Summary
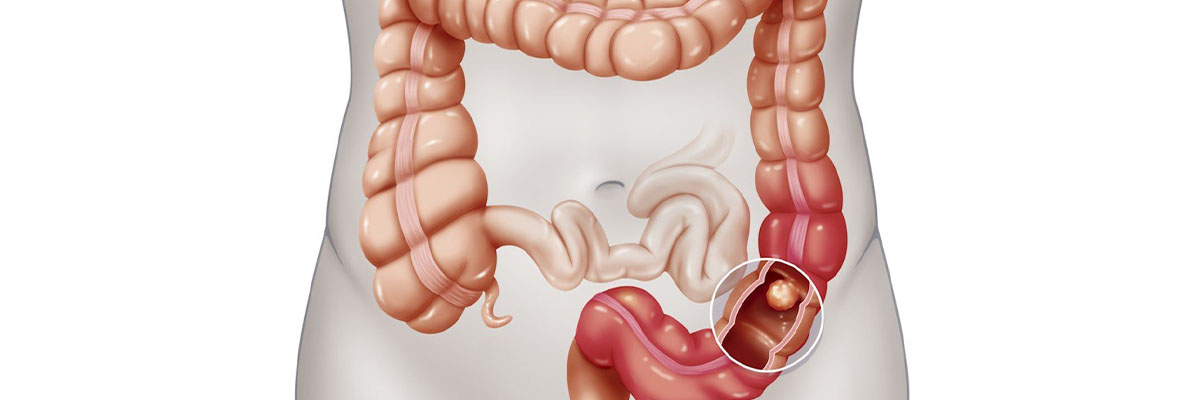
One of the most common types of cancer is colon cancer, also referred to as colorectal cancer. This disease originates from abnormal cell growth and tumor formation in the large intestine (colon). Over time, these tumors can become cancerous, posing serious health risks if left untreated.
Symptoms of colon cancer can include changes in bowel habits, such as constipation or diarrhea that lasts for more than a few days, rectal bleeding, blood in the stool, frequent bloating, abdominal cramps, and general abdominal discomfort. Fatigue or weakness is also common, as colon cancer may cause gradual blood loss, leading to anemia and low energy levels.
Treatment options for colon cancer typically involve a combination of therapies based on the cancer’s stage and location. These may include surgery to remove the tumor, radiation therapy, chemotherapy, and targeted therapy to control or shrink cancerous growth. Early detection is essential, as it significantly increases the effectiveness of treatment and improves survival rates.
Table of Contents
Symptoms of Colon Cancer

In the early stages of colon cancer, there may be no noticeable symptoms. However, as the disease progresses, certain signs and symptoms may begin to appear:
- Changes in bowel habits. This can include persistent constipation, frequent diarrhea, or alternating between the two, often without an obvious cause.
- Rectal bleeding. Blood may be seen in the stool or on the toilet paper after bowel movements.
- Blood in the stool. Stools may appear dark or have visible red streaks, indicating the presence of blood, which can sometimes be mistaken for hemorrhoids.
- Abdominal discomfort. This can include cramping, bloating, or a general feeling of discomfort in the abdomen.
- Feeling of fullness. A persistent sensation that the bowel hasn’t fully emptied can lead to discomfort and unease.
- Extreme fatigue and weakness. As the cancer progresses, fatigue becomes more pronounced, often due to anemia caused by blood loss.
- Unexplained weight loss. Rapid and unintentional weight loss may occur even without significant changes in diet or activity.
It is important to note that these symptoms can be subtle and mistaken for less serious digestive issues. Early screening, especially for those at higher risk, plays a crucial role in detecting colon cancer in its initial stages.
Types of Colon Cancer
There are several types of cancer that can develop in the colon. Here are some of the most common types:
- Adenocarcinoma. Adenocarcinoma is the most common type of colon cancer. It starts in the lining of the large intestine and originates in glandular cells that produce mucus and enzymes. Often, these cancers begin as small adenomatous polyps, which gradually grow and may eventually become malignant tumors if left untreated. Over 95% of colon cancers are adenocarcinomas.
- Gastrointestinal Stromal Tumors (GIST). GISTs begin in the muscle layer of the digestive tract, and while they often start in the stomach or small intestine, they can spread to the colon. When GISTs become malignant, they are classified as sarcomas. Surgical removal is typically recommended to prevent their spread.
- Lymphoma. While lymphomas commonly start in the lymph nodes, they can also originate in the colon or rectum. Lymphomas are cancers of the lymphatic system, which is part of the immune system, and may require specialized treatments such as chemotherapy or radiation.
