Summary
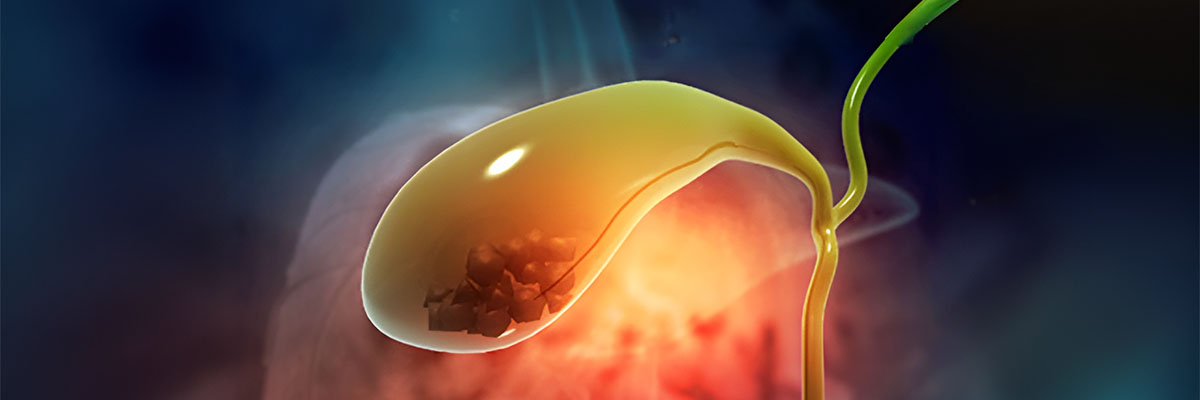
Gallstones are solid particles that form in the gallbladder, a small organ beneath the liver. These stones develop when substances in the bile, such as cholesterol or bilirubin, become imbalanced and harden. The stones can vary in size, and some may not cause any symptoms, while others can lead to painful conditions.
Common symptoms of gallstones include intense pain in the upper abdomen, nausea, vomiting, fever, bloating, indigestion, and jaundice (yellowing of the skin or eyes).
While there are medications available to dissolve gallstones, surgery is often the best approach to fully remove them and prevent complications.
Table of Contents
Symptoms of Gallstones
Gallstones often do not cause symptoms right away. Many individuals are unaware they have gallstones until the condition worsens and the symptoms become more pronounced. Once these symptoms begin, they can be uncomfortable and even debilitating, particularly after eating certain foods.
Here are some of the common symptoms associated with gallstones:
- Pain in the right upper abdomen. This is one of the hallmark symptoms of gallstones. The pain usually occurs in the upper right side of the abdomen and can be sharp or cramping. It often comes in waves and may last from 30 minutes to five hours. The discomfort tends to worsen after eating fatty meals and is more likely to occur at night.
- Sensitivity to fatty and greasy foods. Individuals with gallstones may find it difficult to tolerate high-fat foods. These meals can trigger or worsen symptoms like discomfort, bloating, and indigestion.
- Indigestion, excessive burping, and bloating. Gallstones can cause digestive issues, leading to feelings of fullness or bloating, frequent burping, and indigestion, especially after eating.
- Nausea, vomiting, and dizziness. These symptoms may accompany the pain and are often related to the body’s difficulty in processing certain foods due to the presence of gallstones.
- Fever. A fever may develop if a gallstone causes an infection or blocks the bile duct, indicating a more severe complication that requires medical attention.
- Yellowing of the skin and eyes (jaundice). Gallstones can block the flow of bile, leading to a buildup of bilirubin in the blood. This results in jaundice, where the skin and eyes take on a yellowish tint.

If any of these symptoms occur, especially if they are accompanied by fever or jaundice, it is important to seek medical advice. Early diagnosis and treatment can prevent complications such as infections or more severe conditions related to blocked bile ducts.
Types of Gallstones
There are different types of gallstones that can form in the gallbladder, each with its own characteristics and causes. Understanding the types of gallstones can help in determining the best treatment options.
