Summary
Peptic ulcers refer to sores or lesions that develop on the lining of the stomach, small intestine, or esophagus, often causing severe abdominal pain. These ulcers are categorized based on their location: gastric ulcers affect the stomach, duodenal ulcers occur in the first part of the small intestine, and esophageal ulcers are found in the esophagus. The primary cause of these ulcers is an infection by the bacteria Helicobacter pylori, which weakens the protective lining of the digestive tract, allowing acid to cause irritation and sores.
Although peptic ulcers can sometimes heal on their own, they should not be ignored, as untreated ulcers can lead to more serious complications, such as bleeding, perforation (a hole in the stomach or intestinal wall), or obstruction.
Table of Contents
Symptoms of Peptic Ulcer

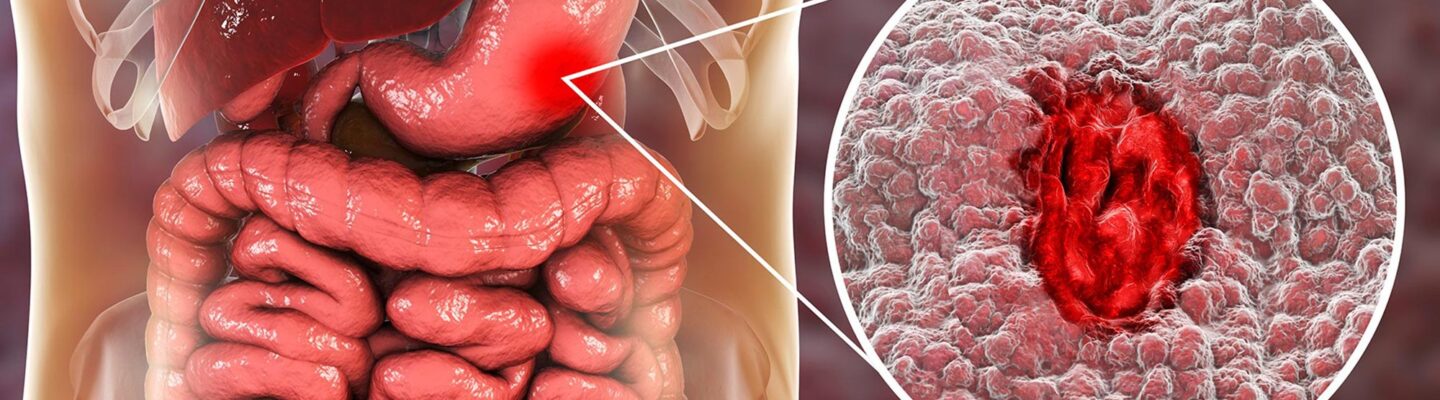
Image Source: health.clevelandclinic.org
Peptic ulcers can manifest with various symptoms, which often depend on the location and severity of the ulcer. Common symptoms include the following:
- Burning stomach pain. The most common symptom, a burning or gnawing pain, often occurs between meals or at night when the stomach is empty.
- Bloating. Many individuals feel a sense of fullness or bloating after eating small amounts.
- Nausea or vomiting. Peptic ulcers can lead to frequent nausea, and some people may vomit as a result.
- Heartburn. Acid reflux or heartburn is common, especially when the ulcer is located in the stomach or esophagus.
- Loss of appetite. Pain or discomfort may reduce appetite, particularly if eating exacerbates symptoms.
- Unintentional weight loss. Reduced appetite or vomiting can contribute to unintended weight loss.
- Dark or bloody stools. This can indicate bleeding in the gastrointestinal tract due to the ulcer, often a sign of a more severe ulcer.
- Vomiting blood. Blood in vomit may appear red or have a coffee-ground texture, indicating internal bleeding.
These symptoms can vary in intensity, and some individuals may experience only mild symptoms or no symptoms at all. However, if symptoms are persistent or worsening, it’s essential to seek medical evaluation to confirm the presence of an ulcer and avoid potential complications.
Types of Peptic Ulcer
Peptic ulcers are classified based on their location within the digestive tract. Each type has distinct features and may cause different symptoms, though all result from the erosion of the mucosal lining due to stomach acid and other factors.
