Summary
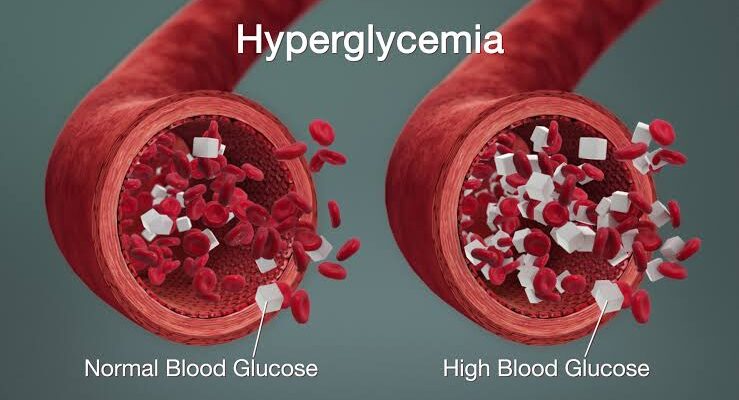
Hyperglycemia, or high blood sugar, occurs when glucose levels in the blood exceed normal ranges. While it’s a primary symptom of diabetes, hyperglycemia can also be triggered by other conditions like pancreatitis, pancreatic cancer, and Cushing’s syndrome. Symptoms typically include frequent urination, excessive thirst, dry mouth, fatigue, unexplained weight loss, slow-healing wounds, blurred vision, and dry or itchy skin. Blood sugar levels above 200 mg/dL are generally considered hyperglycemic.
Common causes of hyperglycemia include overeating (especially carbohydrates), high stress levels, lack of physical activity, certain medications (like steroids), and poor diabetes management. Infections, injuries, and surgeries may also elevate blood sugar due to the body’s stress response. Even non-diabetics can experience spikes due to these factors.
Management of hyperglycemia usually involves lifestyle changes, such as a balanced diet low in refined sugars, regular exercise, and staying hydrated. In severe cases, insulin or other medications may be necessary to restore normal levels. Consulting with a healthcare provider is essential to create a tailored plan for maintaining stable blood sugar levels.
Table of Contents
Symptoms of Hyperglycemia

When a person experiences hyperglycemia, they may show several common symptoms due to elevated blood sugar levels. Early signs include:
- Frequent urination, especially at night. This occurs as the kidneys attempt to filter excess glucose from the blood.
- Persistent thirst. High blood sugar causes dehydration, leading to a constant feeling of thirst.
- Dry mouth. Dehydration from excessive urination can lead to a dry, uncomfortable mouth.
- Frequent drowsiness. Elevated blood sugar can make a person feel unusually sleepy or sluggish.
- Quick fatigue. Low energy levels are common, as the body struggles to use glucose efficiently.
- Unexplained weight loss despite eating. Without insulin, the body cannot access glucose, leading it to break down fat and muscle.
- Slow wound healing. High blood sugar impairs circulation and immune function, slowing healing.
- Blurry vision. Excess sugar can cause swelling in the eyes, leading to visual disturbances.
- Dry and itchy skin. High glucose can dehydrate the skin and lead to irritation.
- Blood sugar levels above 200 mg/dL. This measurement generally indicates hyperglycemia.
These symptoms highlight the importance of recognizing early signs of hyperglycemia and seeking prompt medical care to prevent complications.
Types of Hyperglycemia
Hyperglycemia has two primary types: fasting hyperglycemia and postprandial (or after-meal) hyperglycemia. These types indicate when elevated blood sugar occurs relative to meals and fasting periods.
- Fasting Hyperglycemia. This type occurs when blood sugar levels exceed 130 mg/dL after fasting for at least 8 hours, meaning the individual has not eaten or consumed caloric beverages during this period. Persistent fasting hyperglycemia may signal an issue with insulin production or effectiveness and can be an indicator of diabetes or other metabolic conditions.
- Postprandial Hyperglycemia. Known as after-meal hyperglycemia, this type occurs when blood sugar levels rise above 180 mg/dL within two hours after eating. In people without diabetes, blood sugar levels typically stay below 140 mg/dL after meals. Postprandial hyperglycemia can result from insulin resistance, insufficient insulin, or consuming large quantities of high-carbohydrate foods.