- Carcinoid Tumors. Carcinoid tumors are slow-growing cancers that begin in the hormone-producing cells of the gastrointestinal tract, especially in the colon. When they become malignant, they can spread to other parts of the body. Surgery is the primary treatment for carcinoid tumors.
- Familial Colorectal Cancer (FCC). FCC is a hereditary form of colon cancer that runs in families. Individuals with a family history of colorectal cancer are at a higher risk of developing the disease, often at an earlier age than those without a genetic predisposition. Regular screenings are essential for early detection in at-risk families.
- Juvenile Polyposis Coli. Juvenile Polyposis Coli is a rare genetic condition primarily affecting children. It is associated with multiple hamartomatous polyps that may occur throughout the gastrointestinal tract. Although these polyps are generally benign, they have the potential to become cancerous over time, so early intervention and regular monitoring are crucial.
Understanding the various types of colon cancer is important, as different types may require different treatment approaches. Early diagnosis and treatment can significantly improve outcomes for most colon cancer patients.
Diagnostic Procedures for Colon Cancer
Early detection is crucial for effectively treating colon cancer, as it often develops without symptoms in its early stages. A range of diagnostic procedures can help identify colon cancer or precancerous conditions, such as polyps, before they progress. Here are the primary diagnostic methods used:
- Colonoscopy. A colonoscopy is the most comprehensive test for detecting colon cancer. During the procedure, a long, flexible tube with a camera (colonoscope) is inserted into the rectum, allowing doctors to view the entire colon. If polyps or suspicious tissue are found, they can be removed or biopsied immediately for further examination.
- Fecal immunochemical test (FIT). The FIT test detects hidden (occult) blood in the stool, which may indicate polyps or cancer. It is non-invasive and is usually recommended annually for those at average risk. A positive FIT result generally leads to a follow-up colonoscopy.
- Stool DNA test (e.g., Cologuard). This test detects specific DNA markers associated with cancer cells in the stool, as well as hidden blood. While not as precise as a colonoscopy, it is an effective non-invasive option that can be done at home every 1-3 years. A positive result requires a follow-up colonoscopy.
- CT colonography (Virtual Colonoscopy). This imaging procedure uses a CT scan to produce detailed, three-dimensional images of the colon and rectum. It’s a non-invasive alternative to a traditional colonoscopy, although if polyps are found, a standard colonoscopy will still be needed to remove or biopsy the tissue.
- Flexible sigmoidoscopy. Similar to a colonoscopy, this procedure uses a flexible tube to examine only the lower part of the colon. While it doesn’t provide a full view, it can detect abnormalities in the sigmoid colon and rectum. Polyps found can be biopsied, but a full colonoscopy may be recommended for further screening.
- Biopsy. During a colonoscopy or sigmoidoscopy, if suspicious tissue is found, a small sample (biopsy) can be taken for microscopic analysis. This helps to confirm whether cancer cells are present and determine the type and aggressiveness of the cancer.
- Blood tests. While blood tests cannot diagnose colon cancer directly, they are often used to check for markers like carcinoembryonic antigen (CEA), which may indicate the presence of cancer. Blood tests can also evaluate overall health and help guide treatment decisions.
- Imaging tests (MRI, PET scans, and ultrasounds). If colon cancer is suspected or confirmed, additional imaging tests may be performed to assess the spread (staging) of the cancer. MRI and PET scans, for example, provide detailed views that help in planning surgery or other treatments.
Each of these diagnostic procedures plays a vital role in identifying colon cancer early, when treatment is most effective. Consulting a healthcare provider about the most appropriate screening based on individual risk factors can ensure proactive and personalized care.
Complications of Untreated Colon Cancer
Untreated colon cancer can lead to serious and potentially life-threatening complications. As the cancer progresses, it can spread beyond the colon, affecting nearby organs and tissues, and creating health challenges that significantly impact quality of life. Here are some of the major complications of untreated colon cancer:
- Intestinal obstruction. A growing tumor can block the passage of food and waste through the intestines, leading to an obstruction. This may cause severe abdominal pain, vomiting, constipation, and bloating. In extreme cases, emergency surgery may be required to remove the blockage and prevent further complications.
- Perforation of the colon. Tumors that grow unchecked can weaken the wall of the colon, leading to a tear or perforation. This is a serious condition that allows contents from the colon to leak into the abdominal cavity, causing infection (peritonitis) that can be life-threatening and often requires emergency surgical intervention.
- Spread to other organs (metastasis). Colon cancer, if untreated, is likely to metastasize, or spread, to other parts of the body. The liver is a common site for colon cancer metastasis, followed by the lungs and lymph nodes. Metastasis complicates treatment, reduces survival rates, and requires more aggressive and complex treatments, such as chemotherapy, targeted therapy, or radiation.
