Summary
Cancer is the abnormal and uncontrolled growth of harmful cells in the body. To date, there are over 200 known types of cancer. The term “cancer” originates from Hippocrates, who used the words “carcinos” and “carcinoma” to describe tumors. Cancer cells multiply rapidly and spread, crowding out healthy cells and disrupting normal bodily functions. As these abnormal cells continue to grow, they can impair the function of the affected organs, leading to serious health issues. If not treated promptly, cancer can progress to an advanced stage, increasing the risk of mortality.
The symptoms of cancer vary depending on the affected part of the body. However, common signs include unexplained weight loss, significant swelling or enlargement of the affected area, persistent pain, dizziness, and unusual bleeding or bruising. Diagnosing cancer early is crucial, as it significantly improves the chances of successful treatment and recovery.
Treatment options for cancer depend on the type and stage of the disease. These can include chemotherapy, radiation therapy, immunotherapy, and surgery. Each approach aims to eliminate or control the growth of cancer cells and prevent their spread to other parts of the body. Early detection and appropriate medical care are essential for managing cancer and improving patient outcomes.
How Does Cancer Work?
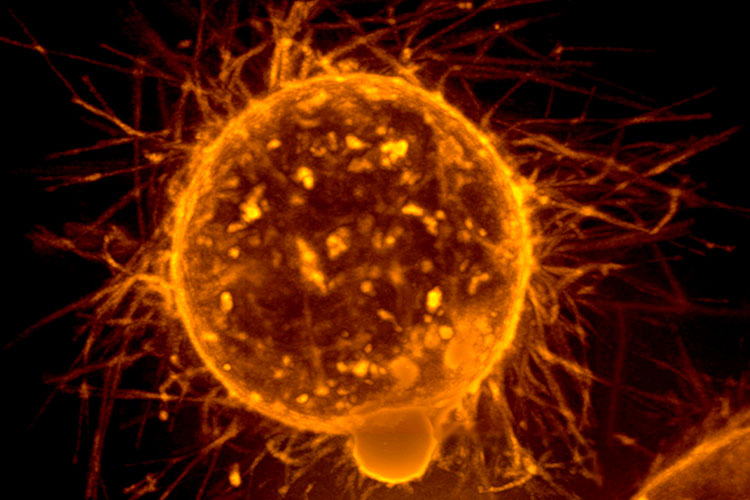
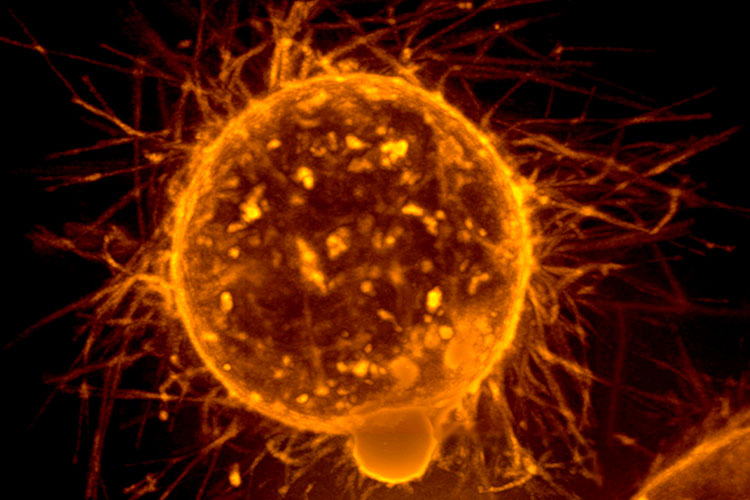
Cancer develops when the body’s normal cell growth and division processes go awry. Normally, cells grow, divide, and die in a controlled manner. However, in the case of cancer, genetic mutations disrupt this cycle. These mutations cause cells to grow and divide uncontrollably, forming masses or tumors. These tumors can either be benign (non-cancerous) or malignant (cancerous). Malignant tumors have the ability to invade nearby tissues and spread to other parts of the body, a process known as metastasis.
The progression of cancer typically starts with a few abnormal cells that multiply, forming a primary tumor. As the tumor grows, it can interfere with the normal function of the tissue or organ where it developed. For example, a tumor in the lungs may obstruct breathing, while one in the colon may interfere with digestion.
