Summary
Graves’ disease is a condition affecting the thyroid gland. Named after the Irish physician Robert James Graves, who was one of the first to observe it, the disease is also known as Basedow’s disease, after German physician Karl Adolph von Basedow, who independently described the condition in 1840.
Graves’ disease is an autoimmune disorder that causes the thyroid gland to produce an excessive amount of thyroid hormone, leading to hyperthyroidism. While the exact cause is still unknown, the condition results from an overactive thyroid gland. Why this overactivity occurs remains a mystery to doctors.
Common symptoms of Graves’ disease include bulging eyes, thickened skin in certain areas, anxiety, rapid heart rate, and sensitivity to heat. Treatments for Graves’ disease may involve medications to reduce thyroid activity, radioiodine therapy, or surgery to remove part or all of the thyroid gland.
Table of Contents
Symptoms of Graves’ Disease

Diagnosing Graves’ disease can be challenging, as its symptoms often resemble those of other conditions. However, some common symptoms associated with Graves’ disease include:
- Unexplained Weight Loss. Despite having a healthy appetite, individuals may experience weight loss.
- Anxiety and Tremors. Shakiness and heightened nervousness are frequent symptoms.
- Irritability. Individuals may become more easily agitated.
- Difficulty Sleeping. Insomnia is common due to heightened metabolism and nervousness.
- Sensitivity to Heat. Increased intolerance to warm temperatures can occur.
- Excessive Sweating. Profuse sweating is often a sign of overactive thyroid function.
- Chest Pain. Some may experience discomfort or pain in the chest.
- Rapid Heartbeat. Tachycardia, or a fast pulse, is a typical symptom.
- Shortness of Breath. This can result from the heart working harder than usual.
- Frequent Bowel Movements. Increased activity in the digestive system may lead to frequent bowel movements, though typically not diarrhea.
- Irregular Menstrual Cycles. Women may experience changes in their menstrual patterns.
- Muscle Weakness. Fatigue and weakened muscles are common.
- Difficulty Managing Diabetes. Blood sugar may be harder to control in those with diabetes.
- Goiter. Enlargement of the thyroid gland, visible as a swelling at the base of the neck.
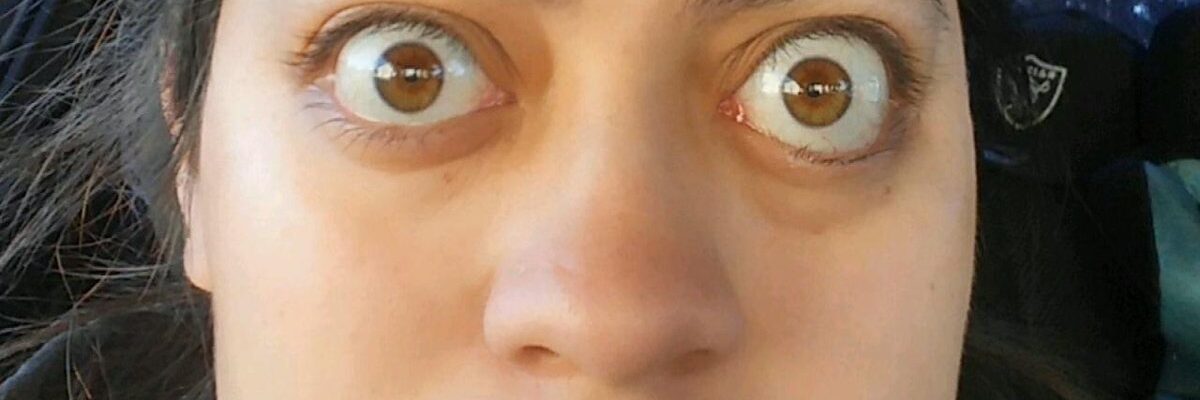
- Bulging Eyes (Exophthalmos). Eyes may appear larger or protrude due to thyroid eye disease.
- Double Vision and Vision Issues. Graves’ disease can affect eye alignment and cause other visual disturbances.
- Thickening of the Skin. Some individuals may experience skin changes, often on the shins and feet.
Additional autoimmune conditions are sometimes linked to Graves’ disease, which may cause symptoms like:
- Turner Syndrome (though rare)
- Celiac Disease
- Pterygium (growth of tissue on the eye)
- Dystonia (muscle contractions causing repetitive movements)
- Cushing Syndrome
- Anal Fissure (tear in the lining of the anus)
- Acid Reflux or Heartburn
While some of these are less common, they may appear in association with Graves’ disease or as complications from autoimmune dysfunction. Recognizing these symptoms and seeking medical attention can aid in early diagnosis and appropriate treatment.
Types of Graves’ Diseases
Graves’ disease can present in different forms, each affecting various parts of the body. Here are some recognized subtypes:
- Graves’ Dermopathy. Also known as localized myxedema or thyroid dermopathy, this rare manifestation of autoimmune thyroiditis in Graves’ disease primarily affects the skin. The main symptom is the thickening of the skin, usually on the shins and feet, where it appears red, swollen, and firm.
