Summary
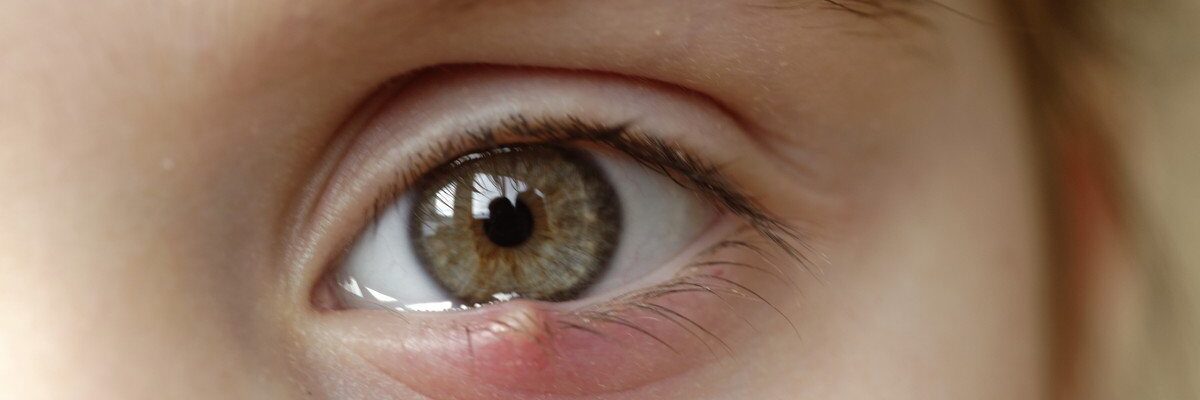
A stye, known medically as a hordeolum, is an infection of the eyelid caused by the Staphylococcus bacteria. This condition appears as a small bump or lump on the upper or lower eyelid, often filled with pus. Styes usually develop near the edge of the eyelid where the eyelashes grow but can also occur within the inner part of the eyelid.
Although a stye is not a serious condition, it can cause discomfort and pain. Common symptoms include swelling, redness, and tenderness in the affected eyelid. The eye may also feel irritated, itchy, and watery due to the infection and resulting inflammation.
Styes generally resolve on their own with basic hygiene and care, such as cleaning the eye area daily. Symptom relief methods include applying warm compresses to the eyelid, using antibiotic eye drops or ointment, and, in some cases, taking oral antibiotics for more persistent infections. For large styes with significant pus buildup, a doctor may perform a minor procedure to drain the stye, which can help relieve symptoms and speed healing.
Table of Contents
Symptoms of Stye
A stye can be identified by several noticeable symptoms and sensations. Here are common signs that someone may have a stye:
- Red, swollen bump on the eyelid. A stye typically appears as a red bump or boil on the edge of the eyelid, resembling a pimple or small abscess.
- Sensation of a lump in the eye. Individuals with a stye may feel as though there is a foreign object or lump in the eye, especially when blinking.
- Pain in the eyelid. The affected area can be tender or painful to the touch, as the stye puts pressure on the surrounding tissue.
- Swelling of the eyelid. In addition to the bump, there may be generalized swelling in the upper or lower eyelid, which can make the eye feel heavy or uncomfortable.
- Excessive tearing. The eye may water more than usual due to irritation from the infection.
- Crusting along the eyelid. As the stye progresses, a crust may form along the edge of the eyelid, particularly after sleep, as discharge from the infection dries.
- Itching of the eye. The infected area may feel itchy, especially if the surrounding tissue is inflamed.
These symptoms usually indicate a stye and can vary in intensity. While most styes resolve on their own with home care, persistent or severe symptoms may require medical attention for relief and to prevent complications.
Types of Stye
A stye, or hordeolum, comes in two primary forms: external stye and internal stye. Each type has distinct characteristics based on its location on the eyelid.
- External stye. Also known as an external hordeolum, this is the most common type of stye. In an external stye, the infection develops on the outer edge of the eyelid, usually at the base of an eyelash follicle. This form of stye often appears as a red, tender bump that is easily visible and may be filled with pus.
- Internal stye. Known as an internal hordeolum, this type of stye forms within the inner part of the eyelid. An internal stye affects the meibomian glands, which are oil-producing glands within the eyelid. Because it grows inward, the patient may feel a lump pressing against the eye, causing discomfort or a sensation of fullness inside the eyelid.
These types of styes differ primarily in location and sensation. External styes are often more visible and accessible for treatment, while internal styes may require additional care or medical attention due to their deeper location in the eyelid.