Here are the main types of gallstones:
- Cholesterol gallstones. This is the most common type of gallstone. These stones are primarily made of undissolved cholesterol and often appear yellowish in color. Cholesterol gallstones form when the liver produces more cholesterol than the bile can dissolve, leading to solid particles that accumulate and form stones.
- Pigment gallstones. These gallstones are typically black or brown and form due to an excess of bilirubin in the bile. Bilirubin is a substance produced when the body breaks down red blood cells. When there is too much bilirubin, it can combine with other components in the bile to create hard stones.
Understanding which type of gallstone is present is important for determining treatment. Cholesterol stones may respond to certain medications, while pigment stones are often linked to other conditions like liver disease or blood disorders. In both cases, surgical removal of the gallbladder may be recommended if the stones cause severe symptoms or complications.
Diagnostic Procedures for Gallstones
Gallstones can be difficult to detect in their early stages, especially if they do not cause noticeable symptoms. However, once symptoms appear or if gallstones are suspected, several diagnostic tests can be used to confirm their presence and assess the extent of the condition. Here are the key diagnostic procedures for gallstones:
- Ultrasound. This is the most common and non-invasive method for detecting gallstones. An ultrasound uses sound waves to create an image of the gallbladder and can reveal the presence, size, and number of stones. It is highly effective in identifying cholesterol stones and monitoring any complications like inflammation.
- Abdominal CT scan. A computed tomography (CT) scan provides a more detailed image of the abdominal area and can detect gallstones, as well as other possible issues with the liver, pancreas, or bile ducts. It is often used if ultrasound results are inconclusive or if there is suspicion of complications.
- Magnetic resonance cholangiopancreatography (MRCP). This specialized MRI scan focuses on the bile ducts, liver, and pancreas. It offers high-resolution images that can identify gallstones lodged in the bile ducts, as well as other abnormalities in the biliary system. MRCP is particularly useful for detecting stones that may not be visible on a standard ultrasound.
- Endoscopic retrograde cholangiopancreatography (ERCP). This is both a diagnostic and therapeutic procedure. During ERCP, a flexible tube with a camera is passed through the mouth and down to the bile ducts to visually inspect for blockages or gallstones. If gallstones are found, they can sometimes be removed during this procedure.
- Blood tests. While blood tests cannot directly detect gallstones, they can help identify signs of infection, inflammation, or liver dysfunction. Elevated levels of certain enzymes or bilirubin in the blood may indicate a blockage or other complications caused by gallstones.
These diagnostic tools help doctors confirm the presence of gallstones and determine the most appropriate treatment plan, whether that involves medication, surgery, or other interventions.
Complications of Untreated Gallstones
If left untreated, gallstones can lead to serious complications that can affect not only the gallbladder but also other organs in the digestive system. While some gallstones may remain asymptomatic, others can cause blockages or infections that require urgent medical attention. Here are some of the potential complications of untreated gallstones:
- Cholecystitis (Inflammation of the Gallbladder). This occurs when a gallstone blocks the cystic duct, causing bile to build up in the gallbladder. The resulting inflammation can lead to severe pain, fever, and infection. If not treated promptly, cholecystitis can cause the gallbladder to rupture, which is a medical emergency.
- Bile Duct Obstruction. Gallstones can migrate from the gallbladder and block the bile ducts, preventing bile from flowing properly into the intestines. This can cause severe pain, jaundice (yellowing of the skin and eyes), and infection. Blockages in the bile ducts can also lead to liver damage or pancreatitis.
- Pancreatitis. If a gallstone blocks the pancreatic duct, it can trigger inflammation of the pancreas, known as pancreatitis. This condition causes intense abdominal pain, nausea, and vomiting, and can become life-threatening if not treated. Pancreatitis may require hospitalization and, in severe cases, surgery.
- Gallbladder Empyema. Empyema is the collection of pus inside the gallbladder, usually as a result of a bacterial infection following a blockage. It can cause severe abdominal pain, fever, and sepsis (a life-threatening infection that spreads throughout the body). Immediate medical intervention is required to drain the pus and treat the infection.
- Gallstone Ileus. A rare but serious complication, gallstone ileus occurs when a large gallstone passes into the intestines and causes a bowel obstruction. This can lead to severe abdominal pain, vomiting, and bloating, and usually requires surgical intervention to remove the blockage.
