Summary
Among all cancer types, lung cancer is the leading cause of cancer-related deaths in the Philippines. Statistics show that three out of ten Filipinos smoke, contributing to the high prevalence of this disease. However, even non-smokers are at risk of developing lung cancer. Former Senator Miriam Defensor-Santiago, a notable figure who was diagnosed with lung cancer despite never having smoked, is one example. Her case underscores the dangers of secondhand smoke exposure, highlighting that inhaling smoke from others’ cigarettes can also pose significant risks.
The primary symptoms of lung cancer are often similar to those of other respiratory conditions, making early detection challenging. Common symptoms include a persistent cough, coughing up blood-tinged phlegm, shortness of breath, and extreme fatigue. As lung cancer progresses to advanced stages, additional symptoms may appear, such as lumps near the shoulder area, yellowing of the skin (jaundice), bone pain, and numbness.
If someone experiences these primary symptoms, it is crucial to seek medical consultation promptly for appropriate treatment. Lung cancer treatment options include surgery, chemotherapy, radiation therapy, and targeted treatments. Early diagnosis and timely treatment are essential for improving survival outcomes and managing the disease.
Table of Contents
Symptoms of Lung Cancer

To prevent lung cancer from worsening, it’s essential to consult a doctor promptly if experiencing any of the following symptoms:
- Persistent cough. A cough that doesn’t go away and may gradually worsen.
- Coughing up blood. Even small amounts of blood in the phlegm can indicate a serious issue.
- Hoarseness. Changes in the voice, especially if it becomes persistently hoarse.
- Shortness of breath. Difficulty breathing or shortness of breath, even during mild activities.
- Chest pain. Discomfort or pain in the chest that may worsen with deep breaths, coughing, or laughing.
- Sudden weight loss. Unexplained and rapid weight loss.
- Extreme fatigue. Persistent weakness and lack of energy, impacting daily activities.
These are primary symptoms of lung cancer. As the disease progresses to advanced stages, additional symptoms may appear, including:
- Lumps near the shoulder. The appearance of lumps or swelling in areas around the shoulders or collarbone.
- Yellowing of the skin (jaundice). This can indicate the spread of cancer to the liver.
- Bone and joint pain. Pain that radiates to the bones or joints, often felt in the back or hips.
- Numbness. Tingling or numbness in the limbs, which may indicate nerve involvement.
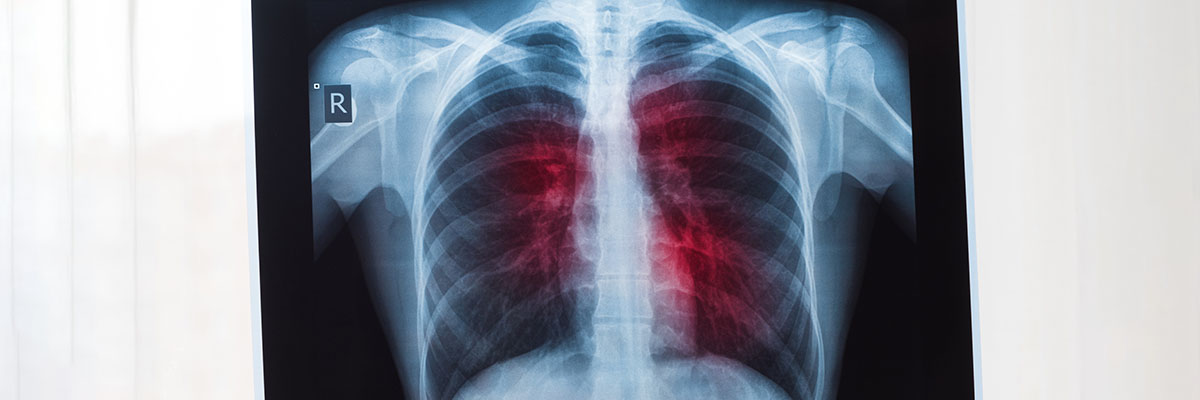
Diagnosing lung cancer can be challenging because its early symptoms resemble those of other respiratory illnesses. To confirm lung cancer, patients need to undergo various diagnostic tests, such as X-rays, sputum cytology (analyzing phlegm for cancer cells), and a biopsy (examining lung tissue for cancer cells). Early diagnosis through these tests is crucial for determining the most effective treatment options.
