Summary
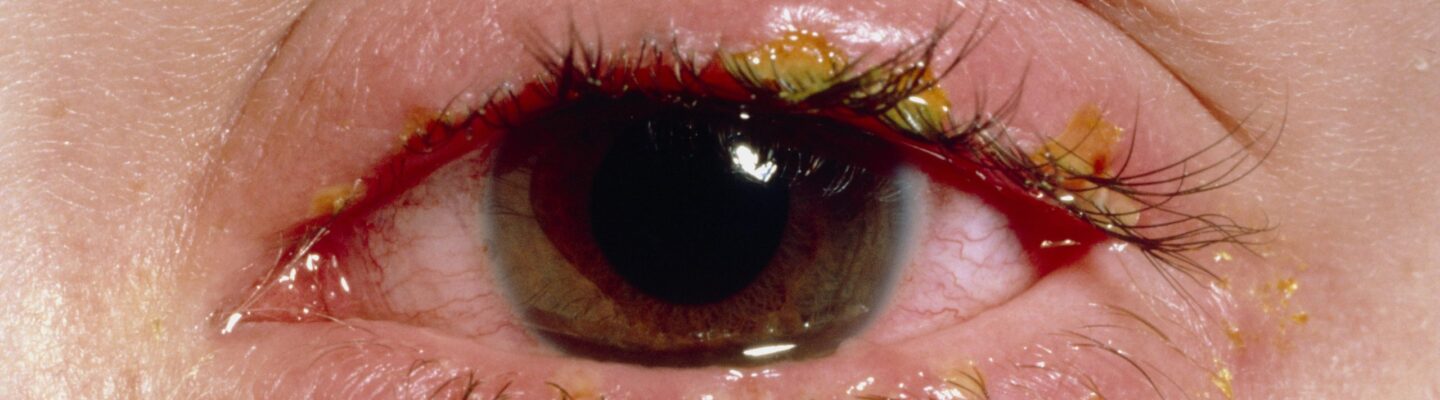
Blepharitis is an inflammation of the eyelids that occurs when the oil glands at the base of the eyelashes become irritated or blocked. This condition can result from bacterial overgrowth, mites, hormone imbalances, allergies, and other factors. Symptoms include red, itchy, and swollen eyelids, a sensation of something lodged under the eyelid, crustiness along the eyelashes, eye dryness, and occasional blurred vision.
Managing blepharitis often involves daily eyelid hygiene. Regularly cleaning the eyelids with a warm, damp cloth or gentle eyelid scrub can remove bacteria and debris that lead to irritation. Applying warm compresses also helps improve oil flow from the glands and soften crust along the lashes.
In some cases, doctors may prescribe steroid drops to reduce inflammation or antibiotic treatments for underlying bacterial infections. Since blepharitis is a chronic condition, consistent eye care and following medical advice are essential for controlling symptoms and preventing recurrence.
Table of Contents
Symptoms of Blepharitis

If a patient experiences the following symptoms, they may have blepharitis:
- Swelling of the eyelids. Eyelids appear puffy or inflamed.
- Redness of the eyelids. The eyelids take on a red or irritated appearance.
- Itching of the eyelids. Patients may feel an urge to scratch or rub their eyelids.
- Eye stinging or burning. Discomfort or a burning sensation is common.
- Excessive tearing or watery eyes. Eyes may produce more tears as a response to irritation.
- Sensation of a foreign body under the eyelids. Patients often feel as though something is stuck in their eye.
- Crusting of the eyelashes. A noticeable buildup of crust or flakes at the base of the lashes.
- Dryness of the eyes. Eyes may feel dry, gritty, or uncomfortable.
- Sensitivity to light. Patients may become more sensitive to bright lights.
- Blurred vision. Blurriness may occur temporarily, typically improving with treatment.
Not every patient will experience all of these symptoms, and blurred vision, if present, is usually temporary and improves once the condition is properly managed. Blepharitis symptoms can vary in intensity, but addressing them promptly can help relieve discomfort and prevent further complications.
Types of Blepharitis
Blepharitis is generally classified into two main types, based on the location of the inflammation:
- Anterior blepharitis. “Anterior” means “front,” so this type affects the front part of the eyelid where the eyelashes attach. Anterior blepharitis is often linked to bacteria or dandruff on the scalp and eyebrows, leading to inflammation at the eyelid edges.
- Posterior blepharitis. “Posterior” means “back,” indicating that the inflammation is located on the inner part of the eyelid, closer to the eye. This type is usually caused by issues with the meibomian glands, which produce oils that help keep the eyes lubricated. Blocked or irritated glands can lead to posterior blepharitis and often contribute to eye dryness and irritation.
