Summary
Breast cancer occurs when cancer cells in the breast grow uncontrollably, forming a tumor. While breast cancer predominantly affects women, it can also develop in men, though much less frequently.
The cancer typically begins as a tumor in the breast tissue. As it progresses, the tumor grows larger and may invade nearby tissues, a process known as metastasis. In advanced stages, breast cancer can spread to other parts of the body, including the lymph nodes, lungs, liver, bones, and brain.
Common symptoms of breast cancer include the presence of a lump in the breast, changes in the shape or size of the breast, redness or swelling of the skin, and the retraction or inversion of the nipples. Early detection is crucial, and treatment options vary depending on the stage and type of cancer. These treatments may include surgery to remove the tumor, radiation therapy to target cancer cells, and chemotherapy to destroy cancer cells throughout the body.
With early diagnosis and the right treatment plan, many individuals with breast cancer can achieve a successful recovery. Regular screening and awareness of the symptoms are essential for catching the disease in its early stages when treatment is most effective.
Table of Contents
Symptoms of Breast Cancer

Breast cancer can present with a variety of signs and symptoms, which may vary from person to person. It is important to recognize these symptoms early for prompt diagnosis and treatment. Here are the most common symptoms of breast cancer:
- Presence of a Lump in the Breast. A new lump or mass in the breast that feels different from the surrounding tissue is often the first noticeable symptom of breast cancer. These lumps are typically hard, irregular in shape, and painless, though some can be tender. Not all lumps are cancerous, but it’s important to have any new lump checked by a doctor.
- Changes in Breast Skin. The skin of the breast may develop visible changes, such as dimpling or puckering, often resembling the texture of an orange peel. This change in texture can indicate underlying cancer affecting the tissue.
- Alterations in Breast Size, Shape, or Appearance. Any unexplained change in the size or shape of one breast compared to the other could be a sign of breast cancer. Swelling or shrinking of the breast, or any noticeable asymmetry, should be evaluated by a healthcare provider.
- Inverted or Retracted Nipple. A nipple that suddenly becomes inverted (pulled inward) or changes position can be a symptom of breast cancer. In some cases, nipple inversion can be accompanied by other changes in the appearance of the breast.
- Redness or Discoloration of the Breast Skin. Unusual redness, warmth, or swelling of the breast can be a sign of inflammatory breast cancer, a rare but aggressive form of the disease. The breast may appear inflamed or feel thicker than usual.
- Peeling, Scaling, or Cracking of the Areola or Breast Skin. Skin changes around the nipple, including peeling, scaling, or cracking of the skin, can be associated with breast cancer. These symptoms might affect the areola (the darkened area around the nipple) or the skin on other parts of the breast. Persistent irritation or flaking should not be ignored.
If you notice any of these symptoms, it is essential to consult a healthcare provider for further evaluation. While these symptoms do not always indicate cancer, early detection is critical in improving treatment outcomes for breast cancer. Regular self-exams and screenings, such as mammograms, are key to catching breast cancer in its earliest stages when it is most treatable.
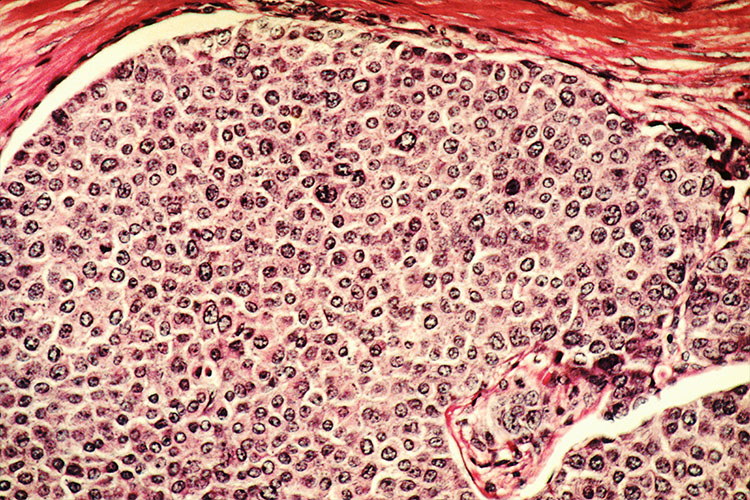
Types of Breast Cancer
The most common type of breast cancer is carcinoma, but there are various subtypes based on where the cancer originates and how it behaves. Understanding the different types of breast cancer is essential for accurate diagnosis and treatment planning. Here are the main types:
- In Situ Breast Cancer. This type of breast cancer is confined to the place where it started and has not yet spread to surrounding breast tissue. There are two primary forms:
- Ductal Carcinoma In Situ (DCIS). Also known as intraductal carcinoma, this type forms in the ducts of the breast. Although it is non-invasive, if left untreated, it can progress to invasive breast cancer.