Types of Lung Cancer
Lung cancer is divided into two main types: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
- Small cell lung cancer (SCLC). SCLC accounts for approximately 15% of all lung cancer cases. While it is less common, it is considered the more aggressive type of lung cancer, often spreading rapidly and showing symptoms only in its advanced stages. Smoking is the primary cause of SCLC, making it highly preventable through lifestyle changes.
- Non-small cell lung cancer (NSCLC). NSCLC is the most prevalent form of lung cancer, making up about 85% of cases. NSCLC itself is divided into three main subtypes:
- Adenocarcinoma. Adenocarcinoma is the most common subtype of NSCLC and can occur in both smokers and non-smokers, although smoking is a significant risk factor. These tumors typically develop on the outer edges or sides of the lungs. Compared to other lung cancer types, adenocarcinoma has a higher chance of being treatable and has a relatively better prognosis.
- Squamous cell carcinoma. This type of NSCLC originates in the central part of the lungs, often near the bronchial tubes. As squamous cell carcinoma progresses, it tends to spread to nearby lymph nodes, which are essential for fighting infections and illnesses. When cancer reaches the lymph nodes, it weakens the immune system, making the patient more susceptible to other health issues.
- Large cell carcinoma. Similar to adenocarcinoma, large cell carcinoma tumors develop on the outer regions of the lungs. However, the tumors are typically larger and grow and spread quickly. Large cell carcinoma can also spread to the lymph nodes, leading to rapid disease progression.
Understanding the specific type of lung cancer is essential for determining the best treatment approach and improving patient outcomes. Each type and subtype has unique characteristics, and early detection plays a crucial role in effective treatment and potential recovery.
Diagnostic Procedures for Lung Cancer

Diagnosing lung cancer involves a series of tests to accurately detect, confirm, and assess the extent of the disease. Here are the primary diagnostic procedures used to evaluate lung cancer:
- Medical history and physical examination. The doctor will review the patient’s medical history, focusing on symptoms like persistent cough, shortness of breath, and unexplained weight loss. A physical exam helps assess overall health and identify signs of lung issues or cancer-related symptoms.
- Imaging tests. Imaging tests are crucial in diagnosing lung cancer and assessing its spread:
- Chest X-ray. A chest X-ray is often the first test done to identify abnormal masses or nodules in the lungs.
- CT (Computed Tomography) scan. CT scans provide more detailed images of the lungs, showing the size, shape, and location of tumors. CT scans can also detect smaller nodules that might not appear on an X-ray.
- PET (Positron Emission Tomography) scan. PET scans are used to determine if cancer has spread beyond the lungs. A small amount of radioactive sugar is injected into the bloodstream, highlighting cancerous areas on the scan.
- Sputum cytology. This test involves examining a sample of mucus (sputum) from a patient’s cough under a microscope. It can detect cancer cells in patients with tumors close to the airways, especially in cases where a persistent cough produces phlegm.
- Bronchoscopy. During a bronchoscopy, a thin, flexible tube with a camera is inserted through the nose or mouth and into the lungs. This allows the doctor to view and take samples from suspicious areas in the airways and lungs.
- Biopsy. A biopsy involves collecting a sample of lung tissue to confirm the presence of cancer cells:
- Needle biopsy. Using CT or ultrasound guidance, a doctor inserts a needle through the chest wall to obtain a tissue sample from the lung.
- Surgical biopsy. In some cases, a small surgical procedure is required to access and remove tissue from the lung.
- Molecular and genetic testing. If lung cancer is confirmed, molecular testing may be performed on the tissue sample to check for specific genetic mutations or biomarkers. These tests help determine if targeted therapy or immunotherapy would be effective treatments for the patient.
