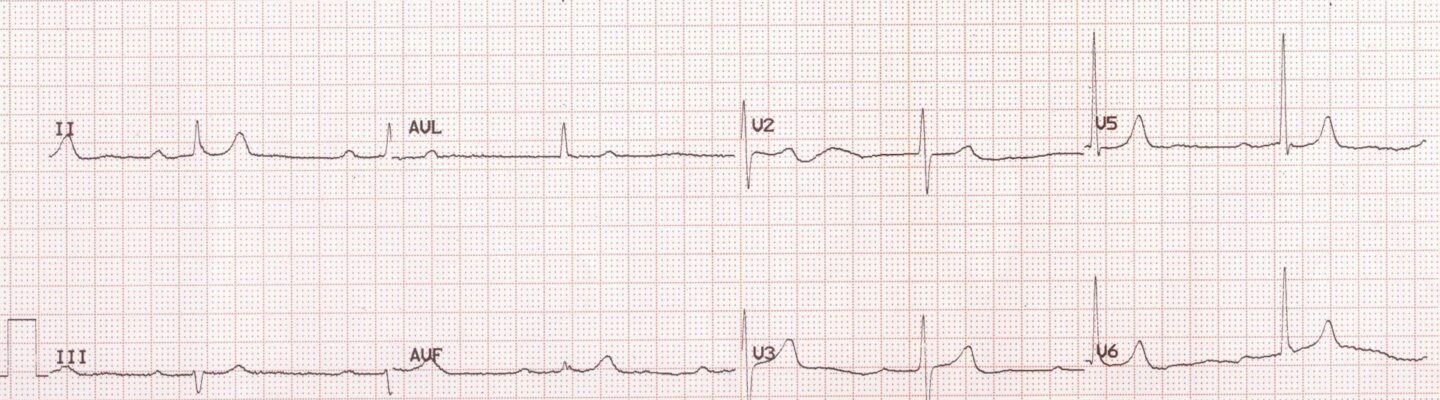
Identifying AV block can be challenging without diagnostic testing, as its symptoms are similar to those of other heart conditions. The most common test to confirm AV block is an electrocardiogram (ECG), in which electrodes are placed on the patient’s chest to monitor the heart’s electrical activity. The ECG results allow doctors to observe the heart’s rhythm and detect any delays or irregularities in its beats, confirming an AV block diagnosis if present.
Types of Atrioventricular Block (Heart Block)
Atrioventricular (AV) block, or heart block, is classified into three categories based on severity. Here are the three types of AV block:
- First-degree AV block. First-degree AV block is the least dangerous type of AV block. Although the electrical signal from the sinus node to the ventricles is delayed, it still reaches its destination. Patients with first-degree AV block may or may not experience symptoms. If asymptomatic, treatment may not be required; however, regular monitoring is essential to ensure the condition doesn’t worsen.
- Second-degree AV block. Second-degree AV block is more serious than first-degree. In this type, some electrical signals do not reach the ventricles, causing a slower heartbeat. Second-degree AV block is further divided into two subtypes:
- Mobitz Type I (Wenckebach’s AV block). In this subtype, the delay of electrical signals gradually increases until a heartbeat is skipped. While Mobitz Type I is typically not life-threatening, it does require monitoring.
- Mobitz Type II (Hay AV block). In Mobitz Type II, the electrical signals are irregular, and some fail to reach the ventricles altogether. This results in a very slow heart rate with multiple skipped beats, making it more dangerous than Type I.
- Third-degree AV block. Known as complete AV block, third-degree AV block is the most severe form. In this condition, none of the electrical signals from the sinus node reach the ventricles, causing the heart rate to slow significantly and become extremely weak. Without prompt treatment, third-degree AV block can be life-threatening.
Each type of AV block affects the heart’s rhythm and requires varying levels of intervention. Early diagnosis and treatment are crucial, especially for second- and third-degree AV blocks, to prevent serious complications.