Malignant cells have the ability to break away from the original tumor and travel through the blood or lymphatic system to other parts of the body. Once these cells reach a new location, they can form secondary tumors, leading to further complications. This spread is what often makes cancer particularly dangerous, as it can cause damage to multiple organs.
The exact causes of these genetic mutations are varied and can include exposure to carcinogens (such as tobacco smoke or radiation), viral infections, chronic inflammation, or inherited genetic mutations. However, not all mutations result in cancer, as the body has mechanisms to repair DNA damage or trigger cell death if the damage is too severe. When these mechanisms fail, the abnormal cells can survive, proliferate, and eventually form cancerous growths. Understanding how cancer develops and spreads is crucial for determining effective treatments and improving survival rates.
Symptoms of Cancer

The symptoms of cancer can vary depending on the part of the body affected. However, most types of cancer share common signs and changes in the body, which may include:
- Development of lumps or swelling in certain areas of the body. Unexplained lumps can be a warning sign, especially if they persist or grow over time.
- Pain in the affected area. Persistent or worsening pain, especially in specific regions, may be indicative of cancer.
- Presence of blood in urine (hematuria) or stool (hematochezia). This can be a sign of cancers in the urinary or digestive tract.
- Extreme fatigue or lethargy. Unlike ordinary tiredness, cancer-related fatigue is more severe and doesn’t improve with rest.
- Frequent muscle and joint pain. Persistent discomfort or unexplained aches can sometimes be related to underlying malignancies.
- Unexplained recurring fevers. Many types of cancer can cause a chronic, low-grade fever as the body fights the disease.
- Unexplained bruising or bleeding. Easy bruising or frequent bleeding, such as from the gums or nose, may indicate blood cancers like leukemia.
- Unintended weight changes. Sudden weight loss or, in some cases, unexpected weight gain can be a symptom, especially if it occurs without changes in diet or physical activity.
- Changes in skin color or texture. Skin may become darker, yellowish (jaundice), red, or more prone to itching or rashes.
- Wounds or sores that do not heal. Persistent wounds, particularly those in the mouth or on the skin, can be warning signs of cancer.
- Changes in bowel habits or urination patterns. Persistent diarrhea, constipation, or changes in the frequency and urgency of urination may be related to cancers of the digestive or urinary systems.
- Chronic cough or difficulty breathing. A lingering cough or shortness of breath, especially when unexplained, can be a symptom of lung cancer.
- Difficulty swallowing. Persistent difficulty or pain when swallowing may be related to cancers of the throat or esophagus.
- Hoarseness of voice. Persistent hoarseness or voice changes can be a sign of cancers in the throat or larynx.
- Frequent indigestion or heartburn. Ongoing digestive discomfort, especially if it is accompanied by difficulty swallowing or a feeling of fullness after eating small amounts, may be related to cancers of the stomach or esophagus.
While these symptoms are common in many types of cancer, they can also be caused by less serious conditions. It is important to consult a healthcare professional if any of these symptoms persist or worsen, especially if they occur without a known cause. Early detection significantly increases the chances of successful treatment.
Types of Cancer
Cancer is classified into four main categories based on where it begins in the body. Understanding these categories helps in determining the most appropriate treatment and approach for each type. Here are the main types of cancer:
Leukemia is a type of cancer that originates in the blood-forming tissues, such as the bone marrow, causing an abnormal increase in white blood cells. This overproduction of cells disrupts the balance of healthy blood cells, leading to various complications, including anemia, infections, and excessive bleeding. Examples include Acute Lymphoblastic Leukemia (ALL) and Chronic Myeloid Leukemia (CML).
Lymphoma refers to cancers that develop in the lymphatic system, which is a crucial part of the immune system. These cancers affect the lymph nodes and can spread throughout the body. The two primary types of lymphoma are Hodgkin lymphoma and non-Hodgkin lymphoma, each with distinct characteristics and treatment protocols.
Sarcomas are cancers that begin in the connective tissues of the body, including bones, muscles, tendons, and fat. They are less common than other types of cancers but can be aggressive. Examples include osteosarcoma (bone cancer) and liposarcoma (cancer in fat tissues).
4. Carcinoma
Carcinomas are cancers that originate in the skin or tissues that line internal organs. These cancers often begin as tumors and can spread to other parts of the body. Common examples include breast cancer, lung cancer, prostate cancer, and colorectal cancer. Carcinomas are the most prevalent type of cancer among adults.