- Bleeding and anemia. Untreated tumors may bleed internally, leading to chronic blood loss. This can cause anemia, a condition characterized by fatigue, weakness, and shortness of breath due to a lack of healthy red blood cells. Severe anemia can strain the heart and other organs, impacting overall health and quality of life.
- Increased pain and discomfort. As the tumor grows and spreads, it can press on surrounding organs and nerves, leading to persistent pain and discomfort. This pain can be difficult to manage and may affect daily activities and mental well-being.
- Fistula formation. Tumors can create abnormal connections (fistulas) between the colon and nearby organs, such as the bladder or vagina. This can lead to infections and other complications that require surgical repair.
- Systemic symptoms and organ failure. In advanced stages, colon cancer may lead to systemic symptoms like weight loss, muscle wasting, and overall weakness. If cancer spreads to the liver or lungs, it can lead to liver failure or respiratory distress, both of which are life-threatening and limit treatment options.
- Reduced quality of life and mental health challenges. The physical symptoms and health decline associated with untreated colon cancer can impact mental health, leading to anxiety, depression, and other emotional challenges. Pain, fatigue, and reduced mobility contribute to a diminished quality of life, making daily tasks increasingly difficult.
Recognizing the serious risks of untreated colon cancer underscores the importance of early detection, routine screening, and timely treatment. Addressing colon cancer in its early stages can prevent these severe complications and improve long-term outcomes, offering a greater chance of recovery and a better quality of life.
Causes of Colon Cancer
Colon cancer typically begins as non-cancerous (benign) growths known as adenomatous polyps, which form on the inner lining of the colon. Over time, these polyps may develop cellular changes that lead them to become malignant. Once malignant, these cancerous cells can spread to other parts of the body through the bloodstream and the lymphatic system, affecting other organs and tissues.
The exact cause of colon cancer is still unknown. However, several risk factors associated with the disease have been identified, which we will discuss in more detail later in this article.
Understanding the progression from benign polyps to malignant tumors emphasizes the importance of routine screening, as early detection of polyps can significantly reduce the risk of developing advanced colon cancer.
Prevention of Colon Cancer

The best way to prevent colon cancer is to detect and treat it in its early stages. Regular screenings, such as colonoscopies and blood tests, play a critical role in early detection and can greatly reduce the risk of developing advanced colon cancer.
Additionally, the following preventive measures can help lower the risk of colon cancer:
- Quit smoking. Long-term smoking has been linked to an increased risk of various cancers, including colon cancer. Stopping smoking can have numerous health benefits beyond reducing cancer risk.
- Daily aspirin use (as advised by a doctor). Some studies suggest that daily, low-dose aspirin may reduce the risk of colon cancer in certain people. However, this should only be done under medical guidance, as aspirin can have side effects.
- Daily folic acid intake (as advised by a doctor). Folic acid, a B vitamin, may play a role in cell health. Its supplementation has been associated with a lower risk of colorectal cancer, but the benefits vary among individuals, and supplementation should be discussed with a healthcare provider.
- Regular exercise. Physical activity has numerous benefits, including improved digestion, a healthier body weight, and a lower risk of many cancers, including colon cancer.
- A diet rich in vegetables, fruits, and fiber. Consuming a variety of vegetables, fruits, and fiber-rich foods supports digestive health and may help reduce the risk of colon cancer. Fiber, in particular, aids in regular bowel movements, which is beneficial for colon health.
Incorporating these lifestyle changes can have a positive impact not only on colon health but also on overall well-being. Additionally, consulting with healthcare professionals for personalized prevention strategies is highly recommended.
Risk Factors for Colon Cancer
Some risk factors for developing colon cancer include:
- Age. While colon cancer can affect people of any age, the risk significantly increases for those over 50.
- Previous colon cancer. Individuals who have previously recovered from colon cancer have a higher likelihood of recurrence.
- Family history of colon cancer. Having relatives, especially immediate family members, with colon cancer raises one’s risk due to shared genetic factors.
- Chronic bowel conditions. Chronic inflammatory conditions in the colon, such as ulcerative colitis and Crohn’s disease, increase the likelihood of developing colon cancer over time due to prolonged inflammation.
- Diet high in fat and low in fiber. A diet rich in fats and low in fiber has been associated with an increased risk of colon cancer, possibly due to slower digestion and prolonged exposure of the colon to potential carcinogens.
- Lack of physical activity. Sedentary lifestyles are linked to a higher risk of colon cancer, as regular exercise supports healthy digestion and overall immune function.
- Obesity. Studies show that overweight and obese individuals have a greater risk of colon cancer compared to those with a healthy weight.
- Diabetes. Having diabetes is associated with a higher risk of colon cancer, likely due to insulin resistance and other metabolic factors affecting cellular growth.