- Lobular Carcinoma In Situ (LCIS). LCIS develops in the milk-producing glands (lobules) of the breast. While it is not considered cancer, it indicates a higher risk of developing breast cancer in the future.
- Invasive Breast Cancer. In this type, cancer has spread beyond the initial site to surrounding breast tissue. The most common types of invasive breast cancer include:
- Invasive Ductal Carcinoma (IDC). This cancer starts in the ducts but spreads to nearby breast tissue and possibly other parts of the body.
- Invasive Lobular Carcinoma (ILC). This cancer begins in the lobules and can also invade nearby tissues.
There are also less common forms of breast cancer, including:
- Inflammatory Breast Cancer (IBC). A rare and aggressive form of invasive breast cancer, IBC accounts for 1% to 5% of all breast cancer cases. It causes the breast to appear red, swollen, and inflamed, often without a noticeable lump. This type of cancer tends to spread quickly and requires prompt treatment.
- Paget Disease of the Nipple. This rare condition begins in the breast ducts and spreads to the skin of the nipple and areola. Symptoms often include crusting, scaling, or redness around the nipple. Paget disease is often associated with DCIS or invasive breast cancer.
- Phyllodes Tumor. A rare type of tumor that forms in the connective tissue of the breast. Most phyllodes tumors are benign (non-cancerous), but some can become malignant and spread to other parts of the body. These tumors grow rapidly and may require surgical removal.
- Angiosarcoma. This rare form of breast cancer develops in the cells lining the lymphatic or blood vessels in the breast. Angiosarcoma may be linked to previous radiation therapy for breast cancer or may occur spontaneously. Because of its aggressive nature, early detection is crucial.
Each type of breast cancer requires a specific treatment approach, depending on the cancer’s stage, location, and whether it has spread. Accurate diagnosis helps doctors determine the best course of action, whether it be surgery, radiation, chemotherapy, or other treatments.
Diagnostic Procedures for Breast Cancer
Diagnosing breast cancer involves a series of tests and examinations to accurately detect cancer, determine its stage, and develop an appropriate treatment plan. Here are the common diagnostic procedures for breast cancer:
- Mammogram. A mammogram is an X-ray of the breast and is one of the most effective tools for early detection of breast cancer. It can reveal abnormal growths or lumps that may not yet be palpable. Women are often advised to undergo regular mammograms, particularly after age 40, to detect breast cancer at its earliest, most treatable stages.
- Breast Ultrasound. An ultrasound uses sound waves to produce detailed images of the breast tissue. It is commonly used to further examine abnormalities found during a mammogram or physical exam. Ultrasound can help distinguish between a fluid-filled cyst (which is usually benign) and a solid mass (which may be cancerous).
- Magnetic Resonance Imaging (MRI). A breast MRI is often used to gather more detailed images of the breast tissue, especially in women who are at high risk for breast cancer or have dense breast tissue. MRI scans can detect cancerous growths that may not show up on a mammogram or ultrasound, and they are often used in conjunction with other diagnostic tests.
- Biopsy. A biopsy is the definitive test for diagnosing breast cancer. In this procedure, a sample of breast tissue or cells is removed from the suspicious area and examined under a microscope to check for cancer cells. There are several types of biopsies:
- Fine-Needle Aspiration (FNA). A thin needle is used to extract a small sample of fluid or cells from a lump.
- Core Needle Biopsy. A larger needle is used to remove a small core of tissue.
- Surgical Biopsy. In some cases, a portion or all of the suspicious tissue is surgically removed for examination.
- Hormone Receptor and HER2 Testing. Once a biopsy confirms breast cancer, further testing is often done to determine whether the cancer cells have hormone receptors (for estrogen or progesterone) or an excess of the HER2 protein. These tests help guide treatment decisions, as hormone receptor-positive cancers may respond to hormone therapy, and HER2-positive cancers may be treated with targeted therapy.
- Sentinel Lymph Node Biopsy. This test helps determine whether breast cancer has spread to the lymph nodes. The sentinel lymph node is the first lymph node to which cancer cells are likely to spread from the primary tumor. A biopsy of this node can help assess the stage of cancer and whether further treatment is needed to target lymphatic spread.
- Genomic Testing. For some patients, genomic tests such as Oncotype DX or MammaPrint may be performed to evaluate the genetic characteristics of the cancer. These tests can help predict how aggressive the cancer is and whether the patient would benefit from chemotherapy or other treatments.
