Summary
The liver plays a crucial role in the body, helping to ensure the proper functioning of the digestive system and various bodily processes. Like other organs, however, the liver can develop cancer.
Liver cancer occurs due to the uncontrolled growth of abnormal cells in the liver, which can damage the healthy liver cells and compromise its functions. Unfortunately, liver cancer is associated with a low survival rate among patients.
Several factors can increase the risk of developing liver cancer. These include cirrhosis, where scar tissue builds up in the liver, chronic infections such as hepatitis B and C, and conditions like diabetes.
Symptoms of liver cancer may include yellowing of the eyes and skin (jaundice), enlargement or swelling of the liver, and abdominal pain.
Treatment options typically involve surgery, radiation therapy, and chemotherapy.
Table of Contents
Symptoms of Liver Cancer

Liver cancer can develop quietly in its early stages, often showing minimal symptoms. However, as the disease progresses, several key signs may emerge. These include:
- Jaundice. A yellowing of the eyes and skin occurs when the liver fails to process bilirubin, leading to its accumulation in the body.
- Abdominal pain. Persistent pain, particularly in the upper right side of the abdomen, is common. The pain may extend to the back or right shoulder.
- Swelling or bloating. This can result from the enlargement of the liver (hepatomegaly) or fluid buildup in the abdomen (ascites).
- Unexplained weight loss. A sudden or unintentional drop in weight, without changes in diet or exercise, may occur.
- Fatigue. Chronic fatigue or weakness can be a significant symptom as the body expends energy combating the cancer.
- Nausea and vomiting. The body’s inability to effectively detoxify can lead to persistent nausea and episodes of vomiting.
- Loss of appetite. As liver function declines, digestive processes can become disrupted, reducing appetite.
- Dark urine and pale stools. Bilirubin buildup may also cause dark-colored urine and unusually light or chalky stools.
- Fever. Some patients with liver cancer experience frequent, unexplained fevers.
- General discomfort. A feeling of weakness or discomfort may persist, affecting the overall well-being of the patient.
Though these symptoms can be indicative of various liver-related issues, they should not be ignored. If these signs persist, seeking medical consultation is essential for early detection and effective treatment of liver cancer.
Types of Liver Cancer
There are four main types of liver cancer, each originating from different cells that form the liver. These primary liver cancers can develop either as a single tumor or in multiple areas of the liver simultaneously.
- Hepatocellular carcinoma (HCC). Also known as hepatoma, this is the most common type of liver cancer. It arises from hepatocytes, the primary liver cells responsible for processing nutrients. HCC may spread from the liver to nearby organs such as the pancreas, intestines, or stomach. This type of cancer is most commonly associated with those who have significant liver damage, often due to long-term alcohol abuse or chronic hepatitis infections (Hepatitis B and C).
- Cholangiocarcinoma. This form of cancer develops in the bile ducts, the channels that carry bile from the liver to the gallbladder and intestines. It accounts for about 10-20% of liver cancer cases. Bile duct cancer can be further classified into intrahepatic and extrahepatic types, depending on where it starts along the bile duct system.
- Liver angiosarcoma. A rare and aggressive type of liver cancer, angiosarcoma forms in the blood vessels of the liver. This cancer grows quickly and is difficult to detect in its early stages, which makes treatment challenging. Its aggressive nature often results in rapid spread before diagnosis.
- Hepatoblastoma. This is another rare form of liver cancer, but it primarily affects children, typically under the age of three. Hepatoblastoma has a high cure rate if detected early and treated effectively, often with surgery and chemotherapy.
While each type of liver cancer affects different cells and functions within the liver, the aggressive nature of the disease, particularly hepatocellular carcinoma, highlights the importance of early diagnosis and appropriate treatment.