Both types of hyperglycemia are important to monitor, as they can lead to complications if unmanaged, and may indicate the need for lifestyle or medication adjustments.
Diagnostic Procedures for Hyperglycemia
Diagnosing hyperglycemia involves several tests to measure blood sugar levels accurately and assess how the body processes glucose. Here are the primary diagnostic procedures for hyperglycemia:
- Fasting Plasma Glucose (FPG) Test. This test measures blood glucose levels after an 8-hour fast. A reading above 126 mg/dL indicates hyperglycemia and may be suggestive of diabetes. This test is often used as a first step in diagnosing high blood sugar.
- Oral Glucose Tolerance Test (OGTT). Primarily used to diagnose gestational diabetes, this test involves fasting, followed by drinking a glucose solution and measuring blood sugar at intervals over two hours. A blood glucose level over 200 mg/dL two hours after consuming the solution confirms hyperglycemia.
- Random Plasma Glucose Test. This test measures blood glucose at any time of the day, without fasting. A reading above 200 mg/dL, especially if accompanied by symptoms of hyperglycemia, may indicate diabetes or uncontrolled blood sugar levels.
- Hemoglobin A1c Test (HbA1c). This test provides an average blood glucose level over the past two to three months by measuring the percentage of glucose attached to hemoglobin in the blood. An HbA1c level of 6.5% or higher indicates poor blood sugar control and potential hyperglycemia.
- Continuous Glucose Monitoring (CGM). A CGM device measures blood sugar levels throughout the day and night, providing real-time glucose data and trends. This test is especially useful for people with diabetes to monitor for episodes of hyperglycemia and adjust their treatment as needed.
These diagnostic procedures help doctors accurately determine blood sugar levels, assess the risk of complications, and create an effective treatment plan.
Complications of Untreated Hyperglycemia
If hyperglycemia is left untreated, it can lead to a variety of serious health complications, particularly in individuals with diabetes. Persistent high blood sugar levels damage blood vessels and organs over time, increasing the risk of several conditions:
- Diabetic Ketoacidosis (DKA). This acute complication primarily affects people with type 1 diabetes. When the body cannot use glucose for energy due to a lack of insulin, it breaks down fats instead, producing acidic ketones. Accumulation of ketones in the blood can lead to DKA, a life-threatening condition characterized by severe dehydration, vomiting, abdominal pain, and altered mental status.
- Hyperosmolar Hyperglycemic State (HHS). This condition is common in individuals with type 2 diabetes and occurs when blood sugar levels become extremely high, leading to severe dehydration and electrolyte imbalances. HHS can result in confusion, seizures, and even coma if not treated promptly.
- Cardiovascular disease. Chronic hyperglycemia damages blood vessels, increasing the risk of atherosclerosis (hardening of the arteries), high blood pressure, heart attacks, and strokes. People with untreated hyperglycemia are at a significantly higher risk for these cardiovascular complications.
- Kidney damage (diabetic nephropathy). High blood sugar can damage the kidneys’ delicate filtering system, leading to kidney disease or even kidney failure. Diabetic nephropathy is one of the leading causes of end-stage renal disease, requiring dialysis or kidney transplant.
- Nerve damage (diabetic neuropathy). Persistent high blood sugar damages nerves, leading to diabetic neuropathy, which can cause pain, tingling, numbness, and weakness, especially in the hands and feet. Severe nerve damage can lead to mobility issues and increase the risk of injuries and infections.
- Vision problems (diabetic retinopathy). High blood sugar can damage the blood vessels in the retina, leading to diabetic retinopathy, a major cause of blindness in adults. Additional complications may include glaucoma and cataracts.
- Foot ulcers and infections. Nerve damage and poor circulation from hyperglycemia increase the risk of developing foot ulcers and infections, which can become severe and may require amputation if not managed properly.
- Skin infections and conditions. High blood sugar weakens the immune system, making the skin more susceptible to infections and slow wound healing. Conditions like bacterial and fungal infections are more common in individuals with untreated hyperglycemia.