- Mediastinoscopy. A mediastinoscopy is used to examine and biopsy lymph nodes in the center of the chest to see if cancer has spread. This procedure is done under general anesthesia, with a small incision made at the base of the neck.
- Blood tests. While blood tests alone cannot diagnose lung cancer, they provide information on overall health and organ function, which can impact treatment options. Blood tests can also detect biomarkers that may indicate cancer presence.
These diagnostic procedures, when combined, offer a comprehensive assessment of lung cancer, confirming its presence, type, and stage. Early and accurate diagnosis is essential for developing a targeted treatment plan and improving patient outcomes.
Complications of Untreated Lung Cancer
If left untreated, lung cancer can lead to severe and life-threatening complications, affecting both the lungs and other parts of the body. Here are some of the main complications associated with untreated lung cancer:
- Respiratory failure. As tumors grow and spread within the lungs, they block airways, making it difficult to breathe. This can lead to respiratory failure, where the lungs are unable to supply enough oxygen to the body, resulting in serious health risks and potential hospitalization.
- Metastasis to other organs. Lung cancer often spreads (metastasizes) to other areas of the body, including the brain, liver, adrenal glands, and bones. When cancer spreads to these organs, it disrupts their function, leading to a range of additional symptoms, such as seizures, jaundice, severe pain, and neurological issues, making treatment more challenging.
- Fluid buildup in the chest (pleural effusion). Lung cancer can cause fluid to accumulate between the layers of tissue surrounding the lungs (the pleura). This fluid buildup can cause chest pain, shortness of breath, and make breathing uncomfortable. Recurrent pleural effusion often requires draining or other treatments to manage symptoms.
- Chronic pain. Advanced lung cancer often causes severe pain, especially if it spreads to bones or affects nerve endings. Pain can be constant and debilitating, impacting a person’s ability to perform daily activities and severely affecting quality of life.
- Blood clots (thrombosis). Cancer, especially lung cancer, increases the risk of blood clots, which can occur in the legs (deep vein thrombosis) or lungs (pulmonary embolism). Blood clots are serious complications that can lead to additional respiratory issues, heart strain, or even sudden death if not treated.
- Severe weight loss and cachexia. Lung cancer frequently leads to significant weight loss and cachexia (a wasting syndrome). This condition results from cancer’s impact on the body’s metabolism and nutrient absorption, leading to fatigue, weakness, and an overall decline in health.
- Infections (pneumonia and bronchitis). Lung cancer weakens lung tissue and impairs immune response, making patients more susceptible to infections like pneumonia and bronchitis. These infections can worsen respiratory symptoms and lead to further health complications if untreated.
- Psychological and emotional distress. Untreated lung cancer often results in increased anxiety, depression, and emotional distress due to persistent symptoms and declining health. This psychological burden can impact overall quality of life and make it difficult for patients to manage daily life.
These complications underscore the importance of early detection and timely treatment for lung cancer. Proper medical intervention can help control cancer progression, reduce the risk of complications, and improve the chances of a better quality of life.
Causes of Lung Cancer
The direct causes of lung cancer involve cellular changes and damage within the lungs, often due to the intake or exposure to harmful substances that lead to cell mutation and tumor formation. The primary causes include:
- Toxic chemical exposure from smoking. Smoking introduces harmful chemicals, such as tar, benzene, and formaldehyde, directly into the lungs. These chemicals damage lung cells at the DNA level, leading to mutations. Over time, the accumulation of damaged cells triggers uncontrollable cell growth, resulting in lung cancer. Smoking remains the single most direct cause of lung cancer.
- Cellular mutation from secondhand smoke exposure. Inhaling secondhand smoke causes the same cellular damage in non-smokers as it does in smokers. Prolonged or frequent exposure to these toxic particles can initiate mutations in healthy lung cells, leading to the same cancerous development seen in smokers.