Diagnostic Procedures for Liver Cancer

Diagnosing liver cancer involves a series of tests and evaluations to determine whether abnormal cell growth is present in the liver and to assess its stage. The following are common diagnostic procedures used to detect liver cancer:
- Blood Tests. Blood tests are typically the first step in diagnosing liver cancer. Doctors may check for abnormal levels of liver enzymes, including elevated levels of alpha-fetoprotein (AFP), a protein that is often higher in individuals with hepatocellular carcinoma.
- Imaging Tests. These are crucial for identifying the size, location, and extent of liver tumors. Common imaging tests include:
- Ultrasound. A non-invasive test that uses sound waves to create images of the liver. It can detect masses or abnormalities in the liver tissue.
- Computed Tomography (CT) Scan. CT scans provide detailed images of the liver, helping doctors assess the extent of the tumor and whether it has spread to other organs.
- Magnetic Resonance Imaging (MRI). MRIs use powerful magnets and radio waves to create detailed images of the liver, particularly useful for determining the type of liver tumor and its characteristics.
- Angiography. This test examines the blood vessels around the liver. A dye is injected into the bloodstream, and X-rays are used to see how blood flows through the liver, which helps identify abnormal blood flow patterns that may suggest cancer.
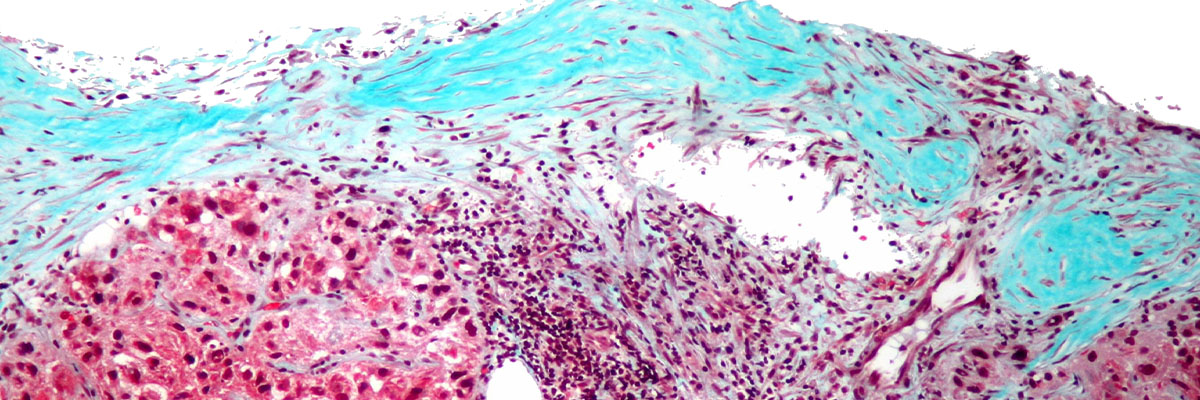
- Liver Biopsy. In cases where imaging tests suggest cancer, a liver biopsy may be performed. A small sample of liver tissue is removed using a thin needle inserted into the liver and is examined under a microscope to confirm the presence of cancerous cells. Although highly effective, a biopsy carries some risk of complications, such as bleeding or infection.
- Liver Function Tests. These tests assess how well the liver is working by measuring levels of enzymes, proteins, and bilirubin in the blood. These can help determine if the liver is damaged, although they are not specific for cancer diagnosis.
- Molecular Testing. In some cases, genetic and molecular tests may be performed to identify mutations or genetic markers in the tumor cells. This can help determine specific treatment options, such as targeted therapies.
- Positron Emission Tomography (PET) Scan. A PET scan involves injecting a small amount of radioactive sugar into the bloodstream. Cancer cells absorb more sugar than normal cells, making them appear brighter on the scan. This test helps identify if the cancer has spread beyond the liver.
Each diagnostic procedure contributes valuable information about the nature of the liver cancer, helping doctors design a comprehensive and effective treatment plan tailored to the patient’s specific condition.