Diagnostic Procedures for Stye
Diagnosing a stye is generally straightforward and relies on a physical examination by a healthcare professional. In most cases, no specialized tests are necessary, but additional evaluation may be required if symptoms are severe or persistent. Here are common diagnostic steps for identifying a stye:
- Physical examination. A doctor will closely examine the affected eyelid, looking for redness, swelling, and the presence of a bump. They may gently touch the area to assess tenderness and check for signs of pus or infection.
- Evaluation of symptoms. The doctor will ask about symptoms, such as pain, itching, tearing, or any sensation of a lump in the eye, to help distinguish a stye from other conditions like a chalazion or blepharitis.
- Eyelid and eyelash inspection. Using a magnifying tool or bright light, the doctor may inspect the eyelid and eyelash follicles for any blocked or infected glands that could contribute to the stye.
- Assessment of underlying causes (if recurring). If styes are recurrent or chronic, the doctor may consider potential underlying causes, such as blepharitis, meibomian gland dysfunction, or other eye-related conditions, and may recommend additional tests or referrals to an eye specialist.
- Bacterial culture (rare cases). In cases where the stye does not respond to standard treatment or there are signs of a more severe infection, the doctor may take a sample from the stye for bacterial culture to identify the specific bacteria and determine the best antibiotic treatment.
These diagnostic steps are typically sufficient to confirm the presence of a stye and distinguish it from other eye conditions. For most individuals, a stye diagnosis is quick and simple, allowing for prompt treatment and symptom relief.
Complications of Untreated Stye
While most styes resolve on their own, untreated styes can occasionally lead to complications, particularly if the infection spreads or becomes chronic. Here are some potential complications of an untreated stye:
- Chalazion formation. An untreated stye can harden over time and turn into a chalazion—a painless, firm lump on the eyelid caused by a blocked oil gland. While less painful, a chalazion may still cause discomfort and may require medical treatment if it doesn’t go away on its own.
- Preseptal cellulitis. If the infection spreads beyond the stye, it can lead to preseptal cellulitis, an infection of the eyelid and surrounding skin. This condition can cause redness, swelling, and tenderness around the eye and may require oral antibiotics to prevent further spread.
- Recurrent styes. Failing to treat a stye properly can lead to recurrent styes, particularly if underlying causes like poor hygiene, blepharitis, or meibomian gland dysfunction are not addressed. Recurrent styes can become a chronic issue that affects the eyelid’s health and appearance.
- Vision interference. A large or persistent stye may press against the eye, leading to blurred vision or difficulty keeping the eye open due to discomfort and swelling.
- Scarring on the eyelid. In some cases, particularly if the stye becomes repeatedly inflamed or is not allowed to drain properly, scarring on the eyelid may occur, which can affect the smooth movement of the eyelid and may require surgical correction.
- Spread of infection. Although rare, an untreated stye can potentially lead to a more serious eye infection, especially if the individual frequently touches or squeezes the stye, introducing additional bacteria to the area.
Prompt treatment of a stye can help prevent these complications, allowing for quicker healing and reducing the risk of future infections or eye issues. For styes that persist, grow, or cause significant discomfort, it’s best to seek medical attention for proper management and to rule out other conditions.
Causes of Stye

A stye is caused by a bacterial infection in the eyelid, most commonly by Staphylococcus bacteria. When bacteria enter an eyelash follicle, they can trigger an infection that blocks the oil glands around the eyelid, leading to a bump filled with pus. This bump can form on either the outer or inner part of the eyelid. Bacteria can enter the eye and cause a stye through various ways, including:
- Rubbing the eyes with dirty hands. Touching the eyes without washing hands can transfer bacteria to the eyelid, leading to infection.
- Irritation from makeup. Eye makeup, especially if old or contaminated, can irritate the eyelid and introduce bacteria that may cause a stye.
- Wearing dry or unclean contact lenses. Contact lenses that haven’t been properly cleaned or have dried out can carry bacteria, increasing the risk of infection.
- Using dirty washcloths or towels on the face. Towels and washcloths that aren’t washed frequently can harbor bacteria, which can transfer to the eyes.
- Sharing personal items with someone who has a stye. Using items like towels, makeup tools, or pillows that have been in contact with someone who has a stye can spread bacteria, leading to infection.
While the bacteria that cause styes are not highly contagious, they can spread through contact with contaminated items. Objects such as towels, makeup tools, or pillowcases can carry bacteria, and touching them and then touching your eyes can increase the risk of developing a stye.