- Gallbladder Cancer. Although rare, chronic inflammation from untreated gallstones can increase the risk of developing gallbladder cancer. Gallstones are a major risk factor for this type of cancer, especially in cases where gallstones have been present for many years.
Untreated gallstones can have life-threatening consequences, so it is crucial to seek medical advice if symptoms such as severe abdominal pain, fever, jaundice, or digestive issues arise. Early treatment can help prevent these complications and improve overall health outcomes.
Causes of Gallstones
Gallstones are the most common cause of gallbladder disease. These stones can interfere with the normal flow of bile, a digestive fluid produced by the liver and stored in the gallbladder. When gallstones block the bile ducts, bile cannot flow out of the gallbladder properly, which can also disrupt the flow of digestive enzymes from the pancreas.
If the blockage persists, both the gallbladder and pancreas can become inflamed. This inflammation is known as cholecystitis when it affects the gallbladder and pancreatitis when it involves the pancreas. These conditions can lead to various complications and infections if left untreated.
While the exact cause of gallstone formation remains unclear, several factors are believed to contribute to their development:
- Excess cholesterol in the bile. Normally, bile contains enough chemicals to dissolve the cholesterol produced by the liver. However, if the liver secretes more cholesterol than the bile can dissolve, the excess cholesterol can crystallize and form stones.
- Excess bilirubin in the bile. Bilirubin is a chemical produced when the body breaks down red blood cells, a process carried out by the liver. Certain conditions can cause the liver to produce too much bilirubin, leading to the formation of pigment gallstones, which are often black or brown in color.
- Inadequate emptying of the gallbladder. If the gallbladder doesn’t empty efficiently, bile can become overly concentrated. This allows particles in the bile to stick together and harden into gallstones over time.
While gallstone formation is not always preventable, being aware of these contributing factors can help individuals understand their risks. Maintaining a healthy diet, staying active, and managing underlying health conditions can reduce the likelihood of developing gallstones. If gallstones do form, early detection and treatment are key to avoiding further complications.
Prevention of Gallstones
While certain factors that increase the risk of developing gallstones—such as age, gender (more common in women), and ethnicity—cannot be controlled, there are several lifestyle changes that can significantly reduce the risk of gallstone formation.
Here are some effective ways to help prevent gallstones:
- Adopting a vegetarian diet. Studies have shown that individuals who consume a diet rich in vegetables have a lower risk of developing gallstones. Vegetables are high in fiber and contain significantly less fat than meat, making them beneficial for maintaining a healthy gallbladder.
- Limiting intake of fatty foods. While some individuals may need to include meat in their diet due to medical conditions, it’s essential to choose lean meats and consume them in moderation. Avoiding excessive intake of high-fat foods can help reduce the likelihood of gallstones forming.
- Maintaining a healthy weight. Weight management plays an important role in gallstone prevention. However, it’s crucial to lose weight gradually and in a healthy manner, as rapid weight loss can actually increase the risk of gallstones.
- Eating smaller meals. Instead of eating large portions in one sitting, try eating smaller, more frequent meals. This approach helps the digestive system process food more efficiently, reducing the risk of gallstone formation.
- Drinking plenty of water. Staying well-hydrated supports healthy digestion and helps the body process food more effectively. Make it a habit to drink plenty of water throughout the day to aid digestion and reduce gallstone risk.

By following these preventive measures, individuals can help lower their chances of developing gallstones, improving overall digestive health and avoiding potential complications. Maintaining a balanced diet, staying active, and focusing on gradual, healthy weight loss are key strategies for long-term prevention.
Risk Factors for Gallstones
Several conditions and lifestyle factors can increase the likelihood of developing gallstones. Understanding these risk factors can help individuals take proactive steps toward prevention.
Here are the common risk factors for gallstones:
- Obesity. Being overweight raises cholesterol levels in the body, making it harder for the gallbladder to empty its contents fully. This increases the chance of gallstone formation as excess cholesterol can crystallize into stones.
- High-fat diet. Consuming large amounts of fatty foods can cause excess fat to accumulate in the gallbladder, which may eventually form gallstones. Diets rich in unhealthy fats can increase the burden on the gallbladder and liver.
