Summary
Bone cancer occurs when abnormal cells multiply uncontrollably within bone tissue. It can affect a specific part of the skeletal system or spread to other organs like the lungs or breasts. While its exact cause is unclear, genetic mutations are often involved, with both inherited and acquired mutations contributing to its development.
Key symptoms include swelling and pain around the affected bone, weakened bones prone to fractures, and general fatigue. Early detection is vital for effective treatment, which often involves surgery. In more advanced cases, radiotherapy or chemotherapy may be necessary to control the spread and minimize further damage.
Research on bone cancer continues, with modern treatments significantly improving outcomes. Early intervention, particularly surgery, greatly enhances the chances of recovery.
Table of Contents
Symptoms of Bone Cancer

Here are the common symptoms of bone cancer, enhanced and translated:
- Pain in the affected area. Pain is the most common symptom of bone cancer. Initially, the pain is triggered by movement, such as walking when the cancer is located in the thigh bone. As the cancer progresses, the pain may become persistent and worsen over time.
- Swelling may develop weeks after the onset of pain. This is caused by the growth of a tumor in the bone, leading to inflammation in the surrounding area.
- Bone fractures. Cancer weakens the bone structure, making the affected bone more prone to fractures, even with minor trauma or stress.
Other possible symptoms of bone cancer include:
- Unintended weight loss. Patients may experience a rapid and unexplainable loss of weight as the cancer progresses.
- Fatigue. The patient may feel constantly tired, even with adequate rest.
- Arthritis-like symptoms. Joint stiffness or pain can occur, often confused with arthritis.
- Breathing difficulties. This may happen if the cancer has spread to the lungs, causing additional complications.
The symptoms can vary depending on the location and stage of the cancer, and they often overlap with other less severe conditions. Early detection is crucial for better treatment outcomes.
Types of Bone Cancer
There are various types of bone cancer, classified based on the specific cells where the cancer first forms. The most common types of bone cancer include the following:
- Osteosarcoma. This is the most common type of bone cancer, usually affecting children, adolescents, and young adults. In this condition, the cancerous cells are those that form new bone tissue. Osteosarcoma typically starts in the long bones, such as the thigh bone (femur) and upper arm (humerus).
- Chondrosarcoma. The second most common type of bone cancer, chondrosarcoma primarily affects middle-aged adults. It typically develops in the cartilage, which is the flexible tissue that pads the joints. This cancer often starts in the pelvis, legs, or arms.
- Ewing Sarcoma. Ewing sarcoma is more common among children and young adults, often starting in the long bones like the thigh (femur), pelvis, or even the chest wall. It is a fast-growing cancer that can also spread to other parts of the body.
- Chondrosarcoma. Although there was a mention earlier, chondrosarcoma indeed primarily develops in the cartilage. It usually affects individuals in their 40s and older. This type of cancer tends to grow slowly but can invade the surrounding bone structures over time.
- Chordoma. This is a rare type of bone cancer that typically affects the spine and the base of the skull in older adults. However, it can also affect children. This type grows slowly but can be quite invasive when it spreads to nearby tissues.
While bone cancer is rare, its impact can be significant, particularly if it is not detected early. Understanding the types of bone cancer helps in choosing the appropriate treatment plans and understanding the disease’s progression.
Diagnostic Procedures for Bone Cancer
Detecting and diagnosing bone cancer requires a combination of medical imaging, laboratory tests, and biopsies to assess the presence and extent of the disease. Early diagnosis is critical for improving the chances of successful treatment. Here are the primary diagnostic procedures used to identify bone cancer:
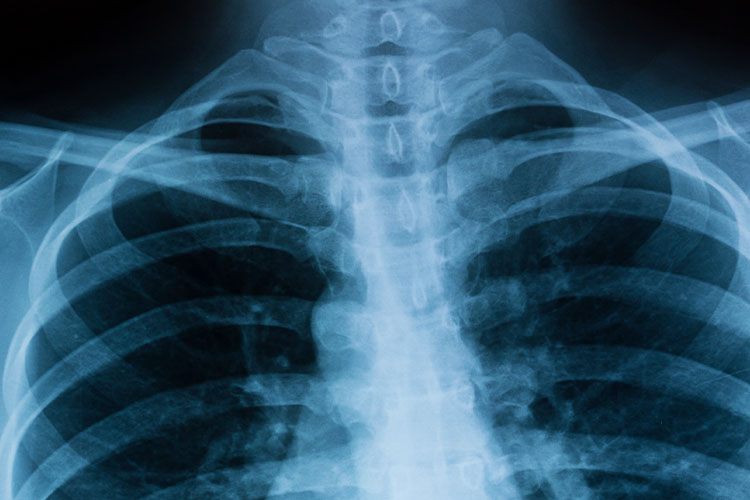
- X-rays. X-rays are often the first imaging test conducted when bone cancer is suspected. They provide detailed images of the bone, revealing any abnormal growths or tumors. In cases of bone cancer, X-rays can show irregularities like bone destruction or the formation of new, disorganized bone tissue.