Complications of Untreated Liver Cancer
Liver cancer, if left untreated, can lead to several severe and potentially life-threatening complications. These arise primarily due to the cancer’s progression within the liver and its spread to other parts of the body. Some of the most serious complications include:
- Liver Failure. As the cancer progresses, it damages healthy liver tissue, making it increasingly difficult for the liver to perform its essential functions. This can lead to liver failure, a condition where the liver can no longer detoxify the blood, produce essential proteins, or regulate important bodily functions, leading to a buildup of toxins, jaundice, and potentially fatal consequences.
- Metastasis. Untreated liver cancer can spread (metastasize) beyond the liver to other parts of the body, including the lungs, bones, and lymph nodes. This spreading makes treatment more complicated and less effective, as cancers in multiple organs are harder to manage. In advanced cases, this can lead to organ failure in affected areas, significantly reducing the patient’s survival chances.
- Ascites. Liver cancer often leads to portal hypertension, a condition where increased pressure builds in the portal vein, causing fluid to leak into the abdominal cavity. This results in a painful swelling of the abdomen known as ascites, which can cause discomfort, breathing difficulties, and infection.
- Jaundice. A common symptom of untreated liver cancer is jaundice, which occurs when the liver fails to process bilirubin, a waste product of red blood cells. This causes yellowing of the skin and eyes, dark urine, and light-colored stools. Jaundice often indicates advanced liver damage.
- Hepatic Encephalopathy. With liver dysfunction, the liver’s inability to filter toxins from the bloodstream can lead to hepatic encephalopathy, a neurological disorder characterized by confusion, memory loss, personality changes, and even coma due to the buildup of toxins in the brain.
- Internal Bleeding (Hemorrhage). Liver cancer can impair the liver’s ability to produce clotting factors, which are essential for stopping bleeding. Patients with advanced liver cancer may develop varices (enlarged veins), particularly in the esophagus or stomach, which can rupture and cause life-threatening internal bleeding.
- Severe Pain. As the tumor grows, it can stretch the liver’s capsule and affect nearby nerves and tissues, causing significant pain in the upper right quadrant of the abdomen. This pain can become debilitating and affect a patient’s quality of life.
- Infection. Liver cancer weakens the immune system and increases the risk of bacterial infections, particularly in the abdomen (peritonitis) or other areas. These infections can become serious, leading to sepsis if not treated promptly.
- Nutritional Deficiencies and Weight Loss. The cancer and its impact on the liver’s ability to process nutrients can lead to severe weight loss and malnutrition. This condition, known as cachexia, often contributes to the weakening of the patient and a decline in overall health.
- Death. If liver cancer progresses unchecked, it can lead to liver failure, widespread metastasis, and ultimately death. The prognosis for untreated liver cancer is generally poor, emphasizing the importance of early detection and treatment.
Untreated liver cancer is a rapidly progressing condition with high morbidity and mortality rates. Early diagnosis and intervention are crucial to managing the disease and preventing these severe complications.
Causes of Liver Cancer
Hepatocellular carcinoma, the most common type of liver cancer, typically develops in a liver already damaged by certain conditions. Key factors contributing to this disease include:
- Congenital Conditions. Some individuals are born with liver-related disorders, such as biliary atresia or metabolic conditions, which can lead to liver damage over time, increasing the risk of cancer.
- Alcohol Abuse. Chronic alcohol consumption damages liver cells and can lead to cirrhosis, a known risk factor for hepatocellular carcinoma.
- Cirrhosis. Scarring of the liver caused by chronic injury — from hepatitis, alcohol abuse, or other liver diseases — significantly raises the risk of liver cancer.
- Hepatitis B and C. Chronic infections with these viruses are major contributors to liver cancer globally, especially when left untreated, as they cause long-term inflammation and liver damage.
- Hereditary Conditions. Genetic disorders like hemochromatosis, where excess iron builds up in the liver, can lead to cancerous changes over time.
Substances Linked to Liver Cancer
In addition to health conditions, certain harmful substances have been identified as carcinogens that raise the risk of liver cancer:
- Chemicals in Cigarettes. Long-term smoking exposes the liver to toxins that can contribute to cancer, especially in those who also drink alcohol heavily.