Understanding the type of blepharitis is essential, as it helps guide treatment options to target the specific area of inflammation and underlying cause more effectively.
Diagnostic Procedures for Blepharitis
Diagnosing blepharitis is generally straightforward and often begins with a physical examination by an eye care professional. Here are some common procedures used to identify and confirm blepharitis:
- Visual examination. The eye doctor examines the eyelids, eyelashes, and eye surface under a light and magnification, looking for signs of inflammation, redness, crusting, and blocked oil glands that are characteristic of blepharitis.
- Slit-lamp examination. This test involves using a specialized microscope (slit-lamp) to closely examine the eye’s structures. The slit-lamp provides a magnified view of the eyelids, oil glands, and surrounding tissues, allowing the doctor to assess the extent of the inflammation.
- Tear film assessment. Because blepharitis can cause dry eyes, the doctor may test the stability and quality of the tear film on the eye’s surface. This helps determine if dry eye is a related factor in the patient’s condition.
- Eyelid culture or biopsy. In some cases, the doctor may collect a sample of the skin or oil from the eyelids to test for bacterial infection, fungi, or parasites, such as Demodex mites. This is generally done if symptoms are severe, recurrent, or unresponsive to initial treatments.
These diagnostic procedures help identify the presence and type of blepharitis, enabling the doctor to develop an effective treatment plan tailored to the specific cause and severity of the condition.
Complications of Untreated Blepharitis

If left untreated, blepharitis can lead to several complications that may affect eye health and comfort. Here are some common complications associated with untreated blepharitis:
- Chronic eye discomfort. Persistent irritation and inflammation can make the eyes feel gritty, itchy, or burning, impacting daily comfort and quality of life.
- Development of styes and chalazia. Blocked oil glands from blepharitis increase the risk of styes (painful, infected lumps on the eyelid) and chalazia (non-infected lumps caused by gland blockage). These lumps can cause pain, swelling, and in some cases, may require minor surgery.
- Dry eye syndrome. Untreated blepharitis can worsen dry eye symptoms due to dysfunction in the oil glands that help maintain a healthy tear film. This can lead to chronic dryness, discomfort, and even blurred vision.
- Damage to the cornea. Prolonged inflammation and irritation can lead to scratches or sores on the cornea (the eye’s outer layer), increasing the risk of corneal ulcers or scarring. Corneal damage can cause pain, sensitivity to light, and, in severe cases, vision impairment.
- Eyelash and eyelid changes. Chronic blepharitis can cause eyelashes to grow abnormally (misdirected eyelashes), fall out (eyelash loss), or become discolored. Long-term inflammation can also lead to thickening or scarring of the eyelids.
Proper treatment and management of blepharitis are essential to avoid these complications. Regular eye care and following a doctor’s treatment plan can help control symptoms, protect eye health, and prevent further complications.
Causes of Blepharitis
Blepharitis occurs when the oil glands in the eyelids become irritated or blocked, directly leading to inflammation. The following are the primary causes of blepharitis:
- Bacterial infection. Overgrowth of certain bacteria, particularly Staphylococcus species, on the eyelids is a common cause of blepharitis. When these bacteria increase in number, they can irritate the eyelids, leading to redness, swelling, and crusting around the eyelashes.
- Mite infestation. Tiny Demodex mites, which naturally live on human skin, can inhabit the eyelash follicles. In cases of overpopulation, these mites can trigger inflammation in the eyelids, contributing to blepharitis symptoms.
- Malfunctioning oil (meibomian) glands. The meibomian glands produce oils that help lubricate the eyes. When these glands become blocked or do not function properly, they fail to release adequate oils, leading to dryness and irritation in the eyelids. This condition, called meibomian gland dysfunction (MGD), is a primary cause of posterior blepharitis.
- Seborrheic dermatitis. Seborrheic dermatitis is a skin condition that results in flaky, inflamed skin, which can extend to the eyelids. This condition affects the natural balance of oils on the skin and contributes to inflammation and crusting on the eyelids.
- Viral infections. Certain viruses, such as herpes simplex virus, can directly infect the eyelid tissue and lead to inflammation. This type of viral infection can produce blepharitis-like symptoms, including eyelid swelling and discomfort.
Addressing these direct causes is essential for effectively managing blepharitis. Proper diagnosis and targeted treatment can help relieve symptoms and control underlying factors contributing to inflammation.