Comprehensive List of Cancer Types
Here is an alphabetical list of various types of cancers, affecting different parts of the body:
Cancer by Age and Stage
- Cancers Common in Adults: Many types of cancers, such as breast cancer, lung cancer, and prostate cancer, are more frequently seen in adults, often developing as people age.
- Cancers in Children and Infants: Certain cancers like retinoblastoma, Wilms tumor, and certain types of leukemia are more likely to occur in children and infants.
- Hard-to-Detect Cancers: Some cancers, such as pancreatic cancer or liver cancer, may not show symptoms in their early stages. As a result, many patients may only discover they have these cancers when they have already advanced, making treatment more challenging.
Regular screenings and early detection are essential in managing cancer effectively. Individuals with a family history of cancer are strongly advised to have regular check-ups with an oncologist, as early diagnosis significantly increases the chances of successful treatment and better outcomes.
Diagnostic Procedures for Ceancer
Diagnosing cancer involves various tests and procedures that help detect the presence, type, and extent of the disease. The goal is to identify cancer early, determine its stage, and guide the appropriate treatment plan. Here are some common diagnostic procedures used in cancer detection:
- Physical Examination. A thorough physical exam is often the first step in diagnosing cancer. During this exam, the doctor checks for lumps, skin changes, or other unusual signs that could indicate a tumor. They may also review the patient’s medical history to identify symptoms that may suggest cancer, such as unexplained weight loss, persistent fatigue, or chronic pain.
- Blood Tests. Blood tests help detect abnormalities that could indicate cancer. Specific tests like a complete blood count (CBC) can reveal abnormal levels of white blood cells, which may suggest blood cancers like leukemia. Tumor markers, such as prostate-specific antigen (PSA) for prostate cancer or CA-125 for ovarian cancer, can also be measured to assess the likelihood of certain types of cancer.
- Imaging Tests. Imaging tests are crucial in visualizing tumors and determining the extent of cancer. Common imaging tests include:
- X-rays. X-rays can help detect tumors in areas like the lungs or bones. They are often used as an initial screening tool.
- CT Scan (Computed Tomography). A CT scan uses X-rays to create detailed cross-sectional images of the body. It is commonly used to detect tumors in the chest, abdomen, and pelvis, as well as to monitor cancer progression.
- MRI (Magnetic Resonance Imaging). MRI uses strong magnetic fields and radio waves to create detailed images of soft tissues. It is especially useful for detecting brain, spinal cord, and breast cancers.
- Ultrasound. This test uses sound waves to produce images of internal organs. It is commonly used to detect tumors in areas like the liver, kidneys, and abdomen.
- PET Scan (Positron Emission Tomography). PET scans use a small amount of radioactive material to detect cancerous activity in tissues. They are often used to identify cancer spread (metastasis) and evaluate the effectiveness of treatment.
- Biopsy. A biopsy involves removing a small sample of tissue or cells from the suspected area and examining it under a microscope. It is the most definitive way to diagnose cancer. Types of biopsy include:
- Needle Biopsy. A thin needle is used to extract cells from a lump or suspicious area, such as a breast lump or lymph node.
- Core Needle Biopsy. A larger needle is used to remove a small cylinder of tissue, providing more information about the tumor.
- Surgical Biopsy. A surgeon removes a portion or the entire suspicious mass for further examination, especially when a needle biopsy is insufficient.
- Endoscopic Biopsy. This involves using a thin, flexible tube with a camera (endoscope) to examine internal organs like the lungs or digestive tract. If abnormalities are found, a biopsy sample can be taken.
- Bone Marrow Aspiration and Biopsy. This test is performed when there is a suspicion of blood cancers like leukemia, lymphoma, or multiple myeloma. A small amount of bone marrow is removed from the hip bone using a needle to analyze the blood cells under a microscope.
- Mammogram. A mammogram is a specialized X-ray for examining breast tissue. It is commonly used for screening and detecting breast cancer at an early stage. If an abnormality is detected, additional tests such as an ultrasound or biopsy may be needed.
- Pap Smear and HPV Testing. These tests are used for detecting cervical cancer. A Pap smear involves collecting cells from the cervix to check for abnormalities, while HPV testing detects the presence of the human papillomavirus, which can cause cervical cancer.
- Colonoscopy. Colonoscopy involves inserting a long, flexible tube with a camera into the rectum to examine the colon and rectum for abnormalities or polyps. If suspicious growths are found, tissue samples can be collected for biopsy. It is a key diagnostic tool for colorectal cancer.