By combining these diagnostic tools, doctors can accurately assess whether breast cancer is present, its type and stage, and the best course of action for treatment. Early detection through screening, such as regular mammograms, is crucial in catching breast cancer at its most treatable stages, significantly improving survival rates and outcomes.
Complications of Untreated Breast Cancer
If left untreated, breast cancer can lead to serious complications that affect not only the breast but also other parts of the body. The disease tends to progress over time, becoming more difficult to treat and increasing the risk of life-threatening outcomes. Here are the common complications of untreated breast cancer:
- Metastasis (Spread of Cancer). One of the most dangerous complications of untreated breast cancer is metastasis, where the cancer spreads to other parts of the body. Breast cancer can metastasize to nearby lymph nodes, as well as distant organs such as the bones, lungs, liver, and brain. Once breast cancer spreads, it becomes more challenging to treat and requires more aggressive therapies.
- Bone Complications. When breast cancer spreads to the bones, it can cause significant pain and weaken the bones, increasing the risk of fractures. Bone metastasis can also lead to hypercalcemia, a condition where too much calcium is released into the bloodstream, causing symptoms such as nausea, vomiting, dehydration, and confusion.
- Lung Complications. If breast cancer metastasizes to the lungs, it can cause pleural effusion, which is the buildup of fluid in the space around the lungs. This can result in difficulty breathing, chest pain, and coughing. Untreated, this condition can severely impair lung function and overall respiratory health.
- Liver Damage. Breast cancer that spreads to the liver can cause liver failure, leading to symptoms such as jaundice (yellowing of the skin and eyes), abdominal pain, nausea, and swelling in the abdomen. Liver metastasis is often a sign of advanced breast cancer and may require specialized treatment.
- Brain Metastasis. When breast cancer spreads to the brain, it can cause neurological complications, including headaches, seizures, vision problems, confusion, and cognitive decline. Brain metastasis can significantly affect a person’s quality of life and may require treatments like radiation or surgery to manage symptoms.
- Chronic Pain. As breast cancer progresses and spreads to other parts of the body, patients may experience persistent pain, especially if the cancer has invaded the bones, muscles, or nerves. This pain can become debilitating and may require specialized pain management strategies, including medications and palliative care.
- Lymphedema. Breast cancer can block the normal flow of lymphatic fluid, leading to lymphedema, a condition characterized by painful swelling in the arms, chest, or breast. This can occur if the cancer spreads to the lymph nodes or if lymph nodes are damaged or removed during treatment. Lymphedema can cause discomfort, restrict movement, and increase the risk of infection.
- Severe Infections. Untreated breast cancer can weaken the immune system, making the body more susceptible to infections. This risk is heightened if cancer spreads to the lymphatic system or blood vessels, impairing the body’s ability to fight off harmful pathogens.
- Death. Ultimately, untreated breast cancer can be fatal, especially as it spreads to vital organs and causes irreversible damage. The progression of the disease can lead to organ failure, severe infections, and other life-threatening complications.
Early detection and treatment of breast cancer are crucial to preventing these severe complications. Timely intervention not only improves survival rates but also enhances the quality of life by reducing the risk of metastasis and other associated health issues. Regular screenings, such as mammograms, and being aware of early symptoms can make a significant difference in the outcome of breast cancer.
Causes of Breast Cancer
Breast cancer develops when abnormal breast cells begin to multiply uncontrollably, forming a tumor. This process usually starts when there are mutations or changes in the DNA of the breast cells. These mutations disrupt the normal growth and repair cycle of cells, causing them to grow and divide faster than healthy cells. Over time, these cancerous cells can form a mass or tumor.
Breast cancer can originate in various parts of the breast, but it most commonly begins in the milk ducts (ductal carcinoma), which carry milk from the lobules (milk-producing glands) to the nipple. In some cases, it may start in the lobules themselves (lobular carcinoma) or other tissues of the breast.
As breast cancer progresses, it can invade nearby tissues and spread (metastasize) to other parts of the body. The cancer cells often travel through the lymphatic system, a network of lymph nodes (kulani) and vessels that help the body fight infections. Once the cancer reaches the lymph nodes, it has a higher chance of spreading to distant organs such as the lungs, liver, bones, and brain.
The exact causes of why these mutations occur are still not entirely clear, but genetic, hormonal, and environmental factors are believed to play a role. Hormonal imbalances, particularly involving estrogen and progesterone, can influence breast cell growth and contribute to cancer development. Additionally, certain inherited genetic mutations, such as BRCA1 and BRCA2, are known to significantly increase the risk of breast cancer.