- Gastric Ulcer. This type of ulcer forms on the lining of the stomach. It is often associated with stomach pain that worsens after eating and may be more common in older adults. Gastric ulcers can be aggravated by spicy foods, alcohol, and certain medications.
- Duodenal Ulcer. These ulcers are located in the upper part of the small intestine, called the duodenum. Duodenal ulcers typically cause pain that improves after eating but returns a few hours later. They are generally more common than gastric ulcers and can affect individuals of all ages.
- Esophageal Ulcer. This type forms in the lining of the esophagus, the tube connecting the throat to the stomach. Esophageal ulcers are often caused by acid reflux, where stomach acid moves upward into the esophagus, causing damage to its lining. Symptoms may include heartburn, chest pain, and difficulty swallowing.
Each type of peptic ulcer results from similar mechanisms, including bacterial infection (such as Helicobacter pylori) and the use of NSAIDs (non-steroidal anti-inflammatory drugs) that can erode the protective lining of the digestive tract. Recognizing the type and location of an ulcer is crucial for effective treatment, as certain therapies may target specific ulcer sites more efficiently.
Diagnostic Procedures for Peptic Ulcer
Diagnosing a peptic ulcer typically involves a combination of medical history, physical examination, and specific tests to confirm the presence and location of the ulcer. The following are commonly used diagnostic procedures:
- Medical History and Physical Exam. Doctors will review the patient’s symptoms, medical history, and any risk factors such as NSAID use, smoking, or previous ulcers. They may also perform a physical exam, pressing gently on the abdomen to assess pain or tenderness.
- Endoscopy. An endoscopy is a common procedure for diagnosing peptic ulcers. A thin, flexible tube with a camera (endoscope) is inserted through the mouth and down the esophagus to examine the lining of the stomach and small intestine. If an ulcer is found, a biopsy may be taken to check for Helicobacter pylori infection or to rule out cancer in the stomach lining.
- Upper Gastrointestinal (GI) Series. For this imaging test, the patient drinks a barium solution, which coats the lining of the digestive tract and makes ulcers visible on X-rays. This procedure is useful for detecting ulcers when endoscopy is unavailable, though it’s less commonly used today.
- H. pylori Tests. Several tests are available to detect the H. pylori bacteria, a leading cause of peptic ulcers. These tests include:
- Breath Test. The patient drinks a solution containing a harmless radioactive substance. If pylori is present, it will produce an enzyme that breaks down the solution, releasing carbon dioxide, which can be detected in the breath.
- Stool Test. This test checks for pylori antigens in a stool sample and is particularly useful for monitoring treatment effectiveness.
- Blood Test. A blood test can detect antibodies to pylori, though it is less reliable for active infections and is generally used less often today.
- Biopsy. During an endoscopy, the doctor may take a small tissue sample (biopsy) from the ulcer area to test for H. pylori or look for signs of other diseases, such as cancer.
- Complete Blood Count (CBC). A CBC may be performed if the doctor suspects bleeding from the ulcer. This test can reveal anemia, which may indicate blood loss.
These diagnostic procedures help confirm the presence of a peptic ulcer, identify the cause, and rule out other conditions with similar symptoms. Accurate diagnosis is essential for choosing the most effective treatment plan and preventing potential complications.
Complications of Untreated Peptic Ulcer
When peptic ulcers are left untreated, they can lead to severe complications that may require urgent medical intervention. The following are the primary complications associated with untreated peptic ulcers:
- Bleeding. One of the most common and dangerous complications, bleeding can occur when an ulcer erodes into a blood vessel. This can lead to symptoms such as vomiting blood (which may look like coffee grounds) or black, tarry stools. Significant blood loss can cause anemia or, in severe cases, lead to life-threatening hemorrhage.
- Perforation. Perforation occurs when the ulcer creates a hole through the wall of the stomach or intestine, allowing digestive juices and food to leak into the abdominal cavity. This condition can cause sudden, intense pain and may lead to peritonitis—an infection of the abdominal cavity lining—which is a medical emergency requiring immediate surgery.
- Gastric Outlet Obstruction. Peptic ulcers, particularly those located near the stomach outlet, can cause swelling, inflammation, or scarring that blocks food from moving from the stomach into the small intestine. Symptoms may include vomiting, bloating, and feelings of fullness after eating. Severe cases of obstruction may require surgical intervention.