- Genetic Testing. Genetic testing is sometimes recommended for individuals with a family history of certain cancers, such as breast or ovarian cancer. It identifies mutations in genes like BRCA1 and BRCA2 that increase the risk of developing specific cancers. Genetic testing can guide both diagnosis and preventive measures.
- Cytology Tests. Cytology tests, like the examination of sputum or urine, are used to detect cancer cells in body fluids. For example, sputum cytology can help identify lung cancer, while urine cytology is used for bladder cancer.
- Lumbar Puncture (Spinal Tap). A lumbar puncture involves collecting cerebrospinal fluid (CSF) from the lower back to check for cancer cells or other abnormalities. It is commonly used when there is a suspicion of cancers affecting the central nervous system, such as lymphoma or leukemia.
These diagnostic procedures provide critical information that helps doctors determine the presence, type, stage, and spread of cancer, as well as the most appropriate treatment options. Early detection through these methods can significantly improve the chances of successful treatment and recovery.
Complications of Untreated Cancer
When cancer is left untreated, it can lead to various serious and potentially life-threatening complications. These complications often depend on the type of cancer, the affected organ, and the extent of its spread. Here are some common complications that may arise from untreated cancer:
- Metastasis. One of the most dangerous complications of untreated cancer is metastasis, which is when cancer cells spread from their original location to other parts of the body, such as the bones, liver, lungs, or brain. Once cancer spreads, it becomes more challenging to treat and often requires more aggressive therapies. Metastatic cancer can severely impact the function of the organs it spreads to, leading to further complications.
- Organ Failure. As cancer progresses, it can impair the normal function of the organs it affects. For instance, liver cancer can eventually lead to liver failure, while lung cancer may cause respiratory failure. This occurs because the cancerous growths take up space and resources that the organ needs to function properly. Eventually, the organ can no longer perform its essential roles, which can be fatal.
- Severe Pain. As tumors grow, they can press on nerves, bones, or other tissues, leading to significant pain. Cancers that spread to the bones, such as breast or prostate cancer, are particularly known for causing severe bone pain. Pain management becomes more difficult as the cancer advances, and untreated pain can severely impact the quality of life.
- Anemia and Fatigue. Many cancers affect the bone marrow, where blood cells are produced, leading to anemia (a reduction in red blood cells). This results in chronic fatigue, weakness, and shortness of breath. Even cancers that do not directly involve the bone marrow can cause fatigue through inflammation, nutritional deficiencies, and the overall strain of fighting the disease.
- Cachexia (Severe Weight Loss). Untreated cancer can lead to cachexia, a syndrome characterized by severe weight loss, muscle wasting, and loss of appetite. Cachexia is common in advanced stages of cancer and is not simply a result of poor nutrition but rather a metabolic condition where the body breaks down muscle and fat. This condition can weaken the body significantly and reduce the patient’s ability to tolerate treatment.
- Infections. Cancer, particularly blood cancers like leukemia or lymphoma, can weaken the immune system, making the body more susceptible to infections. Tumors that block the respiratory or digestive tracts can also create a breeding ground for bacteria, increasing the risk of pneumonia or sepsis. Infections in an immunocompromised patient can be more difficult to treat and can lead to severe complications.
- Blood Clots. Cancer increases the risk of developing blood clots, such as deep vein thrombosis (DVT) or pulmonary embolism (PE). This is because tumors can produce substances that cause the blood to clot more easily. Blood clots can be life-threatening if they travel to the lungs, heart, or brain, leading to conditions like stroke or heart attack.
- Fluid Accumulation. Certain cancers can cause fluid buildup in different parts of the body, such as:
- Ascites: Fluid buildup in the abdomen, often seen in liver or ovarian cancer, leading to swelling and discomfort.
- Pleural Effusion: Fluid accumulation in the space around the lungs, causing difficulty breathing and chest pain.
- Pericardial Effusion: Fluid buildup around the heart, which can interfere with heart function and lead to a condition called cardiac tamponade, a medical emergency.
- Neurological Issues. Cancers that spread to the brain or spinal cord can cause a range of neurological problems, including seizures, headaches, vision changes, and difficulty walking or speaking. Brain metastases can significantly impair cognitive function and can cause personality changes or loss of motor skills.