In summary, breast cancer arises from uncontrolled cell growth in the breast, typically starting in the ducts or lobules. As the disease advances, it can spread to other parts of the body, making early detection and treatment crucial to prevent its progression.
Prevention of Breast Cancer

While there is currently no guaranteed way to prevent breast cancer, there are several proactive steps that women can take to reduce their risk. These lifestyle changes and preventive measures can lower the likelihood of developing breast cancer:
- Limit Alcohol Consumption. Reducing or avoiding alcohol is one of the most effective steps in lowering the risk of breast cancer. Studies have shown that women who consume alcohol regularly have a higher risk, so limiting intake to moderate levels, or abstaining altogether, can help decrease this risk.
- Eat a Nutritious, Balanced Diet. A diet rich in fresh fruits and vegetables can support overall health and may reduce the risk of breast cancer. Opt for a variety of nutrient-dense foods, including whole grains, lean proteins, and healthy fats, while minimizing processed foods and red meat, which have been linked to higher cancer risks.
- Ensure Adequate Rest. Getting enough quality sleep is essential for maintaining a healthy immune system and hormonal balance. Poor sleep or chronic fatigue can affect hormone levels, which might influence breast cancer development. Aim for 7-9 hours of restful sleep each night.
- Manage Stress. Chronic stress can have a negative impact on the immune system and hormone levels. Finding healthy ways to manage stress, such as through meditation, yoga, or relaxation techniques, can contribute to better overall health and potentially reduce the risk of cancer.
- Exercise Regularly. Physical activity has been shown to lower the risk of breast cancer. Regular exercise helps regulate hormones, reduce body fat, and improve the immune system. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week, combined with strength training.
- Maintain a Healthy Weight. Keeping a healthy body weight is particularly important after menopause, as obesity is linked to a higher risk of breast cancer. Monitoring and maintaining a healthy Body Mass Index (BMI) through balanced eating and regular physical activity can reduce this risk.
- Consider Preventive Surgery. For women with a family history of breast cancer or who carry inherited genetic mutations (like BRCA1 or BRCA2), preventive surgery may be an option. Prophylactic mastectomy (preventive removal of breast tissue) or oophorectomy (removal of the ovaries) can significantly lower the risk of breast cancer. However, these options should be carefully discussed with a healthcare provider.
In addition to these lifestyle changes, regular screenings such as mammograms and clinical breast exams are critical for early detection. Women at high risk, due to genetic factors or family history, should consider speaking with their doctor about more intensive screening protocols or other preventive measures. While breast cancer cannot be completely prevented, these steps can help reduce the likelihood of developing the disease and improve overall health.
Risk Factors for Breast Cancer
Several risk factors increase the likelihood of developing breast cancer. Understanding these factors can help in identifying individuals who may be at higher risk and emphasize the importance of regular screenings and preventive measures. Here are the primary risk factors:
- Being Female. While men can develop breast cancer, the risk is significantly higher in women. This is largely due to hormonal differences, as breast tissue in women is more responsive to hormonal changes that can influence cancer growth.
- Age. As women age, the risk of breast cancer increases. The majority of breast cancer cases are diagnosed in women over the age of 50, particularly after menopause.
- Family History of Breast Cancer. A woman’s risk is higher if her mother, sister, or daughter has been diagnosed with breast cancer, especially if the diagnosis occurred before menopause. A strong family history suggests a possible genetic predisposition to the disease.
- Inherited Genetic Mutations. Mutations in certain genes, most notably BRCA1 and BRCA2, significantly increase the risk of breast cancer. These mutations can be passed down from parents to their children, raising the chances of developing breast cancer and other cancers, such as ovarian cancer.
- Personal History of Breast Conditions. Women diagnosed with lobular carcinoma in situ (LCIS) or atypical hyperplasia (an abnormal increase in cells) of the breast are at a higher risk of developing breast cancer. These conditions often serve as early warning signs of potential cancer development.
- Personal History of Breast Cancer. Women who have already had breast cancer in one breast are at a higher risk of developing cancer in the other breast or in another part of the same breast.
- Exposure to Radiation. Women who have undergone radiation therapy to the chest, particularly at a young age, are at greater risk of developing breast cancer later in life. This is particularly true for women treated for conditions like Hodgkin’s lymphoma.
- Obesity. Being overweight or obese, especially after menopause, increases the risk of breast cancer. Excess body fat can lead to higher estrogen levels, which fuel the growth of hormone-sensitive cancers like breast cancer.
