Summary
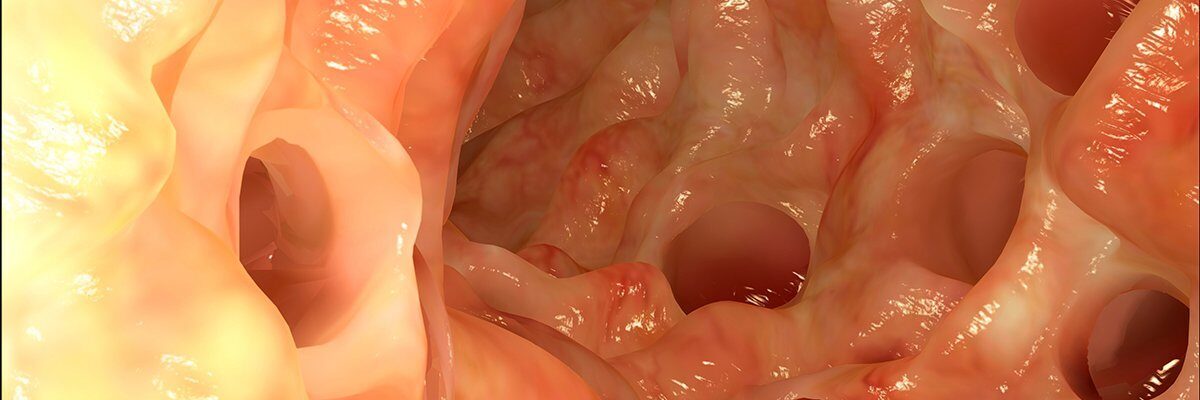
Diverticulitis is a condition that affects the digestive system when small, pouch-like structures called diverticula form in the walls of the large intestine and bulge outward. These pouches can become inflamed or infected, leading to various symptoms and complications. The condition is commonly seen in adults over 40, often linked to age-related weakening of the colon walls.
One of the main causes of diverticulitis is a lack of dietary fiber. Low fiber intake can make stools harder and increase pressure on the colon walls, contributing to the formation of diverticula. Symptoms of diverticulitis include pain (typically in the lower left abdomen), constipation, and sometimes blood in the stool. Other signs may include fever, nausea, and changes in bowel habits.
Mild cases of diverticulitis may resolve with rest, dietary changes, and antibiotics. However, if the condition is severe or recurrent, surgery may be necessary to remove the affected portion of the colon. Early diagnosis and lifestyle changes, such as increasing fiber intake, can help manage diverticulitis and reduce the likelihood of complications.
Table of Contents
Symptoms of Diverticulitis

Some common symptoms of diverticulitis include:
- Pain in the lower left abdomen lasting for several days. This is the most typical symptom of diverticulitis, often felt as a constant or cramping pain.
- Fever. The body may develop a fever in response to the infection or inflammation caused by diverticulitis.
- Nausea and vomiting. These symptoms often accompany abdominal pain and may indicate a more severe or complicated case.
- Constipation or diarrhea. While constipation is more common, some people with diverticulitis may also experience bouts of diarrhea.
- Abdominal tenderness or weakness. The affected area in the abdomen may feel sore or sensitive to touch.
- Blood in the stool. In some cases, diverticulitis may cause minor bleeding in the colon, leading to blood in the stool.
- Cramping on the left side of the abdomen that eases with gas release. Gas buildup can increase abdominal discomfort, and relief may occur after passing gas.
These symptoms can vary in severity depending on the individual and the extent of the inflammation or infection. If symptoms persist or worsen, it is essential to consult a healthcare provider, as untreated diverticulitis can lead to complications, including abscess formation or bowel obstruction. Early diagnosis and treatment can help manage symptoms effectively and prevent complications.
Types of Diverticulitis
Diverticular disease is associated with two main conditions: diverticulitis and diverticular bleeding.
Diverticulitis
Diverticulitis occurs when waste and bacteria become trapped in the pouches or pockets (diverticula) that form in the walls of the large intestine. This buildup can cause irritation, infection, and even ulcers within these areas, leading to inflammation. Diverticulitis often disrupts the balance of gut bacteria, reducing beneficial bacteria and increasing harmful bacteria.
This condition can cause pain, infection, and swelling in the affected area, and may lead to the following complications:
- Abscess formation. Infected pockets may develop pus, which can lead to abscesses.
- Rectal bleeding. Inflammation may cause bleeding from the affected area in the colon.
- Intestinal narrowing. Swelling and scar tissue can cause a narrowing of the colon, leading to difficulty passing stool.
- Fistula formation. This condition can create an abnormal connection, such as from the colon to the bladder, allowing waste to pass from one organ to another.
In severe cases, diverticulitis may require surgical intervention to remove or repair the affected portion of the intestine.
Diverticular bleeding
In diverticular bleeding, blood vessels within the muscle layers of the large intestine pass through the diverticula, where they may rupture. When this happens, blood can appear in the stool, usually during bowel movements.
This type of bleeding is often painless. However, blood loss can sometimes cause dizziness or weakness. Diverticular bleeding may stop on its own, but if severe, it can lead to significant complications. In such cases, the following treatments may be necessary:
- Surgery. To stop persistent or severe bleeding.