- Graves’ Orbitopathy. This form of Graves’ disease impacts the retroocular tissues (tissues behind the eyes) and is an autoimmune condition affecting individuals with Graves’ disease. It is often called Graves’ ophthalmopathy; however, “Graves’ orbitopathy” more accurately describes this condition, which involves inflammation and immune response in the eye area.
- Graves’ Ophthalmopathy (Thyroid Eye Disease or TED). Known as thyroid eye disease, this autoimmune inflammatory disorder affects the orbit (eye socket) and surrounding tissues. It is characterized by upper eyelid retraction, eye swelling, redness, conjunctivitis, and bulging eyes (proptosis or exophthalmos). TED can range from mild eye discomfort to more severe symptoms affecting vision.
These subtypes reflect the diverse ways Graves’ disease can affect the body beyond just thyroid overactivity.
Diagnostic Procedures for Graves’ Disease
Diagnosing Graves’ disease involves several tests to confirm hyperthyroidism and identify the autoimmune cause. Here are the primary diagnostic procedures:
- Physical Examination. A doctor will check for physical signs of Graves’ disease, such as an enlarged thyroid gland (goiter), rapid pulse, tremors, and symptoms of thyroid eye disease like bulging eyes.
- Blood Tests. You may be asked to take a blood test for your doctor to get readings on the following:
- Thyroid Hormone Levels (T3 and T4): Elevated levels of these hormones indicate an overactive thyroid.
- Thyroid-Stimulating Hormone (TSH): TSH levels are typically low in Graves’ disease because excess thyroid hormone suppresses TSH production by the pituitary gland.
- Thyroid-Stimulating Immunoglobulins (TSI): Testing for these specific antibodies helps confirm Graves’ disease as they stimulate the thyroid gland to produce more hormones.
- Radioactive Iodine Uptake (RAIU) Test. This test measures how much iodine the thyroid gland absorbs from the bloodstream. In Graves’ disease, iodine uptake is typically higher due to the gland’s hyperactivity. The patient ingests a small amount of radioactive iodine, and after a set period, thyroid uptake is measured with a special scanner.
- Thyroid Scan. Often done in conjunction with the RAIU test, a thyroid scan provides an image of the thyroid gland, showing areas of increased activity, which is common in Graves’ disease. This helps to rule out other potential causes of hyperthyroidism, such as thyroid nodules.
- Ultrasound. An ultrasound may be used to examine the size and structure of the thyroid gland. This is particularly useful if there is a noticeable goiter or if a physical exam raises concerns about nodules.
- Ophthalmologic Examination. If Graves’ ophthalmopathy (thyroid eye disease) is suspected, an eye exam may be performed to assess symptoms like bulging eyes, redness, swelling, or vision problems.
These diagnostic procedures provide a comprehensive assessment of thyroid function and help confirm whether Graves’ disease is the cause of hyperthyroidism. Early and accurate diagnosis is essential for managing symptoms and reducing complications.
Complications of Untreated Graves’ Disease
If left untreated, Graves’ disease can lead to a variety of serious complications due to prolonged thyroid hormone overproduction. Here are some potential complications:
- Heart Disorders. Excess thyroid hormone increases heart rate and blood pressure, which can lead to arrhythmias (irregular heartbeat), heart palpitations, and congestive heart failure. Persistent high heart rate and hypertension also put extra strain on the cardiovascular system.
- Osteoporosis. High thyroid hormone levels interfere with the body’s ability to incorporate calcium into the bones, resulting in decreased bone density. Over time, this can lead to osteoporosis, increasing the risk of fractures.
- Thyroid Storm. A rare but life-threatening complication, thyroid storm is a sudden and severe increase in thyroid hormone levels. It can cause extreme symptoms like high fever, rapid heartbeat, confusion, and dehydration, requiring immediate medical intervention.
- Graves’ Ophthalmopathy (Thyroid Eye Disease). If untreated, Graves’ disease can worsen thyroid eye disease, leading to bulging eyes, double vision, eye pain, and in severe cases, vision loss. Eye complications may become irreversible if not addressed early.
- Mental Health Issues. Chronic untreated Graves’ disease can lead to mood swings, anxiety, and depression due to hormonal imbalance. Severe cases can even result in more significant mental health issues, impacting daily functioning.
- Skin Disorders (Graves’ Dermopathy). In rare cases, Graves’ disease can cause Graves’ dermopathy, leading to thickened, red skin, usually on the shins or tops of the feet.
- Reproductive Issues. Untreated Graves’ disease can disrupt menstrual cycles in women, leading to irregular periods and reduced fertility. During pregnancy, untreated hyperthyroidism can increase the risk of miscarriage, premature birth, and low birth weight.
- Unintentional Weight Loss and Muscle Weakness. Persistent high metabolism can result in significant, unintended weight loss and muscle wasting, leading to fatigue, weakness, and reduced physical endurance.
- Increased Risk of Other Autoimmune Disorders. Prolonged immune system dysfunction may make individuals more susceptible to developing other autoimmune conditions, such as type 1 diabetes, rheumatoid arthritis, or vitiligo.