- Asbestos fiber inhalation. When asbestos fibers are inhaled, they lodge deep within the lung tissue, where they irritate cells and create inflammation. Over time, this chronic irritation damages lung cell DNA, which can lead to cancerous changes, particularly in people who have worked with asbestos for extended periods.
- Radon-induced DNA damage. Radon gas, which is emitted from soil and rock, releases radiation that, when inhaled, directly damages the DNA of lung cells. This radiation exposure is a significant cause of lung cancer, especially in areas with high radon levels, as it breaks down lung cell structures and leads to tumor formation.
- Continuous inflammation from air pollution exposure. Prolonged exposure to polluted air introduces harmful particles into the lungs. These particles cause ongoing inflammation and cellular damage. The buildup of these particles and the resulting chronic irritation can lead to cellular mutations in the lung tissue, eventually resulting in cancer.
- Genetic predisposition and cellular vulnerability. Some individuals inherit genes that make their lung cells more susceptible to damage and mutation. This genetic susceptibility can make their lung cells more vulnerable to changes in response to toxins, even at lower exposure levels, leading to an increased chance of cancerous growth.
Understanding these direct causes highlights the importance of reducing exposure to known carcinogens and managing genetic predispositions through preventive healthcare. These measures can help reduce the likelihood of the cellular mutations that directly cause lung cancer.
Prevention of Lung Cancer

According to the Department of Health, lung cancer is one of the most common lifestyle-related diseases, meaning it often develops due to unhealthy lifestyle choices. To help prevent lung cancer, consider the following steps:
- Avoid smoking. As mentioned earlier, 90% of lung cancer cases are directly caused by smoking. If you smoke, gradually reduce the habit until you quit entirely. Quitting smoking significantly lowers the risk of lung cancer by preventing exposure to the harmful chemicals in tobacco.
- Cover your nose while traveling. When in polluted or smoky areas, make it a habit to cover your nose. Remember, it’s not only cigarette smoke that poses a risk; exhaust fumes from vehicles and the smell of burning trash contain carcinogens that can harm lung tissue.
- Wear a face mask when outdoors or at work. If you work in mining, construction, or other high-risk environments, always wear a face mask to protect yourself from direct inhalation of carcinogens like asbestos fibers and radon gas. These substances can directly damage lung cells, increasing cancer risk over time.
- Eat plenty of fruits and vegetables. Fruits and vegetables are rich in antioxidants, which help protect healthy cells from damage caused by carcinogens. Foods high in antioxidants—such as berries, apples, nuts, broccoli, and carrots—are especially beneficial in supporting lung health.
- Exercise regularly. Daily exercise, such as walking, jogging, swimming, or going to the gym, helps flush out toxins from the body. Physical activity also improves blood circulation and promotes healthy lung function, supporting the body’s ability to maintain clean and healthy lungs.
- See a doctor if you notice any unusual respiratory symptoms. A persistent cough, shortness of breath, or chest pain can be early signs of lung cancer. Early detection is crucial for effective treatment, as lung cancer is more treatable when diagnosed in its early stages.
By adopting these preventive measures, individuals can significantly reduce their risk of developing lung cancer. Early lifestyle adjustments and regular checkups can contribute to better long-term health and increase the chances of early intervention if any issues arise.
Risk Factors for Lung Cancer

According to the Lung Cancer Alliance, the following primary factors significantly increase the likelihood of developing lung cancer:
- Age between 55 and 80 years. Lung cancer risk rises with age, particularly among those within this age range.
- Smoking. Smoking remains the most direct cause of lung cancer, especially in individuals who smoke heavily or have smoked for many years.
- Heavy smoking history. People who smoke two packs of cigarettes or around 30 cigarettes daily are at extremely high risk. Even after quitting, they may still develop lung cancer, as carcinogens remain in the body and continue to affect cellular health.
In addition to these primary factors, there are other factors that also contribute to the risk of developing lung cancer:
- Family history. If lung cancer is common in your family, your genetic predisposition increases your risk, especially without preventive measures.