- Bleeding and Hemorrhage. Some cancers, particularly those that affect the digestive tract or blood, can lead to severe bleeding. Tumors can erode blood vessels, causing internal bleeding, which may appear as blood in the stool or vomit. In advanced stages, cancer can cause spontaneous bleeding in various parts of the body, which may require emergency medical intervention.
- Emotional and Mental Health Challenges. Untreated cancer can have a profound impact on a person’s mental and emotional well-being. The fear, uncertainty, and physical suffering associated with cancer can lead to depression, anxiety, and a sense of hopelessness. This emotional burden can affect not only the patient but also their loved ones and caregivers.
Addressing cancer at its earliest stage offers the best chance for effective treatment and avoiding these serious complications. Regular check-ups, early detection, and timely intervention can significantly improve outcomes for individuals facing a cancer diagnosis.
Causes of Cancer

Cancer can develop due to various factors that lead to abnormal cell growth and damage to the body’s cells. Here are some of the primary causes of cancer:
- Smoking Smoking contains a host of harmful chemicals like nicotine, tar, and benzene that can cause significant damage to the cells lining the lungs, mouth, and throat. These chemicals are known carcinogens that can trigger mutations in the cells, leading to lung cancer, oral cancer, and other cancers in the respiratory system. Additionally, secondhand smoke poses risks to those around smokers, increasing their likelihood of developing cancer as well.
- Exposure to Carcinogens Carcinogens are substances that have been identified to promote or facilitate the development of cancer. These include certain industrial chemicals, asbestos, formaldehyde, benzene, and even UV radiation from the sun. When the body is repeatedly exposed to these harmful agents, the DNA within cells can become damaged, leading to mutations that can evolve into cancer over time.
- Excessive Alcohol Consumption Chronic alcohol consumption is linked to a higher risk of several types of cancer, including liver cancer, esophageal cancer, throat cancer, and cancers of the mouth. Alcohol can irritate the tissues of these areas and lead to changes that make them more susceptible to developing cancerous cells. In the liver, alcohol overuse can cause cirrhosis, a condition that significantly increases the risk of liver cancer.
- Obesity Being overweight or obese can alter the body’s metabolism and hormone levels, contributing to chronic inflammation. This environment can foster cell growth, including that of cancer cells. Obesity is specifically associated with an increased risk of breast cancer (in post-menopausal women), colorectal cancer, pancreatic cancer, and kidney cancer.
- Infections Certain infections can directly contribute to cancer development. For example, viruses like human papillomavirus (HPV) can cause cervical cancer, while Hepatitis B and C infections are known risk factors for liver cancer. The inflammation and cellular changes caused by these infections can lead to cancerous transformations over time.
- Radiation Exposure Exposure to high levels of radiation, such as from nuclear power accidents or excessive exposure to radiation therapy, can damage the DNA in cells. This can lead to various cancers, including leukemia and thyroid cancer. Prolonged exposure to ultraviolet (UV) rays from the sun is a common cause of skin cancers like melanoma.
- Genetic Mutations Some people inherit mutations in specific genes that make them more prone to cancer. For instance, mutations in the BRCA1 and BRCA2 genes are linked to a higher risk of breast and ovarian cancer. While not all cancers are inherited, these genetic predispositions can make a person more susceptible when combined with environmental factors.
- Hormonal Changes Hormones can play a role in the development of certain cancers. For example, high levels of estrogen over prolonged periods can increase the risk of breast cancer and uterine cancer. Some hormonal medications, like hormone replacement therapy (HRT), can also contribute to cancer risk, particularly when used long-term.
Understanding these causes is crucial for taking preventive steps and making lifestyle changes that can reduce the likelihood of developing cancer. It’s always advisable to consult with healthcare professionals about reducing risk factors, especially if there is a family history of cancer or other contributing factors.
Treatment Options for Cancer
Specialists who focus on diagnosing and treating cancer are called oncologists. They study this complex disease and provide guidance on the most suitable prevention and treatment methods. The type of treatment that oncologists recommend depends on several factors: the specific type of cancer, the part of the body affected, the patient’s overall health condition, and the stage of the cancer.

Here are some of the primary cancer treatments:
- Chemotherapy. Chemotherapy uses powerful drugs to target and kill cancer cells. It is effective in shrinking tumors and reducing the spread of cancer throughout the body. However, chemotherapy can have significant side effects, such as hair loss, fatigue, nausea, and a weakened immune system. These side effects occur because chemotherapy can also damage healthy cells, particularly those that divide quickly, like those in the bone marrow, digestive system, and hair follicles.