Diagnostic Procedures for Atrioventricular Block (Heart Block)
AV block occurs when there is a delay or interruption in the electrical signals between the heart’s upper chambers (atria) and lower chambers (ventricles). Detecting and assessing AV block requires specific diagnostic tests that provide insight into the heart’s electrical activity and function. Below are the primary diagnostic procedures for AV block:
- Electrocardiogram (ECG or EKG). The ECG is the primary diagnostic tool for AV block. It records the heart’s electrical signals and helps identify the presence and type of AV block by showing any delays or irregularities in the signals moving from the atria to the ventricles.
- Holter monitor. A Holter monitor is a portable ECG device that continuously records the heart’s electrical activity over 24 to 48 hours. This test is beneficial for detecting intermittent AV block or irregularities that may not appear during a standard ECG.
- Event monitor. For individuals who experience symptoms infrequently, an event monitor can be worn over a longer period, usually up to several weeks. The patient activates the monitor whenever symptoms occur, allowing doctors to capture heart rhythms during those episodes.
- Exercise stress test. This test monitors the heart’s electrical activity while the patient exercises, typically on a treadmill or stationary bike. An exercise stress test can help detect AV block that occurs specifically during physical activity and assess the heart’s response to stress.
- Electrophysiology (EP) study. In an EP study, catheters are inserted through blood vessels and guided to the heart to precisely map its electrical pathways. This test provides detailed information on where electrical signal delays occur, helping doctors determine the specific type of AV block and plan for potential treatments.
- Blood tests. Blood tests may be performed to check for underlying conditions that can contribute to AV block, such as electrolyte imbalances, thyroid disorders, or infections. While not specific to AV block, these tests help identify contributing factors that may require management.
These diagnostic procedures are essential for identifying AV block and determining its severity and type. Once the AV block is confirmed, doctors can tailor a treatment plan that may include medications, lifestyle changes, or, in more severe cases, pacemaker implantation to regulate the heart’s rhythm and maintain adequate blood flow. Early diagnosis and intervention are critical for preventing complications and ensuring optimal heart health.
Complications of Untreated Atrioventricular Block (Heart Block)
When AV block is left untreated, the heart’s ability to maintain a steady and effective rhythm is compromised, potentially leading to serious health complications. The severity of these complications depends on the degree of heart block and the underlying causes. Below are the primary complications that can arise from untreated AV block:
- Bradycardia (slow heart rate). AV block often causes a significant reduction in heart rate, which may lead to bradycardia. If the heart rate drops too low, the body’s organs and tissues may not receive adequate blood flow and oxygen, resulting in symptoms like fatigue, dizziness, and fainting.
- Heart failure. Prolonged disruption in the heart’s electrical signaling can weaken the heart muscle over time, eventually leading to heart failure. In this condition, the heart is unable to pump blood effectively, which can cause fluid buildup in the lungs and other parts of the body, leading to shortness of breath, swelling, and fatigue.
- Syncope (fainting spells). AV block can cause sudden and unpredictable fainting episodes due to reduced blood flow to the brain. This can be dangerous, as it increases the risk of falls, injury, and accidents, particularly in individuals with severe AV block.
- Sudden cardiac arrest. In severe cases of AV block, particularly third-degree (complete) AV block, the heart’s electrical system may fail entirely. Without prompt intervention, this can lead to sudden cardiac arrest, where the heart stops beating effectively, cutting off blood flow to vital organs. Sudden cardiac arrest is life-threatening and requires immediate medical attention.
- Cognitive impairment. Chronic low blood flow to the brain due to untreated AV block can result in cognitive decline and memory problems over time. This is especially prevalent in older adults, as the brain is particularly vulnerable to prolonged oxygen deprivation.
- Permanent organ damage. When the heart cannot maintain adequate blood flow, organs like the kidneys, liver, and brain can suffer from long-term oxygen deprivation, leading to tissue damage. This organ damage may become irreversible if left untreated for an extended period.