- Magnetic Resonance Imaging (MRI). MRI scans use powerful magnets and radio waves to create detailed cross-sectional images of the body. They provide a clearer view of the tumor’s size, location, and whether it has spread to surrounding soft tissues. MRIs are particularly useful in determining the precise extent of the cancer before planning surgery.
- Computed Tomography (CT) Scan. A CT scan provides a more detailed, three-dimensional view of the affected bone and surrounding tissues than a traditional X-ray. It is often used to check if the cancer has spread (metastasized) to other organs, such as the lungs.
- Bone Scan. A bone scan involves injecting a small amount of radioactive material into a vein, which is absorbed by the bones. A special camera detects the radiation, highlighting areas of abnormal bone activity, which may indicate cancer or other bone conditions. This test is particularly useful for detecting the spread of cancer to other bones.
- Positron Emission Tomography (PET) Scan. A PET scan uses a small amount of radioactive sugar to detect active cancer cells in the body. Since cancer cells typically absorb sugar more rapidly than normal cells, this test helps in identifying metastasis or checking the effectiveness of ongoing treatments.
- Biopsy. A biopsy is the definitive test for diagnosing bone cancer. During this procedure, a sample of the abnormal tissue is taken from the suspected tumor and examined under a microscope to determine if cancer cells are present. There are two main types of biopsy procedures for bone cancer:
- Needle Biopsy. A thin, hollow needle is inserted into the tumor to extract a small sample of tissue.
- Surgical Biopsy. A small incision is made to remove a larger portion of the tumor or, in some cases, the entire tumor for analysis.
- Blood Tests. Although blood tests cannot diagnose bone cancer directly, they can help determine overall health and identify certain markers associated with cancer. For example, elevated levels of alkaline phosphatase or lactate dehydrogenase (LDH) may indicate bone disease, although these markers are not specific to bone cancer.
Complications of Untreated Bone Cancer

If bone cancer remains untreated, it can lead to several serious and potentially life-threatening complications. These complications can affect the skeletal system, surrounding tissues, and even other organs. Here are some of the key complications associated with untreated bone cancer:
- Bone Fractures and Structural Weakness. One of the most common complications of bone cancer is a weakened bone structure. As cancer cells grow, they destroy healthy bone tissue, which increases the risk of fractures, even from minor injuries or everyday activities. These fractures are often called “pathologic fractures” because they result from weakened bone rather than external trauma.
- Tumor Growth and Expansion. Without treatment, the cancerous tumor can grow larger, putting pressure on nearby muscles, nerves, and blood vessels. This can lead to chronic pain, numbness, or a loss of function in the affected limb. As the tumor grows, it may also lead to swelling, making movement and daily activities more difficult.
- Metastasis. Untreated bone cancer can spread to other parts of the body, a process known as metastasis. The lungs are a common site for metastasis from bone cancer, particularly for osteosarcoma. Once the cancer spreads to vital organs like the lungs, it becomes much harder to treat and significantly reduces the patient’s chances of survival.
- Hypercalcemia. Bone cancer can cause excessive calcium to be released into the bloodstream due to bone destruction. This condition, known as hypercalcemia, can cause symptoms such as nausea, vomiting, confusion, and kidney problems. If left untreated, hypercalcemia can be life-threatening.