- Intravenous (IV) fluids. To prevent dehydration and stabilize blood pressure.
- Blood transfusion. To replace lost blood and maintain healthy blood levels.
- Immediate medical care. To monitor and treat complications effectively.
Both diverticulitis and diverticular bleeding can have serious health implications if left untreated. Early diagnosis and appropriate medical care are essential for managing these conditions and preventing potential complications.
Diagnostic Procedures for Diverticulitis
Diagnosing diverticulitis typically involves a combination of physical exams, imaging tests, and laboratory analyses. These procedures help healthcare providers confirm the diagnosis, assess the severity of the condition, and determine the appropriate treatment plan. Here are the most common diagnostic procedures used for diverticulitis:
- Physical examination. The doctor will perform a physical exam, often pressing on the lower abdomen to check for tenderness, pain, or swelling, which are common signs of diverticulitis. They may also assess vital signs for signs of infection, such as fever and elevated heart rate.
- Blood tests. A complete blood count (CBC) can reveal elevated white blood cell levels, indicating infection or inflammation. Blood tests can also check for electrolyte imbalances and signs of anemia if there has been bleeding.
- Urinalysis. A urine test is sometimes conducted to rule out other conditions, such as urinary tract infections or kidney stones, which can present similar abdominal symptoms.
- CT scan (computed tomography). A CT scan of the abdomen is the most accurate imaging test for diagnosing diverticulitis. It can detect inflamed or infected diverticula, as well as complications like abscesses, perforations, or fistulas, allowing doctors to assess the severity of the condition.
- Ultrasound. In some cases, an abdominal ultrasound may be used, particularly for patients who may not tolerate CT scans well. While less detailed than a CT scan, an ultrasound can still reveal signs of inflammation and abscess formation.
- Colonoscopy (after acute infection resolves). Though not used during the acute phase due to the risk of perforation, a colonoscopy may be recommended several weeks after recovery to examine the colon. This helps rule out other conditions and assess for additional diverticula.
- Stool test. In certain cases, a stool test may be done to rule out other causes of symptoms, like infections or inflammatory bowel disease, especially if diarrhea is present.
These diagnostic procedures provide a comprehensive assessment of diverticulitis, enabling healthcare providers to develop an appropriate treatment plan. Early and accurate diagnosis is crucial for effective management, reducing the risk of complications, and promoting a faster recovery.
Complications of Untreated Diverticulitis
If left untreated, diverticulitis can lead to serious and sometimes life-threatening complications. These complications may require intensive medical treatment, including surgery, to prevent further health issues. Here are some of the primary complications associated with untreated diverticulitis:
- Abscess formation. When diverticula become infected, pockets of pus, or abscesses, can form around the inflamed areas in the colon. These abscesses can cause significant pain and may require drainage to prevent further infection.
- Peritonitis. If a diverticulum ruptures, the infection can spread to the abdominal cavity, leading to peritonitis, a severe and life-threatening infection of the abdominal lining. Peritonitis requires immediate medical intervention and usually involves surgery and antibiotic treatment.
- Fistula formation. A fistula is an abnormal connection between two organs. In diverticulitis, the inflamed colon can form a fistula with nearby organs, such as the bladder, leading to symptoms like urinary tract infections or abnormal discharge. Fistulas often require surgical repair.
- Intestinal obstruction. Chronic inflammation and scarring from repeated diverticulitis episodes can narrow the intestinal passage, causing a partial or complete blockage. This can lead to symptoms such as severe abdominal pain, bloating, and vomiting and may require surgical intervention to restore normal bowel function.
- Rectal bleeding. Untreated diverticulitis can cause blood vessels in the colon to rupture, leading to rectal bleeding. Although often painless, severe bleeding can lead to anemia or require emergency treatment if blood loss is significant.
- Sepsis. When the infection spreads beyond the colon, sepsis, a life-threatening response to infection, can occur. Sepsis affects multiple organ systems and requires immediate hospitalization, often in an intensive care unit, where patients may receive IV antibiotics and other intensive treatments.
- Chronic digestive issues. Repeated or severe episodes of diverticulitis can lead to long-term digestive problems, such as irritable bowel syndrome (IBS) symptoms, changes in bowel habits, and chronic abdominal discomfort.
Preventing these complications involves early diagnosis and proper treatment of diverticulitis. Lifestyle changes, such as a high-fiber diet, regular exercise, and prompt medical attention at the first signs of diverticulitis, can help manage symptoms and reduce the risk of complications.
Causes of Diverticulitis

One of the main factors believed to cause diverticulitis is a lack of dietary fiber. Without enough fiber, stool hardens in the large intestine, requiring more force to pass it through. This increased strain on the intestine can weaken its muscle walls, eventually leading to the formation of small pouches called diverticula.
Excessive straining causes these weakened areas to bulge outward, creating diverticula, which can become inflamed or infected, leading to diverticulitis. While fiber deficiency is traditionally linked to diverticulitis, some recent studies question this connection, suggesting that other factors may also play a role.