Treating Graves’ disease promptly is essential to prevent these complications and maintain overall health. Proper management can significantly reduce the risks associated with the condition.
Causes of Graves’ Disease
Graves’ disease results from a malfunction in the immune system, though the precise reasons why this occurs remain under study.
One of the immune system’s key roles is to produce antibodies, which target and destroy harmful invaders like viruses and bacteria. The thyroid gland, located in the neck, plays a role in this process by producing antibodies and managing various bodily functions through the release of thyroid hormones.
In Graves’ disease, however, the immune system mistakenly triggers the thyroid to produce an excessive amount of thyroid hormones, leading to hyperthyroidism and further disrupting immune function. This immune response causes the thyroid gland to become overactive, resulting in various symptoms associated with Graves’ disease.
Researchers believe that genetic predisposition and environmental factors may play a role in the onset of Graves’ disease, though much is still being investigated.
Prevention of Graves’ Disease

While the exact cause of Graves’ disease remains unclear, genetics play a significant role in its development. For individuals with a family history of Graves’ disease, adopting a healthy lifestyle may help reduce the risk of triggering the condition. Here are some recommended preventive measures:
- Avoid Smoking. Smoking is known to increase the risk of developing Graves’ disease and can exacerbate symptoms, particularly those related to eye health.
- Engage in Regular Exercise. Consistent physical activity supports overall health and can help regulate immune function.
- Manage Stress Levels. Practicing stress-reducing activities, such as meditation, deep breathing exercises, or hobbies, can help minimize triggers that may exacerbate autoimmune responses.
Adopting these lifestyle practices can promote general health and may help lower the risk of autoimmune conditions like Graves’ disease, especially for those with a family predisposition.
Risk Factors for Graves’ Disease

The following factors can increase the risk of developing Graves’ disease:
- Family History. Graves’ disease is known to run in families, suggesting a genetic component that predisposes individuals to the condition.
- Gender. Women are more likely to develop Graves’ disease than men.
- Age. Studies show that Graves’ disease commonly affects individuals under the age of 40.
- Existing Autoimmune Conditions. People with other autoimmune disorders, such as type 1 diabetes or rheumatoid arthritis, are at higher risk of developing Graves’ disease.
- Emotional and Physical Stress. Stressful events can trigger the onset of Graves’ disease, especially in individuals with a family history of the condition.
- Pregnancy and Postpartum Period. Pregnancy and childbirth can increase the risk of Graves’ disease, particularly for women with a family history of the condition.
- Smoking. Smoking can compromise the immune system and increase susceptibility to autoimmune diseases, including Graves’ disease. It also heightens the risk of Graves’ ophthalmopathy (eye involvement).
Understanding these risk factors can help in early detection and intervention, reducing the likelihood of complications associated with Graves’ disease.
Graves’ Disease FAQs
Here are answers to some frequently asked questions about Graves’ disease:
- What is Graves’ disease?
Graves’ disease is an autoimmune disorder that causes the thyroid gland to produce excessive amounts of thyroid hormone, leading to hyperthyroidism. This can impact metabolism, energy levels, and various bodily functions. - What causes Graves’ disease?
The exact cause is unknown, but Graves’ disease occurs when the immune system mistakenly attacks the thyroid, stimulating it to produce more hormones. Genetic predisposition and environmental factors, such as stress and smoking, are thought to play a role. - What are the common symptoms of Graves’ disease?
Symptoms include rapid heartbeat, weight loss, anxiety, increased sweating, bulging eyes, and enlarged thyroid (goiter). Other symptoms may include muscle weakness, sleep disturbances, and sensitivity to heat. - Is Graves’ disease the same as hyperthyroidism?
No, but Graves’ disease is the most common cause of hyperthyroidism. Hyperthyroidism refers to any condition that causes excess thyroid hormone, while Graves’ disease specifically involves an autoimmune trigger. - How is Graves’ disease diagnosed?
Diagnosis includes a physical exam, blood tests to check thyroid hormone and antibody levels, and imaging tests, such as a radioactive iodine uptake scan, to assess thyroid function. - Can Graves’ disease affect the eyes?
Yes, Graves’ disease can lead to Graves’ ophthalmopathy, or thyroid eye disease (TED), which causes bulging eyes, double vision, eye dryness, and redness. - Is Graves’ disease curable?
Graves’ disease can be managed effectively, though it is typically a lifelong condition. Treatment options—such as medication, radioactive iodine therapy, and surgery—help control symptoms but don’t fully cure the autoimmune aspect. - What are the treatment options for Graves’ disease?
Treatment includes antithyroid medications to reduce hormone production, radioactive iodine to shrink the thyroid, and surgery to remove part or all of the thyroid gland in severe cases. - Can lifestyle changes help manage Graves’ disease?
Yes, lifestyle changes like avoiding smoking, managing stress, and eating a balanced diet can support treatment and help reduce symptoms. - Is Graves’ disease genetic?
Genetics can increase susceptibility, and having a family history of autoimmune conditions may raise the risk of developing Graves’ disease.
These FAQs provide an overview of Graves’ disease, covering its causes, symptoms, diagnosis, treatment, and management tips.