Some common myths claim that styes result from peeking or looking at things secretly, but there is no truth to this. Likewise, there is no evidence that chicken blood can cause a stye if it splashes into the eye. However, if any substance enters the eye and is not cleaned promptly, bacteria may enter and cause infection, potentially leading to a stye.
Prevention of Stye

If you’ve had a stye before, you are at a higher risk of developing one again. To help prevent future styes, consider following these steps:
- Wash hands thoroughly with soap and water before touching the eyes. Clean hands help prevent transferring bacteria to the eyelids, reducing the chance of infection.
- Clean the face regularly, paying special attention to the eyelids. When cleaning the eyelids, you can use a cotton swab dipped in warm, soapy water. Gently wipe along the eyelid margin to remove any oil, dirt, or bacteria that could clog the glands.
- Wash your face before bed, especially if wearing makeup. Be sure to remove all makeup, particularly eye makeup, to avoid clogging pores and irritating the eyelids. If you wear contact lenses, remove them before bed to prevent dryness and irritation.
- Avoid sharing personal items, like towels or face cloths, with others. Using personal items that others have used on their faces can transfer bacteria to your eyes and increase the risk of infection.
These steps can help lower the risk of recurring styes by keeping the eye area clean and reducing exposure to bacteria.
Risk Factors for Stye

Anyone can develop a stye, but certain groups are more susceptible due to specific habits or underlying conditions. People in the following categories have a higher likelihood of experiencing styes:
- Individuals who frequently touch their eyes without washing their hands. Touching the eyes with unwashed hands can introduce bacteria to the eyelids, increasing the risk of infection.
- Contact lens wearers. People who use contact lenses have a higher chance of styes if they don’t follow proper hygiene, as bacteria on the fingers or lenses can transfer to the eyelids.
- People who use eye makeup. Using makeup on the eyelids, especially if it’s expired or not removed at the end of the day, can clog the glands and introduce bacteria that lead to styes.
- Individuals with blepharitis. Blepharitis is a chronic condition characterized by inflamed and irritated eyelid edges, which can lead to blocked glands and increase the risk of styes.
- People with rosacea. Rosacea is a skin condition that causes facial redness and can also affect the eyes (ocular rosacea), leading to inflammation that increases the likelihood of developing styes.
Recognizing these risk factors can help individuals take preventive measures, such as maintaining good hygiene, following proper contact lens care, and removing eye makeup before bed.
Stye FAQs
Here are answers to some frequently asked questions about styes to help you understand this common eye condition and how to manage it effectively.
- What is a stye?
A stye, or hordeolum, is a red, swollen bump on the eyelid caused by a bacterial infection. It usually forms near the base of an eyelash or inside the eyelid and may resemble a small boil or pimple. - What causes a stye?
Styes are caused by a bacterial infection, typically from Staphylococcus bacteria. This infection clogs oil glands or hair follicles on the eyelid, leading to the formation of a swollen, often painful bump. - What are the symptoms of a stye?
Common symptoms include a red, swollen bump on the eyelid, pain or tenderness, excessive tearing, a feeling of a lump in the eye, and sometimes crusting around the eyelid. - Are styes contagious?
While the bacteria that cause styes can spread, styes themselves are not highly contagious. However, sharing personal items, such as towels or makeup, with someone who has a stye can increase the risk of bacterial transfer. - How can I treat a stye at home?
Home treatments include applying a warm compress to the affected area for 10–15 minutes several times a day to reduce pain and promote drainage. Avoid squeezing the stye, as this can worsen the infection. Over-the-counter pain relievers can help with discomfort. - When should I see a doctor for a stye?
See a doctor if the stye does not improve after a few days of home treatment, if it grows larger, or if it affects your vision. Persistent or painful styes may require prescription antibiotics or minor drainage by a healthcare professional. - Can a stye lead to complications?
While most styes resolve on their own, untreated styes can lead to complications such as a chalazion (a hardened lump), preseptal cellulitis (infection of the eyelid area), or even recurrent styes if hygiene habits aren’t improved. - How can I prevent styes?
Good hygiene is key to preventing styes. Wash your hands before touching your eyes, clean your face regularly, remove eye makeup before bed, and avoid sharing personal items like towels or makeup brushes. - Can I wear contact lenses if I have a stye?
It’s best to avoid wearing contact lenses until the stye heals, as they can irritate the eye and increase the risk of spreading bacteria. Switch to glasses temporarily for comfort and safety. - Is a stye the same as a chalazion?
No, a stye is caused by an infection, while a chalazion results from a blocked oil gland and is usually not painful. However, an untreated stye can sometimes turn into a chalazion if it hardens over time.