- Vinyl Chloride. This industrial chemical, used in plastics production, has been associated with liver angiosarcoma, a rare but aggressive form of cancer.
- Arsenic. Drinking water contaminated with arsenic increases the risk of liver cancer, as chronic exposure causes liver cell damage.
- Aflatoxin. This toxin, produced by mold on crops like peanuts and corn, is a potent liver carcinogen. The risk is particularly high when combined with hepatitis B infection.
- Androgens and Estrogens. Long-term use of steroids (androgens) or estrogen therapy can stimulate abnormal cell growth in the liver, increasing the risk of cancer.
- Thorotrast. This now-discontinued radioactive substance used in medical imaging is known to cause liver cancer, particularly angiosarcoma.
These factors emphasize how a combination of lifestyle habits, genetic predispositions, and environmental exposures contribute to the development of liver cancer.
Prevention of Liver Cancer
Ris There are various ways to lower the risk of developing liver cancer, primarily by addressing factors that increase the likelihood of the disease. The key to prevention is minimizing liver damage and maintaining overall liver health.

One critical preventive measure is avoiding cirrhosis, a condition where scar tissue forms in the liver due to long-term injury. Cirrhosis significantly raises the risk of liver cancer. Here are steps to prevent cirrhosis:
- Limit or avoid alcohol consumption. Heavy drinking over time can damage liver cells and lead to cirrhosis. If you drink, do so in moderation.
- Maintain a healthy weight. Obesity is linked to non-alcoholic fatty liver disease, which can progress to cirrhosis and liver cancer. Ensure that your weight aligns with your height and age.
- Avoid foods high in fat and cholesterol. These can contribute to fatty liver disease, increasing the risk of cirrhosis over time. Opt for a balanced diet rich in fruits, vegetables, and lean proteins.
- Exercise regularly. Engage in at least 30 minutes of physical activity each day to maintain liver health and reduce fat accumulation.
In addition to these lifestyle adjustments, other measures to prevent liver cancer include:
- Get vaccinated against hepatitis B. Chronic hepatitis B infection is a significant cause of liver cancer. Vaccination is an effective preventive tool, especially for those at high risk.
- Take prescribed antiviral medication. For those with hepatitis B or C, antiviral medications, as recommended by a doctor, can help control the infection and prevent liver damage from progressing to cancer.
- Regular liver screenings. For individuals at high risk (such as those with a history of hepatitis or cirrhosis), routine liver screenings can help detect early signs of liver cancer.
- Practice safe sex. Use protection, such as condoms, during intercourse to prevent the transmission of hepatitis B and C, both of which significantly raise the risk of liver cancer.
Taking these precautions can significantly reduce the chances of developing liver cancer and promote long-term liver health.
Risk Factors for Liver Cancer
There are several factors that can increase the risk of developing liver cancer. These risk factors are linked to lifestyle choices, genetic predisposition, and certain environmental exposures.
- Type 2 Diabetes. Studies have shown a connection between type 2 diabetes and liver cancer. Individuals with type 2 diabetes are two to three times more likely to develop this type of cancer compared to those without diabetes. This is often due to the higher likelihood of liver disease, such as fatty liver disease, in people with diabetes.
- Family History of Liver Cancer. Those with a parent or sibling who has had liver cancer are at a significantly higher risk of developing the disease. Genetic predispositions and shared lifestyle habits may contribute to this increased risk.
- Heavy Alcohol Consumption. One of the primary causes of cirrhosis, a known precursor to liver cancer, is excessive alcohol intake. Continuous abuse of alcohol damages the liver cells and can lead to cirrhosis, which in turn can progress to liver cancer.
- Smoking. Smoking is known to increase the risk of chronic liver infections, such as hepatitis B and C, which are major causes of liver cancer. Smoking also has direct toxic effects on liver cells, making smokers more vulnerable to liver cancer.