- Early Menstruation. Women who began menstruating before the age of 12 have a slightly higher risk of breast cancer. Early menstruation results in longer exposure to estrogen and progesterone, which can increase cancer risk.
- Late Menopause. Women who experience menopause after the age of 55 are also at higher risk. Like early menstruation, late menopause increases the total exposure to estrogen over a woman’s lifetime.
- Late Pregnancy or No Pregnancy. Women who have their first child after the age of 30 or who have never been pregnant are at higher risk. Pregnancy reduces the total number of menstrual cycles a woman experiences in her lifetime, lowering her overall exposure to estrogen.
- Postmenopausal Hormone Therapy. Women who undergo hormone therapy that combines estrogen and progesterone for an extended period after menopause have an increased risk of breast cancer. This therapy is often used to manage menopausal symptoms but may elevate cancer risk, particularly with long-term use.
- Excessive Alcohol Consumption. Drinking alcohol in large quantities has been linked to an increased risk of breast cancer. The more alcohol a woman consumes, the higher her risk. Alcohol can affect estrogen levels, which may contribute to the development of breast cancer.
These risk factors do not guarantee that someone will develop breast cancer, but they do raise the likelihood. Awareness of these risks can encourage more regular screenings, such as mammograms, and prompt discussions with healthcare providers about personalized prevention strategies. Early detection remains one of the most critical factors in successfully treating breast cancer.
Breast Cancer FAQs
Here are some frequently asked questions about breast cancer, providing essential information for individuals seeking to learn more about the disease.
- What are the early signs of breast cancer?
Early signs of breast cancer may include a new lump or mass in the breast, changes in the size or shape of the breast, dimpling of the skin, nipple inversion (turning inward), and unusual nipple discharge. While not all lumps are cancerous, it’s important to have any new or unusual changes evaluated by a healthcare provider. - Who is at risk for breast cancer?
Breast cancer can affect anyone, but certain factors increase the risk. Women are at a higher risk than men, and the risk increases with age. Other risk factors include a family history of breast cancer, inherited gene mutations (such as BRCA1 or BRCA2), early menstruation, late menopause, obesity, and alcohol consumption. - Can men get breast cancer?
Yes, men can develop breast cancer, though it is much rarer than in women. Men should also be aware of changes in their breast tissue, such as lumps or swelling, and consult a doctor if they notice any unusual symptoms. - How is breast cancer diagnosed?
Breast cancer is diagnosed through several tests, including mammograms (X-rays of the breast), ultrasound, and MRI scans. If a suspicious lump or abnormality is detected, a biopsy is performed to confirm the presence of cancer cells. Hormone receptor and HER2 testing may also be done to help determine the most effective treatment. - Is breast cancer hereditary?
Yes, breast cancer can be hereditary. Inherited mutations in genes such as BRCA1 and BRCA2 increase the risk of developing breast cancer. Women with a strong family history of breast or ovarian cancer may choose to undergo genetic testing to assess their risk and discuss preventive measures with their doctor. - What are the treatment options for breast cancer?
Treatment for breast cancer depends on the type and stage of the disease. Common treatments include surgery (such as a lumpectomy or mastectomy), radiation therapy, chemotherapy, hormone therapy, and targeted therapy. The treatment plan is tailored to the individual based on the specific characteristics of the cancer. - Can breast cancer be cured?
Many cases of breast cancer can be cured, especially when detected early. The chances of a cure are highest when the cancer is confined to the breast and has not spread to other parts of the body. Even for advanced cases, treatments can often control the disease and prolong life. - How can I reduce my risk of breast cancer?
To reduce the risk of breast cancer, it is recommended to maintain a healthy weight, exercise regularly, limit alcohol consumption, avoid smoking, and eat a balanced diet rich in fruits and vegetables. Regular breast cancer screenings, such as mammograms, can also help detect cancer early when it is most treatable. - What should I do if I find a lump in my breast?
If you find a lump or notice any changes in your breast, it is important to consult a healthcare provider right away. While not all lumps are cancerous, a doctor can perform tests to determine the cause and recommend further steps if necessary. - At what age should I start getting screened for breast cancer?
Most women should start getting mammograms at age 40, though some healthcare providers may recommend starting earlier for women at higher risk. Women with a family history of breast cancer or other risk factors may need to begin screening at a younger age. Always consult with your doctor to determine the best screening schedule for you.
These FAQs offer a general understanding of breast cancer, but each individual’s situation is unique. For more personalized advice or concerns, it’s best to consult a healthcare provider who can guide you through screening, diagnosis, and treatment options.