- Cognitive decline. Chronic hyperglycemia is linked to an increased risk of cognitive impairment and may contribute to dementia, including Alzheimer’s disease, due to its damaging effects on brain blood vessels and nerve cells.
The complications associated with untreated hyperglycemia underscore the importance of monitoring and managing blood sugar levels. Prompt diagnosis and treatment can help prevent or delay these potentially life-altering conditions.
Causes of Hyperglycemia

Hyperglycemia, or high blood sugar, occurs due to specific physiological disruptions that prevent the body from properly regulating glucose. Here are the primary direct causes:
- Insufficient insulin production. The pancreas may not produce enough insulin, a hormone crucial for lowering blood sugar. This lack of insulin occurs most commonly in type 1 diabetes due to autoimmune destruction of pancreatic beta cells. Without adequate insulin, glucose cannot effectively enter cells, causing it to accumulate in the bloodstream.
- Insulin resistance. In type 2 diabetes and certain other conditions, the body becomes resistant to insulin, meaning cells do not respond to it effectively. This resistance forces the pancreas to produce more insulin, but when it can’t keep up, blood sugar levels rise. Insulin resistance is often the result of genetic factors, and it directly disrupts glucose regulation.
- Excess glucose production by the liver. The liver plays a key role in maintaining blood sugar levels by producing glucose, especially during fasting. However, in some conditions, such as type 2 diabetes, the liver may produce too much glucose due to hormonal imbalances, contributing to elevated blood sugar levels.
- Excessive carbohydrate intake without matching insulin response. High carbohydrate intake can directly cause spikes in blood sugar, especially if the body cannot produce or respond to insulin adequately. This can occur in people with diabetes who are not taking sufficient insulin or other medications to counteract the glucose load.
- Hormonal imbalances. Certain hormones, like cortisol and adrenaline, increase blood sugar levels as part of the body’s response to stress. Conditions that lead to excessive production of these hormones, such as Cushing’s syndrome (excess cortisol), can directly elevate blood sugar.
- Acute physical stress from illness or injury. Severe illness or physical trauma, including infections and injuries, prompt the body to release stress hormones that increase blood sugar levels. This response provides energy to cells for repair and recovery but can lead to hyperglycemia, especially if insulin production or function is impaired.
These direct causes lead to hyperglycemia by disrupting the body’s natural mechanisms for regulating glucose, either through inadequate insulin, excess glucose production, or hormonal triggers that increase blood sugar. Addressing these direct factors is essential for effective blood sugar management.
Prevention of Hyperglycemia

To prevent hyperglycemia, certain precautions can help maintain stable blood sugar levels and promote overall health:
- Eat balanced, nutritious meals. Focus on balanced portions and limit intake of sugary and fatty foods. A diet rich in vegetables, lean proteins, and whole grains helps regulate blood sugar levels.
- Exercise for at least 30 minutes daily. Physical activity supports a healthy weight and enhances the body’s use of insulin, making it easier to control blood sugar.
- Avoid stress as much as possible. Stress releases hormones that can raise blood sugar levels. Engaging in relaxation techniques or activities you enjoy can help manage stress effectively.
- Maintain good health to avoid infections and illnesses. Keeping your immune system strong and avoiding common infections like colds and flu can prevent spikes in blood sugar related to illness.
- Drink plenty of water. Staying hydrated helps the body flush out excess sugar through urination, assisting in blood sugar regulation.
Hyperglycemia is generally manageable when addressed early. However, if ignored, it can lead to severe complications, such as diabetic ketoacidosis (DKA), a life-threatening condition. In DKA, the body starts breaking down fats for energy instead of glucose, producing acidic ketones that can accumulate in the blood, leading to potential toxicity and danger to the patient’s life. Prevention through these measures can help avoid such serious outcomes.
Risk Factors for Hyperglycemia

Hyperglycemia can potentially affect anyone, but certain factors may increase the likelihood of developing this condition:
- Age. As people get older, they may be less active, which can impact insulin sensitivity. The body becomes less efficient at using insulin with age, raising the risk of hyperglycemia.