- Severe Pain. As the cancer progresses, it can lead to significant, persistent pain. Bone cancer pain is often severe because the tumor destroys bone tissue and may also compress surrounding nerves. Over time, this pain can become debilitating, affecting the patient’s quality of life and ability to perform daily tasks.
- Mobility Impairment. The progression of bone cancer can lead to a significant loss of mobility, particularly if the tumor is located in the limbs. This can make walking or using the affected limb very difficult, reducing independence and increasing reliance on mobility aids.
- Organ Dysfunction. In cases where bone cancer spreads to other organs like the lungs or liver, it can severely impact their function. This can lead to respiratory difficulties, liver failure, or other life-threatening conditions that can be challenging to manage without timely treatment.
- Increased Risk of Infection. Bone cancer, especially when untreated, weakens the body’s immune system, making patients more susceptible to infections. In addition, if a fracture occurs or if surgery is needed, the risk of infection in the affected area increases, which can further complicate the patient’s condition.
Early detection and prompt treatment are crucial to prevent these severe complications. If bone cancer is left untreated, not only does the disease progress, but it also significantly lowers the chances of successful treatment and recovery.
Causes of Bone Cancer
The true cause of bone cancer remains uncertain, but studies suggest that genetic mutations play a significant role in its development. These mutations are not inherited but occur when a person is exposed to chemicals or other substances that may trigger the onset of cancer in the bone. Research continues to better understand how these mutations happen and what other factors might contribute to the disease.
Treatment for Bone Cancer
The treatments for bone cancer depend on the type, stage, and health of the patient. Here are the most common treatment methods:
- Surgery. Surgery is often the first line of treatment. It aims to remove the cancerous tumor while trying to preserve the bone and surrounding tissues. Limb-sparing surgeries are common, but in some cases, amputation may be required. Reconstruction using prosthetics or bone grafts may follow surgery to restore function.
- Chemotherapy. Chemotherapy involves using powerful drugs to kill cancer cells or prevent them from growing. It is often used for aggressive bone cancers like osteosarcoma and Ewing sarcoma, especially if the cancer has spread. Sometimes it’s administered before surgery to shrink tumors or after surgery to destroy remaining cancer cells.
- Radiation Therapy. This treatment uses high-energy radiation to target and kill cancer cells. It is commonly used for cancers like Ewing sarcoma that respond well to radiation. Radiation therapy can also help shrink tumors before surgery or relieve pain in advanced cancer cases.
- Targeted Therapy. This approach targets specific molecules involved in cancer growth. Targeted therapies are often used in cases where other treatments are less effective, offering a more precise attack on cancer cells while minimizing damage to healthy cells.
- Immunotherapy. Immunotherapy helps boost the body’s immune system to attack cancer cells more effectively. Though not common in bone cancer treatment, it is being studied for its potential in advanced cases.
- Cryosurgery. This method involves freezing and destroying cancer cells using liquid nitrogen. It is an option for certain bone cancers when conventional surgery is not feasible.
- Palliative Care. For advanced bone cancer, palliative care focuses on relieving symptoms and improving quality of life. This may involve managing pain, using radiation therapy to shrink tumors, or providing supportive therapies to maintain mobility and strength.
Treatment is usually a combination of these methods to enhance the chances of success and improve patient outcomes.
Prevention of Bone Cancer
Preventing bone cancer is challenging because its exact cause is still unknown, and many of the risk factors are unavoidable, such as genetic mutations or conditions present from birth. However, there are steps that may help reduce the risk or at least help in the early detection of bone cancer:
- Avoid exposure to harmful chemicals. Prolonged exposure to certain chemicals, such as industrial toxins and carcinogens, may increase the risk of cancer. Minimize exposure to harmful substances, especially in the workplace.
- Radiation safety. Avoid unnecessary exposure to radiation, especially in medical settings. If radiation therapy is required for another condition, ensure that it is done with the appropriate safety measures.
- Healthy lifestyle. Eating a balanced diet rich in vitamins and minerals can help keep bones strong and healthy. Regular exercise and avoiding smoking or excessive alcohol intake also support overall health, reducing the risk of cancer and other diseases.
- Genetic screening. Individuals with a family history of genetic conditions like Li-Fraumeni syndrome or hereditary retinoblastoma, which increase the risk of bone cancer, may benefit from genetic testing. This allows for early monitoring and preventive steps.