- Occupational exposure (such as mining and military work). Occupations involving exposure to hazardous materials like radon gas and asbestos carry a high risk of inhaling carcinogens that damage lung tissue.
- Marijuana use. Studies show that inhaling smoke from burned marijuana contains carcinogens similar to those found in cigarette smoke, which can harm lung cells.
- Use of vape or e-cigarettes. Although research is still ongoing, vaping liquids often contain nicotine and other chemicals that can damage lung health, potentially increasing cancer risk.
- Pre-existing lung conditions. Common lung issues, such as asthma and chronic bronchitis, may also increase the risk of lung cancer. Research indicates a 50-100% higher likelihood of developing lung cancer in individuals with other lung conditions.
Understanding these factors can help people make informed decisions about their health and take preventive steps. Avoiding smoking, limiting exposure to known carcinogens, and managing any existing lung conditions are essential strategies to lower lung cancer risk.
Lung Cancer FAQs
These FAQs provide general information about lung cancer. For personal advice and treatment options, consult a healthcare provider.
- What is lung cancer?
Lung cancer is a type of cancer that starts in the lungs. It occurs when abnormal cells in the lungs grow uncontrollably, forming tumors that can interfere with lung function and may spread to other parts of the body. - What causes lung cancer?
The primary cause of lung cancer is smoking, responsible for nearly 90% of cases. Other causes include exposure to secondhand smoke, radon gas, asbestos, air pollution, and genetic factors. In some cases, lung cancer can develop in non-smokers due to these other factors. - What are the types of lung cancer?
There are two main types: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). SCLC is less common but more aggressive, while NSCLC is more prevalent and has multiple subtypes, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. - Who is at risk for lung cancer?
Risk factors include smoking, secondhand smoke exposure, age (usually 55 and older), family history of lung cancer, exposure to radon or asbestos, and certain occupations (e.g., mining, construction). Even former smokers remain at higher risk due to long-term exposure to carcinogens. - What are the symptoms of lung cancer?
Common symptoms include a persistent cough, coughing up blood, chest pain, shortness of breath, unexplained weight loss, and fatigue. As lung cancer progresses, additional symptoms like bone pain and jaundice may appear if cancer spreads to other organs. - Can non-smokers get lung cancer?
Yes, non-smokers can develop lung cancer due to secondhand smoke, environmental factors like radon, exposure to carcinogens, or genetic predisposition. While non-smoker lung cancer is less common, it can still be severe. - How is lung cancer diagnosed?
Diagnostic tests include imaging (like X-rays, CT scans), sputum cytology (examining mucus for cancer cells), and biopsy (collecting lung tissue samples to confirm cancer). PET scans and MRIs may also be used to determine if cancer has spread. - How is lung cancer treated?
Treatment depends on the type and stage of cancer but may include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, and, in some cases, palliative care to manage symptoms. Early-stage cancer is often treated with surgery, while advanced cases may require a combination of therapies. - What is the survival rate for lung cancer?
Survival rates vary depending on cancer type, stage, and individual factors. Early-stage lung cancer has a higher survival rate when treated promptly, but advanced lung cancer has a lower survival rate. Advances in treatment have improved outcomes, especially with targeted and immunotherapies. - Can lung cancer be prevented?
Preventive measures include not smoking, avoiding secondhand smoke, testing for radon in homes, wearing protective gear if working with carcinogens, and maintaining overall lung health through exercise and a healthy diet. Avoiding known carcinogens and regular check-ups can also lower risk. - What should I do if I think I have symptoms of lung cancer?
If you have symptoms like a persistent cough, unexplained weight loss, or chest pain, consult a healthcare provider for evaluation. Early detection through medical consultation and testing is essential for effective treatment. - Can quitting smoking lower my lung cancer risk?
Yes, quitting smoking significantly reduces lung cancer risk. The longer you remain smoke-free, the more your risk declines, although former smokers are still at higher risk compared to never-smokers.