- Smoking. Smoking introduces harmful chemicals that increase the risk of various cancers, including colon cancer, due to their effect on cellular DNA.
- Excessive alcohol consumption. High alcohol intake can contribute to colon cancer risk, as alcohol can damage the cells lining the colon.
- Radiation therapy for other cancers. Past radiation treatments, especially those involving the abdomen, can damage healthy cells in the colon, increasing the risk of colon cancer.
- Ethnicity. Research indicates that African Americans have a higher incidence of colon cancer compared to other ethnic groups, possibly due to genetic, dietary, and socioeconomic factors.
Understanding these risk factors is crucial for prevention and early detection strategies. Regular screenings and lifestyle modifications, such as a balanced diet, exercise, and avoiding tobacco and excessive alcohol, can reduce these risks significantly.
Colon Cancer FAQs
Colon cancer is one of the most common types of cancer, affecting millions of people worldwide. Understanding the risk factors, symptoms, and preventive measures can make a significant difference in early detection and treatment outcomes. The following FAQs address common questions and provide essential information about colon cancer to help you stay informed and proactive about your health.
- What is colon cancer?
Colon cancer is a type of cancer that begins in the large intestine (colon). It typically starts as small, noncancerous clumps of cells called polyps, which over time may develop into cancer. - What are the symptoms of colon cancer?
In early stages, colon cancer often has no symptoms. As it progresses, symptoms may include changes in bowel habits, blood in the stool, persistent abdominal discomfort, fatigue, and unexplained weight loss. - Who is at risk for colon cancer?
Risk factors include being over the age of 50, a family history of colon cancer, chronic inflammatory bowel diseases (such as Crohn’s disease or ulcerative colitis), a diet low in fiber and high in fat, smoking, obesity, and a sedentary lifestyle. - How is colon cancer diagnosed?
Colon cancer is diagnosed through screening methods such as colonoscopy, stool tests (like FIT or Cologuard), CT colonography, and flexible sigmoidoscopy. A colonoscopy is the most common method, allowing doctors to visualize the colon and remove polyps if found. - What are polyps, and are they always cancerous?
Polyps are small growths on the lining of the colon. While most are benign, some types, especially adenomatous polyps, have the potential to become cancerous over time. Removing polyps during a colonoscopy can prevent them from developing into cancer. - Can colon cancer be prevented?
Prevention strategies include regular screenings, a healthy diet rich in fiber, regular exercise, maintaining a healthy weight, avoiding smoking, and limiting alcohol intake. These measures can reduce the risk but do not guarantee prevention. - What are the treatment options for colon cancer?
Treatment depends on the stage of the cancer and may include surgery, chemotherapy, radiation therapy, and targeted therapies. Surgery is typically the primary treatment for early-stage colon cancer, while advanced cases may require a combination of treatments. - How does staging work for colon cancer?
Staging describes how far cancer has spread. Stages range from 0 (cancer in situ, meaning it hasn’t spread) to IV (cancer has spread to other organs). Staging helps guide treatment decisions and determine prognosis. - Is colon cancer hereditary?
Yes, about 5-10% of colon cancers are due to inherited gene mutations. Family history of colon cancer or inherited syndromes like Lynch syndrome or familial adenomatous polyposis (FAP) increases the risk and may warrant earlier and more frequent screenings. - At what age should I start getting screened for colon cancer?
Most people should start screenings at age 45 or 50, depending on risk factors. Those with a family history of colon cancer or other risk factors may need to begin screenings earlier. - How does lifestyle affect the risk of colon cancer?
A diet high in red and processed meats, lack of exercise, obesity, smoking, and excessive alcohol use have all been linked to an increased risk of colon cancer. Maintaining a healthy lifestyle can help lower this risk. - Are there any new developments or research in colon cancer treatment?
Recent advances include targeted therapies and immunotherapies that specifically attack cancer cells while sparing healthy cells. Research is also exploring personalized treatments based on genetic testing of the tumor, improving outcomes and reducing side effects. - Is colon cancer treatable?
Yes, colon cancer is highly treatable, especially when detected early. Survival rates are high for early-stage cancers, and even advanced stages have a range of treatment options that can extend and improve quality of life. - How often should I get screened if my first test was normal?
For individuals with an average risk, a normal colonoscopy typically means you won’t need another one for 10 years. Other types of tests, such as stool tests, may need to be done more frequently (annually or every three years). - What should I do if I think I might be at risk for colon cancer?
If you believe you’re at risk, speak with your doctor about your concerns. They can help you assess your risk factors and recommend appropriate screening tests and lifestyle changes. Early detection through screening is the best defense against colon cancer.