Summary
An ear infection is a condition that can affect people of all ages. Although usually not severe, untreated ear infections can lead to complications. Ear infections have been common for centuries, but the invention of the otoscope in the 19th century significantly advanced our understanding by allowing doctors to examine the ear canal and eardrum directly.
There are various types of ear infections, including otitis externa (outer ear canal infection), otitis media (middle ear infection), and otitis interna (inner ear infection), among others. These infections can result from viruses, bacteria, or fungi. Symptoms depend on the infection type but may include ear pain, hearing loss, itching, or discharge.
Treatment often involves antibiotics or steroid ear drops to reduce inflammation and clear the infection. Prevention is typically straightforward, involving good personal hygiene and avoiding contaminated water. Prompt treatment and preventive measures can help avoid complications like hearing loss and, in severe cases, infections spreading to nearby areas.
Table of Contents
Symptoms of Ear Infection

The symptoms of an ear infection vary based on the specific type of infection. Here are common symptoms associated with different types of ear infections:
- Swelling and redness of the ear. Infection often causes parts of the ear to become swollen and red. This symptom is common across most types of ear infections.
- Ear pain. Ear pain is frequently experienced, especially in cases of otitis externa (outer ear infection), otitis media (middle ear infection), and acute mastoiditis (infection of the mastoid bone).
- Presence of pus or fluid in the ear. Infections can lead to a buildup of fluid or pus, causing blockage. This symptom is seen in otitis externa, otitis media, infectious myringitis, and acute mastoiditis. It is also a primary symptom in cases of serous otitis media, where fluid accumulates without infection.
- Itchy ear. Itching in the ear is commonly associated with otitis externa, often due to fungal infections or irritation.
- Temporary hearing loss. Swelling and fluid buildup can lead to temporary hearing impairment. This is often due to blockage or inflammation, common in otitis media and other middle ear infections.
- Fever. The body may respond to the infection with a fever as it tries to fight off the infection. This is commonly seen in otitis media, infectious myringitis, and acute mastoiditis.
- Loss of balance, dizziness, or vertigo. Inner ear infections such as vestibular neuronitis or herpes zoster oticus (shingles in the ear) can lead to balance issues, dizziness, or vertigo due to their impact on the inner ear.
- Painful small blisters in the ear. Painful blisters may form in cases of infectious myringitis or herpes zoster oticus. These can cause significant discomfort and may require specific treatments.
Ear infection symptoms can vary in intensity and may overlap, making proper diagnosis by a healthcare provider essential for effective treatment and to prevent complications.
Types of Ear Infections
There are many types of ear infections, and determining the exact type requires examination by a doctor. Here are the different types of ear infections:
- Otitis externa. Also known as “swimmer’s ear,” otitis externa occurs when the outer ear canal becomes infected. It is often caused by swimming in contaminated water, physical trauma to the ear, or frequent ear cleaning, which disrupts the ear’s natural defenses. The infection can be due to bacteria or fungi.
- Otitis media. This infection affects the middle ear and can be caused by viruses or bacteria. Otitis media can lead to complications such as meningitis, labyrinthitis, hearing loss, and facial paralysis if left untreated. Otitis media can present in various forms:
- Acute otitis media. This is a short-term infection and the most common type of otitis media in children. It usually resolves with proper treatment.
- Chronic otitis media. Chronic otitis media refers to a long-lasting or recurring middle ear infection. It often occurs when contaminated fluid remains trapped in the middle ear.
- Serous otitis media (glue ear). In this condition, thick fluid builds up in the middle ear, increasing the risk of infection. It commonly affects children between 6 months and 2 years old.
- Otitis interna. When the inner ear is affected, the condition is known as otitis interna, also referred to as labyrinthitis or vestibular neuritis. This infection can lead to permanent hearing loss if not treated promptly. It typically impacts balance due to its effect on the inner ear.
- Infectious myringitis. Infectious myringitis is an infection of the eardrum, causing inflammation and small, painful blisters in the ear. It can be triggered by either bacterial or viral infections.