- Family history of hyperglycemia. Individuals with a family history of hyperglycemia or diabetes are at higher risk. Genetics can play a role in both insulin resistance and the body’s ability to produce insulin effectively.
- Unhealthy lifestyle. Being overweight, smoking, having high blood pressure, or avoiding physical activity can increase the risk of hyperglycemia. These lifestyle factors put extra strain on the pancreas, which produces insulin, and may contribute to insulin resistance over time.
- Pregnancy. During pregnancy, a woman’s body undergoes significant hormonal changes. Sometimes, these changes lead to reduced insulin production by the pancreas, increasing the risk of hyperglycemia. This is often seen in cases of gestational diabetes, where high blood sugar can affect both mother and baby.
Recognizing these risk factors can help individuals take preventive measures to maintain stable blood sugar levels, especially those with a family history or other predisposing conditions.
Hyperglycemia FAQs
Hyperglycemia, or high blood sugar, is a condition that can affect anyone and understanding its causes, symptoms, and management is key to maintaining optimal health.
- What is hyperglycemia?
Hyperglycemia, commonly referred to as high blood sugar, is a condition where there is too much glucose in the bloodstream. It can occur due to insufficient insulin, insulin resistance, or excessive glucose production by the liver. While it’s often associated with diabetes, other conditions and lifestyle factors can lead to hyperglycemia. - What are the common symptoms of hyperglycemia?
Common symptoms include frequent urination (especially at night), increased thirst, dry mouth, fatigue, blurred vision, slow-healing wounds, and unexplained weight loss. In severe cases, it may lead to symptoms like confusion, abdominal pain, dizziness, and shortness of breath. - What causes hyperglycemia?
Hyperglycemia can be caused by a lack of insulin, insulin resistance, high carbohydrate intake, hormonal imbalances, and certain illnesses or stress. For individuals with diabetes, hyperglycemia can result from missed doses of insulin or blood sugar-lowering medications, insufficient exercise, or high stress levels. - How is hyperglycemia different from hypoglycemia?
Hyperglycemia refers to high blood sugar levels, while hypoglycemia refers to low blood sugar levels. Both conditions are related to glucose balance in the blood, but they have opposite effects and symptoms. Hypoglycemia can cause symptoms like shakiness, sweating, and confusion, and may lead to loss of consciousness if severe. - How can hyperglycemia be prevented?
Prevention strategies include eating a balanced diet low in refined sugars, exercising regularly, managing stress, staying hydrated, and maintaining a healthy weight. For those with diabetes, taking medications or insulin as prescribed and monitoring blood sugar levels frequently are crucial. - What is the difference between fasting and postprandial hyperglycemia?
Fasting hyperglycemia occurs when blood sugar levels exceed 130 mg/dL after an 8-hour fast. Postprandial (after-meal) hyperglycemia happens when blood sugar levels are above 180 mg/dL within two hours after eating. Monitoring both can help in managing blood sugar effectively. - Can hyperglycemia be dangerous if left untreated?
Yes, untreated hyperglycemia can lead to serious complications like diabetic ketoacidosis (DKA) in type 1 diabetes or hyperosmolar hyperglycemic state (HHS) in type 2 diabetes. Both conditions are medical emergencies that can result in coma or death if not promptly treated. - How is hyperglycemia treated?
Treatment depends on the severity. Mild cases may be managed through lifestyle changes like diet and exercise. Severe cases may require insulin or other medications to lower blood sugar. It’s important to consult a healthcare provider to determine the appropriate treatment plan. - Does hyperglycemia only affect people with diabetes?
No, while hyperglycemia is commonly associated with diabetes, it can also occur in people without diabetes due to factors like high stress, illness, certain medications, or hormonal imbalances. - When should I see a doctor about hyperglycemia?
If you experience persistent symptoms of hyperglycemia or if your blood sugar levels are consistently above target, it’s essential to consult a healthcare provider. Immediate medical attention is necessary if you experience symptoms like severe dehydration, confusion, difficulty breathing, or abdominal pain.