- Exposure to Aflatoxins. Aflatoxins are toxic compounds produced by certain types of fungi that can contaminate food products, such as peanuts, soybeans, and corn. While the risk of aflatoxin exposure is relatively low for most people, prolonged or high exposure can significantly increase the risk of liver cancer.
- Weakened Immune System. Individuals with a compromised immune system, such as those with HIV/AIDS, have a heightened risk of developing liver cancer. A weakened immune system makes it harder for the body to fight off infections, including chronic hepatitis B and C, which can lead to cancer.
- Obesity. Being overweight or obese increases the likelihood of fatty liver disease and cirrhosis, both of which are linked to liver cancer. The accumulation of fat in the liver causes inflammation and can damage liver cells over time.
- Gender. Liver cancer is more common in men than women. This is largely due to lifestyle factors—men are more likely to engage in behaviors such as smoking and heavy drinking, both of which increase the risk of liver cancer.
- Arsenic Exposure. People who consume water contaminated with high levels of arsenic, especially from unregulated wells, are at an elevated risk of liver cancer and other liver-related conditions. Long-term exposure to arsenic can lead to various forms of liver damage, including cancer.
By understanding these risk factors, individuals can take steps to lower their chances of developing liver cancer, such as reducing alcohol consumption, maintaining a healthy weight, avoiding smoking, and managing any underlying health conditions like diabetes or hepatitis.
Liver Cancer FAQs
- What is liver cancer?
Liver cancer refers to the abnormal growth of malignant cells in the liver. It can either be primary, starting in the liver, or secondary, originating from other organs and spreading to the liver. Primary liver cancer, particularly hepatocellular carcinoma, is the most common type. - What are the main causes of liver cancer?
Liver cancer is often caused by underlying liver conditions such as cirrhosis, hepatitis B and C infections, excessive alcohol consumption, and non-alcoholic fatty liver disease. Other risk factors include diabetes, obesity, and exposure to toxins like aflatoxins or arsenic. - What are the symptoms of liver cancer?
Common symptoms include yellowing of the skin and eyes (jaundice), pain or swelling in the upper abdomen, weight loss, loss of appetite, nausea, and fatigue. These symptoms can appear in the later stages of the disease, making early detection challenging. - How is liver cancer diagnosed?
Diagnosis typically involves imaging tests like ultrasound, CT scans, or MRI, along with blood tests to detect markers like alpha-fetoprotein (AFP). A liver biopsy, where a tissue sample is analyzed, may also be performed to confirm the diagnosis. - Is liver cancer curable?
The prognosis depends on the stage at diagnosis. Early-stage liver cancer can sometimes be treated successfully with surgery, liver transplants, or targeted therapies. However, advanced liver cancer has a lower survival rate, and treatment focuses on managing symptoms and slowing disease progression. - What are the treatment options for liver cancer?
Treatment may include surgery (partial hepatectomy or liver transplant), radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The best approach depends on the stage and type of cancer, as well as the patient’s overall health. - How can liver cancer be prevented?
Prevention focuses on managing risk factors, such as getting vaccinated for hepatitis B, reducing alcohol consumption, avoiding smoking, maintaining a healthy weight, and controlling conditions like hepatitis C and diabetes. Regular screening is recommended for individuals at high risk. - Can liver cancer spread to other organs?
Yes, liver cancer can metastasize, or spread, to other parts of the body, such as the lungs, bones, or lymph nodes. This is more common in advanced stages and requires systemic treatments like chemotherapy or targeted therapies. - Who is at the highest risk of developing liver cancer?
People with chronic liver disease (especially cirrhosis), chronic hepatitis B or C infections, those who consume excessive alcohol, or have a family history of liver cancer are at a higher risk. Men are also more likely to develop liver cancer than women. - What is the survival rate for liver cancer?
The survival rate depends on the stage at which the cancer is detected. Early-stage liver cancer has a higher survival rate, while advanced stages, particularly when the cancer has spread, have a lower 5-year survival rate.