- Acute mastoiditis. This condition occurs when the mastoid bone (located behind the ear) becomes infected, often as a complication of untreated acute otitis media. Without prompt treatment, acute mastoiditis can lead to severe complications, including hearing loss, blood poisoning (sepsis), meningitis, and facial paralysis.
- Vestibular neuronitis. This infection affects the vestibular system, which helps control balance. It is typically caused by a viral infection and can lead to intense dizziness and balance problems.
- Herpes zoster oticus (shingles in the ear). This condition can develop in individuals who have had chickenpox or shingles. It often affects the auditory nerves, leading to pain and sometimes hearing loss. In severe cases, the infection can spread to other facial nerves, causing inflammation and facial paralysis.
Identifying the specific type of ear infection is essential for proper treatment and to avoid complications. Prompt medical care and adherence to prescribed treatments can greatly reduce the risk of long-term effects.
Diagnostic Procedures for Ear Infection
Diagnosing an ear infection requires a combination of physical examination and diagnostic tests to identify the specific type and severity of the infection. Here are some commonly used procedures:
- Physical examination and medical history. The diagnostic process typically begins with a doctor reviewing the patient’s symptoms and medical history, including any recent respiratory infections or activities like swimming that may have contributed to the infection. The doctor will also examine the ear for visible signs of infection, such as redness, swelling, or discharge.
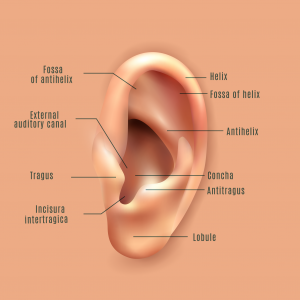
- Otoscopy. Using an otoscope, a lighted device for examining the ear canal and eardrum, the doctor looks for signs of infection, such as fluid behind the eardrum, redness, or swelling. This examination helps identify the location and extent of the infection, such as in cases of otitis media or otitis externa.
- Tympanometry. This test measures the movement of the eardrum in response to changes in air pressure. Tympanometry can help determine if there is fluid in the middle ear or if the eustachian tubes are blocked, which is common in middle ear infections (otitis media).
- Hearing test (audiometry). In cases of chronic or severe ear infections, a hearing test may be conducted to assess the impact on hearing. This test can help determine if there is any temporary or permanent hearing loss due to the infection or damage to the middle or inner ear structures.
- Ear culture (fluid sample). If the infection is severe, recurrent, or resistant to standard treatments, the doctor may collect a fluid sample from the ear to identify the specific bacteria, virus, or fungus causing the infection. This information is useful for selecting targeted treatment, especially in persistent cases.
- Imaging tests (CT scan or MRI). In rare cases where complications are suspected, such as mastoiditis (infection of the bone behind the ear) or potential spread of the infection, imaging tests like CT scans or MRIs may be performed to assess the surrounding structures and rule out any serious complications.
These diagnostic procedures provide valuable information that helps healthcare providers confirm the presence and type of ear infection, allowing for targeted treatment and better outcomes. Prompt and accurate diagnosis is essential for effective treatment and prevention of complications.
Complications of Untreated Ear Infection
When an ear infection goes untreated, it can lead to several complications, some of which may have long-term effects on hearing and overall health. Here are some possible complications:
- Hearing loss. Persistent ear infections can lead to temporary or permanent hearing loss. In severe cases, untreated infections can damage the middle or inner ear structures, leading to more significant hearing impairment.
- Eardrum rupture. The buildup of fluid and pressure from an untreated ear infection can cause the eardrum to rupture. While the eardrum often heals on its own, repeated ruptures can lead to scarring and chronic issues with hearing.
- Chronic otitis media. An untreated middle ear infection can become chronic, resulting in continuous or recurring infections. Chronic otitis media can lead to long-term issues with ear drainage and hearing, often requiring ongoing medical attention.