Current understanding leans toward the idea that muscle wall weakening in the large intestine, rather than fiber deficiency alone, is a key factor in the development of diverticulitis. Nevertheless, maintaining a fiber-rich diet is widely recommended to support digestive health and reduce straining, which may help prevent the formation of diverticula.
Prevention of Diverticulitis

Diverticulitis is relatively easy to prevent with a few simple lifestyle practices that help maintain colon health. Following these preventive steps can significantly reduce the risk of developing diverticulitis:
- Regular exercise. Physical activity promotes regular bowel movements by reducing pressure within the large intestine. Exercise is most effective for preventing diverticulitis when done for at least 30 minutes each day.
- Drinking plenty of water. Staying well-hydrated helps soften stool, making it easier to pass and reducing strain on the intestines. For adults, it’s recommended to drink six to eight glasses of water daily to support digestive health.
- Choosing fiber-rich foods. Fiber helps bulk up and soften stool, which facilitates smoother bowel movements and decreases pressure in the colon. Make it a habit to eat plenty of fruits, vegetables, whole grains, and legumes, as these foods are naturally high in fiber.
By incorporating these habits into daily life, you can support digestive health and minimize the risk of diverticulitis. Maintaining a balanced diet, staying active, and keeping hydrated are essential steps in preventing this condition.
Risk Factors for Diverticulitis

The exact cause of diverticulitis is not yet fully understood, but several risk factors are known to increase the likelihood of developing this condition. These risk factors include:
- Being middle-aged or older. Diverticulitis is more common in adults over 40, as age-related changes weaken the walls of the colon.
- Smoking. Smoking has been associated with an increased risk of diverticulitis and may worsen symptoms in those who have the condition.
- Lack of physical activity. Sedentary lifestyles contribute to digestive issues, including diverticulitis, as regular exercise supports healthy bowel movements and reduces pressure on the colon.
- Obesity. Excess weight, particularly abdominal fat, is linked to a higher risk of developing diverticulitis and more severe complications.
- Low dietary fiber. A diet low in fiber can lead to harder stools, increasing the strain on the intestines and promoting the formation of diverticula.
- High intake of animal fats. Diets high in animal fats, particularly red meat, may increase the risk of diverticulitis, though this risk is believed to be more significant when combined with low fiber intake.
- Certain medications. Some drugs, including steroids, opiates, and non-steroidal anti-inflammatory drugs (NSAIDs), can weaken the intestinal lining, making it more susceptible to inflammation and infection.
Understanding these risk factors can help individuals make informed lifestyle choices to reduce their risk of diverticulitis. A healthy diet, regular physical activity, and avoiding smoking can all contribute to lowering the risk associated with this condition.
Diverticulitis FAQs
Here are some frequently asked questions about diverticulitis, covering its causes, symptoms, prevention, and treatment:
- What is diverticulitis?
Diverticulitis is a condition that occurs when small pouches, known as diverticula, form in the walls of the colon and become inflamed or infected. This inflammation can lead to abdominal pain, fever, and digestive issues. - What causes diverticulitis?
The exact cause of diverticulitis is unclear, but it is often associated with a low-fiber diet, which can lead to hard stools and increased pressure on the colon walls. This pressure may contribute to the formation of diverticula, which can become inflamed and infected. - What are the symptoms of diverticulitis?
Common symptoms include abdominal pain (usually on the lower left side), fever, nausea, vomiting, constipation, or diarrhea. In some cases, there may be blood in the stool. - Who is at risk of developing diverticulitis?
Diverticulitis is more common in people over 40, those who eat low-fiber diets, individuals with sedentary lifestyles, smokers, and people who are overweight. Certain medications, such as NSAIDs and steroids, may also increase the risk. - Can diverticulitis be prevented?
A high-fiber diet rich in fruits, vegetables, and whole grains is thought to reduce the risk of diverticulitis. Regular exercise, staying hydrated, and avoiding smoking can also help prevent the condition. - How is diverticulitis diagnosed?
Diverticulitis is diagnosed through a combination of physical exams, blood tests, and imaging, such as a CT scan, which can identify inflammation or infection in the colon. A colonoscopy may be recommended after an acute episode to assess the colon. - How is diverticulitis treated?
Mild cases are often managed with rest, a temporary liquid diet, and antibiotics to clear the infection. Severe or recurrent cases may require surgery to remove the affected portion of the colon. - Can diverticulitis lead to other health problems?
Yes, untreated diverticulitis can lead to complications such as abscesses, fistulas, intestinal blockages, and, in severe cases, peritonitis or sepsis. Early diagnosis and treatment can help prevent these complications. - Is diverticulitis a lifelong condition?
Diverticulitis can be a recurring condition for some people, but lifestyle changes, such as a high-fiber diet and regular exercise, may help prevent future episodes. In severe cases, surgery may be required to resolve the issue. - When should I see a doctor for diverticulitis?
You should see a doctor if you experience persistent abdominal pain, fever, nausea, or changes in bowel habits, especially if you have a known history of diverticulitis. Severe symptoms, such as intense pain, rectal bleeding, or signs of infection, require immediate medical attention.