- Radiation Therapy. This treatment involves the use of high doses of radiation to destroy cancer cells and shrink tumors. The radiation targets the DNA of cancer cells, damaging them so that they cannot grow or divide. It can be delivered externally using a machine (external beam radiation) or internally through radioactive substances placed near the tumor (brachytherapy). While effective, radiation therapy may also harm nearby healthy tissues, leading to side effects such as skin irritation, fatigue, and localized pain.
- Surgery. Surgery is often used to remove tumors and, in some cases, cancer-affected lymph nodes to prevent the spread of the disease. The extent of the surgery depends on the location and size of the tumor. For early-stage cancers, surgery can sometimes be curative if the entire tumor is removed. For advanced-stage cancers, it may be combined with other treatments like chemotherapy or radiation therapy to improve outcomes.
- Stem Cell Transplant. This procedure is typically used for blood-related cancers, such as leukemia and lymphoma. It involves transplanting healthy blood-forming stem cells into the patient’s body to replace damaged or destroyed bone marrow. There are two main types: autologous (using the patient’s own cells) and allogeneic (using cells from a donor). Stem cell transplants allow for higher doses of chemotherapy and radiation to be used, which can be more effective against certain cancers.
- Immunotherapy. Immunotherapy strengthens the body’s immune system to better recognize and fight cancer cells. Unlike other treatments, immunotherapy focuses on empowering the body’s natural defenses. It includes approaches such as:
- Checkpoint Inhibitors. These drugs help the immune system recognize and attack cancer cells by blocking proteins that prevent immune responses.
- Adoptive Cell Transfer. This involves extracting immune cells from a patient, modifying or enhancing them in the lab, and then reintroducing them into the body to attack cancer cells.
- Cancer Vaccines. These vaccines work by stimulating the immune system to target specific cancer antigens, helping to prevent the growth and spread of cancer cells.
In addition to these primary treatments, some patients may also benefit from targeted therapy. This treatment specifically attacks the genes, proteins, or tissue environment that contributes to cancer growth. Targeted therapies often have fewer side effects compared to traditional chemotherapy because they focus more precisely on cancer cells.
Complementary Treatments and Supportive Care
- Hormone Therapy. For cancers that are sensitive to hormones, like certain types of breast and prostate cancer, hormone therapy can help to slow or stop their growth. This treatment involves blocking the body’s natural hormones or reducing their levels.
- Pain Management and Palliative Care. Managing symptoms and maintaining the patient’s comfort is a critical part of cancer care, especially for advanced stages. This can include pain relievers, anti-nausea medications, and counseling to support the patient’s mental and emotional well-being.
Choosing the Right Treatment
Selecting the appropriate treatment plan involves careful discussion between the patient and their oncology team. Factors such as potential side effects, the likelihood of success, and the impact on quality of life are all considered. In some cases, a combination of treatments may be recommended to achieve the best possible outcome. The goal is to either eliminate the cancer, control its spread, or relieve symptoms to enhance the patient’s quality of life.
Prevention of Cancer

While there is no guaranteed way to prevent cancer entirely, there are several lifestyle changes and practices that can significantly reduce the risk of developing it. Here are some essential tips to help lower your risk:
- Quit Smoking. It is crucial not only to stop smoking but also to avoid exposure to secondhand smoke. Cigarettes contain numerous harmful chemicals that can cause lung cancer and other types of cancer, such as those affecting the mouth, throat, and esophagus. Avoiding areas where people smoke can also protect you from the dangers of secondhand smoke.
- Choose a Healthy Diet. A diet rich in fruits, vegetables, whole grains, and lean proteins can help boost the immune system and provide antioxidants that combat cell damage. Some types of fruits and vegetables contain compounds that have been shown to help prevent the growth of cancer cells. Consider including foods like leafy greens, berries, and foods rich in vitamins A, C, and E.
- Engage in Regular Exercise. Studies have shown that physical activity can help reduce the risk of certain cancers. Aim for at least 30 minutes of exercise most days of the week, whether it’s walking, running, cycling, or any activity that keeps you moving. Regular exercise helps maintain a healthy weight and improves overall immune function.