The complications of untreated AV block highlight the importance of early diagnosis and timely intervention. Treatment options, such as medications or pacemaker implantation, can help manage the condition effectively, reduce symptoms, and prevent life-threatening complications. Regular follow-ups with a healthcare provider are crucial for those diagnosed with any degree of AV block to monitor heart health and avoid potential risks.
Causes of Atrioventricular Block (Heart Block)
There are several direct causes of AV block, many of which disrupt the heart’s electrical pathways or damage the sinus node. These causes include:
- Congenital heart defect. Certain congenital heart defects, especially those involving the right atrium where the sinus node is located, can directly interfere with electrical signaling and lead to AV block.
- Ischemic heart disease. Ischemic heart disease restricts blood flow to the heart muscle, which can damage or weaken the sinus node and interrupt the transmission of electrical signals from the atria to the ventricles, resulting in AV block.
- Idiopathic fibrosis. Idiopathic fibrosis, or scarring of the heart tissue, can interfere with the heart’s electrical system. This scarring affects the sinus node’s ability to generate signals consistently, directly leading to AV block.
- Sclerosis. Some types of sclerosis, such as multiple sclerosis, may impact the body’s nervous system, disrupting the heart’s ability to conduct electrical signals efficiently and leading to AV block.
- Certain medications. Some drugs can interfere with the heart’s electrical impulses. Medications like beta blockers, calcium channel blockers, digoxin, and amiodarone can slow or block signal transmission within the heart.
These direct causes interfere with the heart’s natural electrical conduction system, resulting in slowed or blocked signals and leading to AV block.
Prevention of Atrioventricular Block (Heart Block)
If a person is born with structural issues in the atrium, AV block may be unavoidable. However, for those without congenital issues, maintaining heart health can help reduce the risk of developing AV block. Here are some ways to keep your heart healthy:
- Eat foods rich in omega-3, phytonutrients, and fiber. These nutrients, found in fruits, vegetables, and fish, support heart health by reducing inflammation and promoting healthy cholesterol levels.
- Avoid salty and fatty cuts of meat. Limiting high-sodium and high-fat foods can help reduce the risk of artery blockage, which in turn supports healthy blood flow and reduces heart strain.
- Drink eight glasses of water daily. Staying well-hydrated helps the kidneys flush out excess salt from the body, supporting balanced blood pressure and overall heart health.
- Exercise for at least 30 minutes a day. Regular physical activity promotes healthy circulation, helps maintain a healthy weight, and strengthens the heart muscle.
- Avoid harmful habits like smoking and excessive alcohol consumption. Both smoking and heavy drinking introduce toxins that can harm the heart and blood vessels, increasing the risk of heart conditions.
- Get sufficient rest and sleep. Adequate sleep helps the heart recover and reduces stress on the cardiovascular system.
Second- and third-degree AV block can pose significant health risks if not treated promptly. Regular check-ups with a healthcare provider are essential to monitor heart health and address any potential issues early.
Risk Factors for Atrioventricular Block (Heart Block)
Both men and women can develop AV block, but the risk is higher for those in the following groups:
- Older adults. As people age, the heart muscle may weaken or sustain damage due to gradual degeneration. To compensate, the heart (particularly the atria and ventricles) has to work harder, which can eventually lead to damage affecting the sinus node and increasing the risk of AV block.
- Family history of AV block. If there is a family history of AV block, there is an elevated risk of developing the condition, especially without careful attention to heart health.
- Smokers. Smokers have a higher likelihood of developing AV block. Cigarettes contain nicotine and other toxic substances that can damage the heart muscle, specifically the atrium, and impair the sinus node’s ability to send electrical signals to the ventricles effectively.
- Individuals who have had heart surgery. People who have undergone heart surgery are at an increased risk of developing AV block. Although heart surgery aims to improve cardiac health, it can leave scars that, if not managed properly, may impact the atria and interfere with the sinus node’s function.
- Individuals with other heart conditions. Conditions such as cardiomyopathy, coronary thrombosis, myocarditis, and endocarditis can also increase the risk of AV block. These heart diseases can lead to additional complications and cause direct damage to the heart muscle.