- Penetration. In some cases, an ulcer can penetrate or burrow into adjacent organs, such as the pancreas or liver, causing intense pain and further inflammation. Penetration can lead to complex complications, as the ulcer’s damage extends beyond the digestive tract, often requiring advanced treatment.
- Increased Risk of Stomach Cancer. Long-term infection with Helicobacter pylori and chronic inflammation in the stomach can increase the risk of developing stomach (gastric) cancer. Though not common, this risk makes prompt diagnosis and treatment of ulcers caused by H. pylori essential.
Untreated peptic ulcers can progress rapidly, and the resulting complications can be life-threatening if not addressed promptly. Early diagnosis and treatment are key to preventing these risks and ensuring proper healing of the ulcer.
Causes of Peptic Ulcer
Peptic ulcers occur when the protective lining of the stomach, small intestine, or esophagus is compromised, allowing stomach acid to damage the tissue and create sores. The primary direct causes of peptic ulcers are:
- Helicobacter pylori (H. pylori) Infection. This bacterial infection is the most common cause of peptic ulcers. H. pylori disrupts the protective mucous layer that lines the stomach and small intestine, making it easier for stomach acid to damage the underlying tissue. The bacteria also produce enzymes and toxins that weaken the mucosal defenses, which can directly lead to ulcer formation.
- Excessive Use of NSAIDs. Frequent or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen, can directly erode the protective mucosal lining of the stomach and duodenum. NSAIDs inhibit the production of certain chemicals (prostaglandins) that help maintain the stomach’s protective barrier, leaving the tissue more vulnerable to acid damage.
- Excess Stomach Acid Production. Conditions that lead to the overproduction of stomach acid can directly cause peptic ulcers. This can include rare conditions such as Zollinger-Ellison syndrome, where tumors in the pancreas or duodenum stimulate excessive acid production. In such cases, the high acid levels overwhelm the mucosal defenses and result in ulceration.
These are the primary, direct causes of peptic ulcers. Other factors like smoking, alcohol, and stress are not direct causes but can exacerbate the severity of ulcers or delay healing.
Prevention of Peptic Ulcer
Preventing peptic ulcers involves minimizing the factors that can damage the lining of the stomach, small intestine, and esophagus. The following strategies can help reduce the risk of developing an ulcer:
- Limit NSAID use. Avoid frequent or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, aspirin, and naproxen. If NSAIDs are necessary, use the lowest effective dose and discuss alternatives with your doctor, such as acetaminophen or protective medications like proton pump inhibitors (PPIs).
- Practice good hygiene to avoid H. pylori. Since H. pylori infection is a leading cause of ulcers, maintaining good hygiene can help prevent infection. Wash hands thoroughly with soap and water, especially before eating and after using the restroom, and ensure food and water sources are clean.
- Limit alcohol consumption. Alcohol can irritate and erode the stomach lining, increasing vulnerability to ulcers. Limiting alcohol intake, especially if you use NSAIDs or have a history of gastrointestinal issues, can help prevent damage to the digestive lining.
- Avoid smoking. Smoking increases stomach acid production and impairs the protective mucous barrier of the stomach, which can lead to ulcer formation. Quitting smoking can significantly reduce the risk of peptic ulcers and improve overall gastrointestinal health.
- Manage stress. Although stress is not a direct cause of ulcers, chronic stress can contribute to behaviors that increase ulcer risk, such as smoking, alcohol consumption, and poor diet. Practicing relaxation techniques, such as exercise, meditation, or breathing exercises, can help manage stress and reduce its impact on digestive health.
- Follow a balanced diet. While diet alone doesn’t cause ulcers, eating a balanced diet rich in fruits, vegetables, and fiber can support overall digestive health. Avoiding overly spicy foods, caffeine, and acidic foods may help prevent irritation, especially if you have a sensitive stomach.
By taking these preventive steps, individuals can lower their risk of developing peptic ulcers and maintain a healthy digestive system. Those with a history of ulcers or H. pylori infection should consult with a healthcare provider for personalized preventive strategies.
Risk Factors for Peptic Ulcer
Certain factors increase the likelihood of developing a peptic ulcer by weakening the protective lining of the stomach, small intestine, or esophagus or by contributing to excess stomach acid production. Key risk factors include:
- Helicobacter pylori (H. pylori) infection. This bacterial infection is a significant risk factor for peptic ulcers, as it disrupts the protective mucous lining in the stomach and small intestine, making them more susceptible to damage from stomach acid.