- Mastoiditis. If a middle ear infection spreads to the mastoid bone (located behind the ear), it can cause mastoiditis. This infection can lead to bone damage, abscesses, and even require surgical intervention if not managed promptly.
- Labyrinthitis. Untreated infections that spread to the inner ear may cause labyrinthitis, leading to balance problems, dizziness, and vertigo. This can interfere with daily life and may cause prolonged discomfort.
- Meningitis. In rare cases, untreated ear infections can spread to the surrounding areas and lead to meningitis, a serious infection of the brain and spinal cord membranes. Meningitis can be life-threatening and requires immediate medical attention.
- Facial nerve paralysis. Severe middle ear infections can sometimes lead to inflammation of the facial nerve, causing temporary or permanent facial paralysis. This is more likely if the infection spreads or if the facial nerve is located close to the middle ear.
- Brain abscess. Though very rare, untreated ear infections can lead to an abscess in the brain if the infection spreads beyond the ear structures. This is a life-threatening condition that requires emergency medical intervention.
Prompt treatment and regular follow-up care for ear infections are essential to prevent these complications. Managing ear infections early not only alleviates symptoms but also reduces the risk of severe and long-lasting effects on health.
Causes of Ear Infection
The various causes of ear infections can help identify the type of infection a person might develop. Here are some common causes:
- Bacteria, viruses, and fungi. The primary causes of ear infections are exposure to bacteria, viruses, and fungi, which can trigger inflammatory reactions in the ear. Infection can occur if these pathogens enter the ear canal, often through frequent touching of the ear or exposure to contaminated water while bathing or swimming.
- Complications from colds and flu. Ear infections can develop as complications from other illnesses, such as colds or influenza. Because the sinuses and throat are close to the ears, infections in these areas can easily spread to the ear, especially in young children.
- Allergies. Severe allergies can also lead to ear infections. Allergic reactions may cause swelling and fluid buildup in the ear, creating an environment where bacteria or viruses can thrive, leading to infection.
- Failure to dry the ear thoroughly after swimming or bathing. Water left in the ear canal can create a moist environment, ideal for bacterial, viral, or fungal growth, which can lead to ear infections, especially in the outer ear.
- Frequent ear cleaning. Earwax (cerumen) plays a protective role by trapping bacteria, viruses, and fungi, preventing them from entering deeper into the ear canal. Frequent cleaning can strip the ear of this natural defense, making it more susceptible to infection.
- Sudden changes in air pressure. Rapid changes in air pressure, such as those experienced during airplane travel or diving, can affect the middle ear and potentially lead to infection if the eustachian tubes become blocked or damaged.
Understanding these causes can help prevent ear infections and promote better ear health. Avoiding excessive ear cleaning, thoroughly drying the ears after exposure to water, and taking precautions during cold and flu season can reduce the risk of developing ear infections.
Prevention of Ear Infection

The following practices can help prevent ear infections:
- Avoid swimming or bathing in contaminated water. Exposure to dirty or polluted water increases the risk of bacterial, viral, or fungal infections in the ear.
- Wash hands frequently and thoroughly. Regular handwashing reduces the spread of germs that could cause infections, including those that can reach the ear through contact.
- Avoid crowded places. Staying away from crowded areas, especially during cold and flu season, helps reduce the risk of respiratory infections that can lead to ear complications.
- Avoid smoky environments. Exposure to smoke and other pollutants can irritate the respiratory tract and increase susceptibility to infections, including ear infections.
- Quit smoking. Smoking weakens the immune system and damages tissues in the respiratory and ear passages, making infections more likely. Quitting smoking supports better ear and respiratory health.
- Dry ears properly after swimming or bathing. Ensuring that ears are thoroughly dried after water exposure can prevent moisture buildup, reducing the chance for bacterial or fungal growth in the ear canal.
These preventive measures can help maintain ear health and reduce the risk of infections. Practicing good hygiene and avoiding harmful environments are key steps toward preventing ear infections and promoting overall ear wellness.