- Maintain a Healthy Weight. Obesity is a significant risk factor for various types of cancer, including breast, colon, and kidney cancer. Strive to maintain a weight that is appropriate for your height and age by combining a balanced diet with regular exercise. Consult a healthcare professional to determine a healthy weight range for you.
- Limit Sun Exposure. Ultraviolet (UV) rays from the sun are a major cause of skin cancer, including melanoma. To protect yourself, avoid excessive sun exposure, especially between 10 AM and 4 PM when UV rays are strongest. Wear protective clothing, use a wide-brimmed hat, and apply sunscreen with at least SPF 30 on exposed skin. Even on cloudy days, UV rays can still penetrate and cause damage.
- Reduce Alcohol Consumption. Drink alcoholic beverages in moderation to lower your risk of developing cancers related to alcohol consumption, such as liver, breast, and esophageal cancer. For those who choose to drink, it is recommended to limit alcohol intake to one drink per day for women and up to two drinks per day for men.
- Get Vaccinated. Certain infections can increase cancer risk, particularly in women. Vaccines such as the human papillomavirus (HPV) vaccine can help prevent types of cervical cancer and other cancers caused by HPV. The hepatitis B vaccine can also reduce the risk of liver cancer caused by hepatitis infections.
- Undergo Regular Cancer Screenings. Early detection through regular screening tests can identify cancer at its initial stages when it is most treatable. Depending on age, gender, and family history, doctors may recommend screenings such as mammograms, colonoscopies, Pap smears, or low-dose CT scans for lung cancer. Following your doctor’s advice for screenings can make a significant difference in early detection and successful treatment.
Adopting these preventive measures can greatly reduce your cancer risk and improve your overall health. Regular check-ups and open communication with your healthcare provider are also crucial for maintaining a proactive approach to your health.
Risk Factors for Lung Disease
While anyone can develop cancer, certain factors can increase a person’s likelihood of developing the disease. Here are some of the main risk factors:
- Age Cancer risk increases significantly with age. The majority of cancer diagnoses occur in people aged 55 and older. Over time, cells accumulate damage, which can lead to mutations that trigger cancer. Although older adults are more susceptible, certain types of cancer can affect younger individuals, including children and adolescents.
- Family History Genetics can play a role in cancer development. If a close family member has had cancer, particularly at an early age, it could indicate a genetic predisposition. For example, mutations in the BRCA1 or BRCA2 genes can increase the risk of breast and ovarian cancers. In such cases, genetic counseling and testing can help assess the risk level.
- Lifestyle Choices Certain lifestyle habits are known to increase cancer risk:
- Smoking and excessive alcohol consumption are significant risk factors for various cancers, such as lung, throat, liver, and oral cancers.
- Lack of physical activity and poor diet can contribute to obesity, which is linked to a higher risk of cancers like breast, colorectal, and kidney cancers.
- Unsafe sexual practices, which can lead to infections like HPV, can increase the risk of cervical and other cancers.
- Obesity Being overweight or obese is associated with a higher risk of several types of cancer, including breast (particularly in postmenopausal women), colorectal, pancreatic, and endometrial cancers. Excess body weight can cause chronic inflammation, alter insulin levels, and influence hormone production, all of which can encourage the growth of cancer cells.
- Exposure to Carcinogens Working in environments with chemicals such as asbestos, benzene, formaldehyde, or exposure to secondhand smoke can increase cancer risk. Long-term exposure to polluted air or industrial chemicals can also contribute to lung cancer and other forms of the disease.
- Weakened Immune System Individuals with weakened immune systems, whether due to conditions like HIV/AIDS or immunosuppressive medications (such as those used after organ transplants), are at a higher risk for certain cancers. This is because a weakened immune system is less capable of detecting and destroying abnormal cells.
- Chronic Infections Certain infections can elevate cancer risk. For example:
- Hepatitis B or C increases the risk of liver cancer.
- Human papillomavirus (HPV) is a major risk factor for cervical cancer and cancers of the throat.
- Helicobacter pylori infection is associated with an increased risk of stomach cancer.
- Radiation Exposure Repeated exposure to ultraviolet (UV) radiation from the sun significantly increases the risk of skin cancers like melanoma. Additionally, exposure to ionizing radiation, such as from radiation therapy or accidental exposure (like nuclear accidents), can increase the risk of cancers such as thyroid cancer and leukemia.
- Occupational Hazards Certain professions expose individuals to industrial chemicals, asbestos, pesticides, or radiation, which can heighten the risk of developing cancer. For instance, those working in mines or construction may be at a higher risk of lung cancer due to exposure to dust and harmful fumes.