Each of these factors can elevate the risk of AV block, making it essential for individuals in these groups to monitor their heart health closely and consult with a healthcare provider regularly.
Atrioventricular Block (Heart Block) FAQs
Atrioventricular (AV) block, or heart block, affects the heart’s electrical system and can vary in severity. These FAQs cover common questions about AV block, including causes, symptoms, treatments, and when to seek medical attention.
- What is atrioventricular block (AV block) or heart block?
AV block, also known as heart block, is a condition where the electrical signals between the heart’s upper chambers (atria) and lower chambers (ventricles) are delayed or blocked. This can result in a slower heart rate or irregular heartbeats, affecting the heart’s ability to pump blood effectively. - What are the different types of AV block?
There are three main types of AV block:- First-degree AV block: The electrical signals are delayed but still reach the ventricles. It’s the mildest form and often doesn’t require treatment.
- Second-degree AV block: Some signals don’t reach the ventricles, resulting in occasional missed heartbeats. This type has two subtypes: Mobitz Type I (Wenckebach) and Mobitz Type II.
- Third-degree (complete) AV block: No electrical signals from the atria reach the ventricles, leading to a very slow or unstable heart rate. It’s the most severe type and requires immediate treatment.
- What causes AV block?
AV block can be caused by congenital heart defects, ischemic heart disease, scarring from previous heart conditions, certain medications, and other heart conditions like myocarditis. In some cases, AV block may be present from birth due to genetic factors. - What are the symptoms of AV block?
Symptoms vary depending on the type and severity of the block but may include dizziness, fainting, fatigue, shortness of breath, chest pain, and an unusually slow or irregular heart rate. Some people with mild AV block may not experience any symptoms. - How is AV block diagnosed?
AV block is typically diagnosed with an electrocardiogram (ECG), which records the heart’s electrical activity. For intermittent symptoms, a Holter monitor or event monitor may be used. In certain cases, an electrophysiology (EP) study may be performed for a more detailed assessment. - Is AV block dangerous?
The severity of AV block depends on the type. First-degree AV block is often benign and may not require treatment. However, second- and third-degree AV blocks can be more dangerous, especially if they lead to symptoms like fainting or heart failure, and may require prompt intervention. - How is AV block treated?
Treatment varies based on the type and severity of the AV block. Mild cases may only require regular monitoring. More severe cases, especially third-degree AV block, may require the implantation of a pacemaker, which helps regulate the heart rate. Medications may also be used to manage underlying conditions contributing to AV block. - Can AV block be prevented?
While congenital AV block cannot be prevented, maintaining a heart-healthy lifestyle can reduce the risk of developing AV block due to other heart conditions. This includes regular exercise, a balanced diet, avoiding smoking, and managing blood pressure and cholesterol. - Is AV block hereditary?
In some cases, AV block may be hereditary, especially if it is present from birth as a congenital condition. If there is a family history of heart block, it’s advisable to have regular check-ups with a healthcare provider to monitor heart health. - Do people with AV block need a pacemaker?
Not everyone with AV block requires a pacemaker. Patients with third-degree (complete) AV block or symptomatic second-degree AV block may need a pacemaker to help regulate their heart rhythm. Your doctor will assess the severity of the block and determine if a pacemaker is necessary. - Can AV block progress over time?
Yes, in some cases, AV block can progress from one degree to a more severe degree. Regular follow-up with a healthcare provider is essential for monitoring any progression and adjusting the treatment plan as needed. - What is the outlook for someone with AV block?
With proper diagnosis and treatment, many people with AV block can live a normal, healthy life. First-degree AV block often has a favorable outlook, while second- and third-degree AV blocks may require ongoing management but can still be effectively treated, especially with the use of a pacemaker if needed. - When should I see a doctor if I suspect AV block?
If you experience symptoms like dizziness, fainting, shortness of breath, or a noticeably slow or irregular heartbeat, it’s important to consult a healthcare provider. Early diagnosis and treatment can prevent complications and help maintain a healthy heart.