- Hormonal changes. Factors such as taking birth control pills, undergoing hormone replacement therapy, or pregnancy can increase the risk of gallstones. These conditions elevate estrogen levels in the body, which can slow the emptying of the gallbladder, leading to stone formation.
- Diabetes. People with diabetes often have high levels of triglycerides, a type of fat in the blood. Elevated triglycerides can contribute to the development of gallstones by affecting the bile composition.
- Cholesterol-lowering medications. Some medications designed to lower blood cholesterol may inadvertently increase cholesterol levels in the bile, raising the risk of gallstone formation as a side effect.
- Rapid weight loss. Losing weight too quickly can trigger the liver to produce more cholesterol, which may then lead to the development of gallstones. Gradual, healthy weight loss is recommended to avoid this risk.
- Fasting. Extended periods of fasting or skipping meals can slow down gallbladder contractions. When the gallbladder does not empty regularly, bile can become concentrated, leading to the formation of stones.
- Genetics. Family history can also play a role in gallstone formation. Gallstones are more common in women, older adults (especially those over 60), and certain ethnic groups, suggesting that genetics can influence susceptibility.
Recognizing these risk factors is crucial for individuals who may be at higher risk. By managing weight, maintaining a balanced diet, and being aware of hormonal or medication-related risks, people can take steps to reduce the likelihood of developing gallstones.
Gallstones FAQs
Here are some frequently asked questions (FAQs) about gallstones to help you better understand the condition:
- What are gallstones?
Gallstones are solid particles that form in the gallbladder, usually from cholesterol or bilirubin in bile. These stones can vary in size and may cause no symptoms or lead to painful complications. - What causes gallstones?
Gallstones develop when there is an imbalance in the substances that make up bile, such as cholesterol or bilirubin. Factors like obesity, a high-fat diet, rapid weight loss, and certain medications can contribute to this imbalance. - What are the symptoms of gallstones?
Common symptoms include severe pain in the upper right abdomen, nausea, vomiting, bloating, and indigestion. Some people may also experience jaundice (yellowing of the skin and eyes) or fever if there is a bile duct obstruction or infection. - Can gallstones go away on their own?
Gallstones do not usually go away on their own. While some may remain asymptomatic, others can cause problems and require treatment. In many cases, if gallstones cause significant pain or complications, surgery to remove the gallbladder is recommended. - How are gallstones diagnosed?
Gallstones are typically diagnosed through imaging tests like ultrasound, CT scans, or MRCP (magnetic resonance cholangiopancreatography). Blood tests may also be used to check for signs of infection or complications. - What treatments are available for gallstones?
Treatment options depend on the severity of the symptoms. Some people may benefit from medications that dissolve gallstones, but these are not always effective. In most cases, a surgical procedure called cholecystectomy (removal of the gallbladder) is the best option to prevent further issues. - Is surgery the only option for gallstones?
Surgery is the most common and effective treatment for symptomatic gallstones, especially if they cause pain or complications. However, in some cases, medications can be used to dissolve cholesterol-based stones, though this process is slow and not always successful. - What happens if gallstones are left untreated?
Untreated gallstones can lead to serious complications such as cholecystitis (gallbladder inflammation), pancreatitis (inflammation of the pancreas), bile duct obstruction, or gallbladder infections. These conditions can be life-threatening and usually require immediate medical attention. - Can I live without a gallbladder?
Yes, you can live without a gallbladder. After a cholecystectomy, bile flows directly from the liver into the small intestine, allowing digestion to continue without major issues. Some people may experience mild digestive changes, but most lead normal lives after the surgery. - How can I prevent gallstones?
You can reduce your risk of developing gallstones by maintaining a healthy weight, eating a balanced diet that is low in fat and high in fiber, staying hydrated, and avoiding rapid weight loss. Regular physical activity can also help in prevention.
These FAQs provide an overview of the essential facts about gallstones, from causes and symptoms to treatment and prevention options. If you suspect you have gallstones or experience any concerning symptoms, it is important to consult with a healthcare provider for appropriate diagnosis and management.