- Hormonal Factors Prolonged exposure to estrogen (whether naturally occurring or through hormone replacement therapy) can increase the risk of breast and uterine cancers. Certain birth control methods have also been associated with a slight increase in the risk of some cancers.
- Diet A diet high in processed meats, red meat, and saturated fats, as well as low in fiber, fruits, and vegetables, can increase the risk of cancers such as colorectal cancer. A balanced diet rich in antioxidants and nutrients helps to protect cells from damage.
Understanding these risk factors can help guide lifestyle changes and medical decisions to reduce the likelihood of developing cancer. For those with a family history or other significant risk factors, early screening and regular check-ups with a healthcare provider can be crucial for early detection and prevention.
Cancer FAQs
Here are some frequently asked questions (FAQs) about cancer, aimed at providing a better understanding of this condition:
- What is cancer?
Cancer is a condition characterized by the uncontrolled growth and spread of abnormal cells in the body. These cells can invade and damage surrounding tissues, potentially spreading to other parts of the body through the bloodstream or lymphatic system.
- What causes cancer?
Cancer can be caused by a variety of factors, including genetic mutations, exposure to carcinogens (such as tobacco smoke, certain chemicals, and radiation), lifestyle choices (like diet and physical activity), and infections. Sometimes, the exact cause of cancer in an individual cannot be determined.
- Can cancer be inherited?
Yes, some types of cancer can be inherited, meaning they run in families. For example, breast cancer, ovarian cancer, and colorectal cancer can have hereditary links. Genetic mutations passed from parents to their children can increase the risk of developing these cancers. Genetic testing may help identify such risks.
- What are the early signs of cancer?
Early signs of cancer can vary depending on the type and location of the cancer. Common early symptoms include unexplained weight loss, persistent fatigue, unusual lumps or swelling, changes in bowel or bladder habits, and unexplained bleeding. If you experience persistent symptoms, consult a healthcare professional.
- How is cancer diagnosed?
Cancer is diagnosed using various methods such as imaging tests (e.g., CT scans, MRIs, X-rays), biopsies (removal of a tissue sample for analysis), blood tests, and endoscopy procedures. The choice of diagnostic method depends on the suspected type of cancer and its location.
- Is cancer treatable?
Yes, many types of cancer are treatable, especially when detected early. Treatment options include chemotherapy, radiation therapy, surgery, immunotherapy, and targeted therapy. The effectiveness of treatment depends on factors like the type of cancer, its stage, and the patient’s overall health.
- What are the side effects of cancer treatments?
Cancer treatments can have side effects that vary depending on the type of treatment. Common side effects include fatigue, nausea, hair loss, loss of appetite, skin changes, and an increased risk of infections. Oncologists can recommend supportive therapies to help manage these side effects.
- Can lifestyle changes reduce the risk of cancer?
Yes, adopting a healthy lifestyle can reduce the risk of developing cancer. This includes quitting smoking, eating a balanced diet rich in fruits and vegetables, maintaining a healthy weight, engaging in regular physical activity, reducing alcohol consumption, and protecting the skin from excessive sun exposure.
- How often should I get screened for cancer?
Screening recommendations vary based on age, gender, family history, and risk factors. For example, women over 40 are often advised to get regular mammograms for breast cancer, while colonoscopies are recommended for adults over 50. Consult your healthcare provider for personalized screening guidelines.
- Is cancer always fatal?
No, cancer is not always fatal. Many types of cancer can be successfully treated, especially when caught early. Advances in cancer research have led to better treatments, which can result in complete remission or long-term management of the disease. Early detection and proper treatment significantly improve survival rates.
- Can stress cause cancer?
There is no direct evidence that stress causes cancer. However, chronic stress can weaken the immune system, which may indirectly affect the body’s ability to fight off illnesses, including cancer. Managing stress through relaxation techniques and a healthy lifestyle can support overall well-being.
- What should I do if I suspect I have cancer?
If you notice unusual symptoms or changes in your body that persist, consult a healthcare professional as soon as possible. Early diagnosis is key to effective treatment. A doctor can conduct the necessary tests to determine if your symptoms are related to cancer or another health condition.
These FAQs aim to provide a basic understanding of cancer. If you have further concerns or need specific information, always consult with a healthcare professional or oncologist.