- Regular use of NSAIDs. Non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen, can irritate and erode the stomach lining, especially when used frequently or in high doses. Long-term NSAID use is particularly risky for older adults.
- Smoking. Smoking can increase stomach acid production, damage the stomach lining, and slow the healing of existing ulcers. Smokers who are infected with H. pylori are at an even greater risk for ulcer formation.
- Excessive alcohol consumption. Heavy alcohol use can erode the stomach lining and increase stomach acid production, both of which heighten the risk of developing peptic ulcers.
- High-stress levels. Chronic stress doesn’t directly cause ulcers but may exacerbate symptoms or delay healing. Stress can also lead to lifestyle habits, such as smoking or drinking, that increase ulcer risk.
- Diet high in spicy or acidic foods. While diet alone doesn’t cause ulcers, spicy or acidic foods can worsen symptoms in individuals with existing ulcers or a predisposition to digestive issues.
- History of ulcers or gastrointestinal problems. People who have had previous ulcers, particularly if caused by H. pylori infection or NSAID use, have an increased risk of recurrence.
- Family history of ulcers. A family history of peptic ulcers may indicate a genetic predisposition, as some individuals may inherit a higher risk of excessive stomach acid production or a weaker stomach lining.
Recognizing and managing these risk factors can help reduce the chances of developing peptic ulcers. Those with multiple risk factors should consult a healthcare provider for guidance on minimizing their exposure and maintaining a healthy digestive system.
Peptic Ulcer FAQs
Understanding peptic ulcers is essential for managing symptoms and preventing complications. Here are answers to some frequently asked questions:
- What is a peptic ulcer?
A peptic ulcer is a sore that forms on the lining of the stomach, small intestine, or esophagus. It occurs when the protective lining is damaged, allowing stomach acid to irritate and erode the tissue. - What causes peptic ulcers?
The primary causes of peptic ulcers are infection by Helicobacter pylori bacteria and long-term use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen. Excess stomach acid, smoking, and excessive alcohol use can also contribute to ulcer formation. - What are the symptoms of a peptic ulcer?
Common symptoms include burning stomach pain (especially when the stomach is empty), bloating, heartburn, nausea, vomiting, loss of appetite, and unintentional weight loss. Severe symptoms, such as vomiting blood or dark stools, may indicate complications and require immediate medical attention. - Can stress cause peptic ulcers?
While stress alone does not cause peptic ulcers, it can worsen symptoms and delay healing in individuals who already have ulcers. Stress-related behaviors, like smoking, drinking, or poor dietary habits, may also increase the risk of ulcers. - How are peptic ulcers diagnosed?
Peptic ulcers are diagnosed through a combination of medical history, physical examination, and specific tests such as endoscopy, upper gastrointestinal (GI) series, or tests for H. pylori (breath, stool, or blood tests). - What treatments are available for peptic ulcers?
Treatment typically involves antibiotics to clear H. pylori infection, proton pump inhibitors (PPIs) or H2 blockers to reduce stomach acid, and medications to protect the stomach lining. Avoiding NSAIDs and lifestyle modifications may also help healing and prevent recurrence. - Can peptic ulcers heal on their own?
Some mild ulcers may heal without treatment, but most require medical intervention, especially if caused by H. pylori or NSAIDs. Untreated ulcers can lead to severe complications, so it’s essential to seek medical advice if symptoms persist. - Are peptic ulcers preventable?
Yes, there are preventive measures to reduce the risk of peptic ulcers, such as limiting NSAID use, practicing good hygiene to prevent H. pylori infection, avoiding smoking and excessive alcohol, and managing stress. - What are potential complications of untreated peptic ulcers?
Untreated peptic ulcers can lead to serious complications, including bleeding, perforation (a hole in the stomach or intestinal wall), gastric outlet obstruction, and an increased risk of stomach cancer. - Can diet impact peptic ulcers?
While diet alone does not cause peptic ulcers, certain foods can aggravate symptoms in individuals with ulcers. It’s generally recommended to avoid spicy, acidic, or fatty foods and consume a balanced diet to support digestive health.