Risk Factors for Ear Infection

The following factors increase the likelihood of developing an ear infection:
- Frequent swimming. Regular swimming can lead to trapped water in the ear, creating a moist environment that increases the risk of ear infections, particularly outer ear infections.
- Diabetes. Ear infections can be a complication of diabetes, as higher blood sugar levels may impair the body’s ability to fight infections, including those in the ear.
- Weakened immune system. Individuals with weakened immune systems, such as those with autoimmune disorders, are more susceptible to infections, including ear infections, as their bodies are less able to fend off pathogens.
- Skin conditions, such as eczema or psoriasis. Skin conditions that affect the ear canal, like eczema and psoriasis, can make the skin more prone to irritation and infection.
- Smoking or exposure to smoke. Smoking and exposure to secondhand smoke irritate the respiratory tract and ear passages, raising the risk of ear infections.
- Frequent air travel. Frequent changes in air pressure, such as those experienced during air travel, can stress the middle ear and increase susceptibility to infections, especially if the eustachian tubes are blocked.
- Young age. Children are more prone to ear infections because their immune systems are still developing, and their eustachian tubes are shorter and more easily blocked.
These risk factors highlight the importance of taking preventive measures, especially for individuals with underlying conditions. Reducing exposure to risk factors can help lower the chances of developing an ear infection.
Ear Infection FAQs
Ear infections are common, yet they can be confusing and concerning. Here are some frequently asked questions about ear infections, their causes, and treatments.
- What is an ear infection?
An ear infection occurs when bacteria, viruses, or fungi cause inflammation in one or more parts of the ear. The infection may affect the outer ear (otitis externa), middle ear (otitis media), or inner ear (otitis interna), each with different symptoms and treatments. - What causes ear infections?
Ear infections are typically caused by bacteria or viruses. Factors that increase the risk include respiratory infections, allergies, exposure to cigarette smoke, and water exposure (especially contaminated water). A weakened immune system or conditions like diabetes can also raise the risk. - Who is most at risk for ear infections?
Children are more prone to ear infections because their eustachian tubes are shorter and more easily blocked. Adults with weakened immune systems, chronic conditions, or frequent exposure to water (e.g., swimmers) are also at higher risk. - What are the symptoms of an ear infection?
Common symptoms include ear pain, itching, hearing loss, fluid discharge, and in some cases, fever. Inner ear infections may cause dizziness, vertigo, or balance issues, while outer ear infections may cause swelling and redness. - How is an ear infection diagnosed?
A doctor typically uses an otoscope to examine the ear canal and eardrum. Additional tests, like tympanometry or hearing tests, may be used to assess the extent of the infection or fluid buildup. - Are ear infections contagious?
Ear infections themselves are not contagious, but the viruses and bacteria that cause them (such as those behind colds or the flu) can spread to others, increasing their risk of infection. - Can ear infections resolve on their own?
Some mild ear infections, especially viral ones, may clear up without treatment. However, bacterial infections or more severe cases often require antibiotics or other treatments to prevent complications. - How are ear infections treated?
Treatment depends on the type and severity of the infection. Mild cases may be managed with pain relievers, warm compresses, or eardrops. Bacterial infections may require antibiotics, while chronic or severe infections may need more intensive treatment. - Can ear infections cause hearing loss?
Yes, ear infections can lead to temporary hearing loss due to fluid buildup or inflammation. Chronic or untreated infections may cause permanent damage to the ear structures, resulting in lasting hearing loss. - How can I prevent ear infections?
Preventive steps include maintaining good hygiene, avoiding contaminated water, thoroughly drying ears after swimming, and keeping up with vaccinations (like the flu shot) to reduce infection risks. - When should I see a doctor for an ear infection?
If you or your child experiences severe pain, fever, fluid discharge, or symptoms lasting more than a few days, it’s essential to see a doctor. Persistent symptoms may indicate a more serious infection that requires medical treatment.