Prevention of Blepharitis

Maintaining good hygiene and healthy habits can help prevent irritation and inflammation in the eyelids, reducing the risk of blepharitis. Here are recommended precautions:
- Keep the face clean. To remove any bacteria or debris, wash the face regularly, especially before bed. Remove all makeup with gentle soap and water to prevent eye irritation.
- Avoid touching the eyes with dirty hands. Touching the eyes with unwashed hands can introduce bacteria and cause infection. Always wash hands thoroughly with soap and water before touching the eye area. If washing facilities aren’t available, use a hand sanitizer.
- Prevent dryness in the eyes. Dry eyes can worsen irritation and lead to inflammation. Use moisturizing eye drops to keep eyes lubricated and prevent dryness.
- Consume foods rich in omega-3 fatty acids. Omega-3s help reduce inflammation in the body, including the eyes. Foods high in omega-3, such as salmon, tuna, sardines, and other seafood, can be beneficial in maintaining eye health.
- Manage oily skin. Excess oil on the face can contribute to blocked glands in the eyelids. Use a gentle facial cleanser to reduce oiliness, and consider using powder to reduce excess shine and prevent sweat and oil buildup.
Practicing these preventive measures can help keep the eyelids healthy and reduce the risk of developing blepharitis. Regular hygiene and a balanced diet support eye health and prevent the irritation that can lead to inflammation.
Risk Factors for Blepharitis
While anyone can develop blepharitis, certain factors can increase the likelihood of this condition:
- Advancing age. People over the age of 50 have a higher risk of developing blepharitis. At this age, eyes often become drier, which can lead to irritation and inflammation of the eyelids.
- Oily skin. Individuals with oily skin are more prone to blepharitis, as excess oil on the face can create a favorable environment for bacteria and mites to multiply around the eyelids.
- Dry eyes. Chronic dryness in the eyes can lead to irritation, which increases the risk of inflammation in the eyelids, contributing to blepharitis symptoms.
- Skin conditions. Skin disorders like seborrheic dermatitis can affect the eyelids, causing flakiness, irritation, and inflammation, especially when the entire face is involved.
Understanding these risk factors can help individuals take preventive steps and manage symptoms early, reducing the likelihood of blepharitis flare-ups.
Blepharitis FAQs
Here are some frequently asked questions about blepharitis to help you understand the condition, its causes, and ways to manage it effectively.
- What is blepharitis?
Blepharitis is inflammation of the eyelids, usually caused by blocked or irritated oil glands at the base of the eyelashes. It can result in redness, swelling, and irritation of the eyelids. - What causes blepharitis?
Blepharitis can be caused by bacterial infections, excess oil production, skin conditions like seborrheic dermatitis, or parasitic mites such as Demodex that live in eyelash follicles. These factors can irritate or block the oil glands, leading to inflammation. - Is blepharitis contagious?
No, blepharitis is not contagious. It is typically caused by factors that are unique to an individual, such as bacteria or mites on their skin, oil gland dysfunction, or skin conditions. - What are the symptoms of blepharitis?
Common symptoms include red, swollen eyelids; itchy or burning eyes; crusting on the eyelashes; sensitivity to light; excessive tearing or dry eyes; and a sensation of something in the eye. - Can blepharitis cause vision problems?
While blepharitis itself doesn’t directly affect vision, symptoms like dryness, irritation, or corneal damage from severe cases can lead to blurred vision. Vision typically improves once the inflammation is managed. - How is blepharitis treated?
Treatment often includes warm compresses, gentle eyelid cleaning, lubricating eye drops, and in some cases, prescription medications like antibiotics or anti-inflammatory eye drops. Regular eye hygiene is crucial for managing symptoms. - Is blepharitis curable?
Blepharitis is usually a chronic condition, meaning it can’t be fully cured, but it can be managed effectively with proper care. Regular eyelid hygiene and following a treatment plan can help control symptoms and reduce flare-ups. - Can blepharitis lead to complications?
Yes, untreated blepharitis can cause complications such as styes, chalazia, dry eye syndrome, corneal damage, and changes in eyelash growth or eyelid appearance. Early treatment helps minimize these risks. - Who is at risk of developing blepharitis?
Factors that increase the risk include advancing age, oily skin, dry eyes, certain skin conditions (like rosacea or seborrheic dermatitis), and poor eyelid hygiene. - How can I prevent blepharitis?
Good eyelid hygiene, such as washing the eyelids daily, removing makeup before bed, and avoiding touching the eyes with dirty hands, can help prevent blepharitis. Consuming foods rich in omega-3 fatty acids may also reduce inflammation, supporting eye health.