- Avoid smoking and alcohol abuse. Smoking and heavy alcohol consumption weaken the immune system, increasing cancer risk. Quitting smoking and moderating alcohol intake can improve overall health and reduce the likelihood of developing cancers, including bone cancer.
- Manage pre-existing bone conditions. Conditions like Paget’s disease or inherited bone disorders raise the risk of bone cancer. Proper treatment and regular check-ups help manage these conditions and allow for early detection if cancer develops.
- Exercise and bone health. Regular physical activity, particularly weight-bearing exercises, strengthens bones and promotes overall health, which may indirectly reduce the risk of bone cancer.
While prevention is not always possible, adopting these measures can help reduce the risks associated with bone cancer. Early detection and a healthy lifestyle are key factors in mitigating potential health risks.
Risk Factors for Bone Cancer

Bone cancer is a rare but serious condition where abnormal cells form in the bones, leading to the development of tumors. It can affect any bone in the body, though it commonly arises in the long bones of the arms and legs. There are multiple types of bone cancer, each with distinct characteristics and affecting different age groups. While the exact cause remains unclear, genetic mutations and previous radiation exposure are significant factors. Early detection and treatment, such as surgery or chemotherapy, greatly improve the prognosis, especially when diagnosed at an early stage.
- Inherited conditions. Some inherited genetic disorders may increase the risk of bone cancer. Though the exact mechanism isn’t fully understood, doctors are researching how specific genetic mutations could play a role in its development.
- Paget disease. People with Paget disease, a condition that causes abnormal bone growth, have a higher likelihood of developing bone cancer. Although the tumors in Paget disease are typically non-cancerous, they can evolve into malignant tumors over time. It’s crucial for individuals with Paget disease to be monitored regularly to prevent the progression to cancer.
- Exposure to radiation. Bones that are exposed to high levels of ionizing radiation, especially during cancer treatments, have an increased risk of developing bone cancer. While normal diagnostic X-rays are considered safe, prolonged or high-level exposure to radiation can pose a risk, especially in younger and older individuals.
- Previous bone marrow transplants. There is a slight increased risk of developing bone cancer in people who have undergone bone marrow transplants, typically used to treat blood cancers or severe blood conditions. This risk stems from the extensive treatments involved in bone marrow transplantation, such as chemotherapy and radiation, which may contribute to cancerous changes in bone tissue later on.
These risk factors don’t guarantee that a person will develop bone cancer but highlight groups of individuals who may be more vulnerable and who should monitor their bone health more closely. Regular check-ups and early detection can make a significant difference in managing or preventing this condition.
Bone Cancer FAQs
- What is bone cancer?
Bone cancer is a rare type of cancer that starts in the bones. It involves the abnormal and uncontrollable growth of cancerous cells in bone tissues, leading to tumors that may spread to other parts of the body. There are several types of bone cancer, including osteosarcoma, chondrosarcoma, and Ewing sarcoma. - What are the common symptoms of bone cancer?
The most common symptoms include persistent bone pain, swelling near the affected area, fractures in weakened bones, fatigue, and unintended weight loss. In more severe cases, bone cancer can cause difficulty in movement and breathing problems if it spreads to the lungs. - What causes bone cancer?
The exact cause of bone cancer is still not fully understood. However, genetic mutations, exposure to high doses of radiation, and certain inherited conditions, such as Paget disease and Li-Fraumeni syndrome, are believed to increase the risk of developing this cancer. - Who is at risk for bone cancer?
Individuals who have undergone radiation therapy, have a family history of bone cancer, or have genetic disorders like hereditary retinoblastoma are at a higher risk. Bone cancer is more common in teenagers and young adults, though it can occur at any age. - How is bone cancer diagnosed?
Bone cancer diagnosis often involves imaging tests such as X-rays, CT scans, MRIs, and bone scans to detect tumors. A biopsy, where a sample of the bone tissue is taken for lab analysis, is the definitive method to confirm the presence of cancer. - Can bone cancer spread to other parts of the body?
Yes, bone cancer can metastasize (spread) to other parts of the body. The most common site for metastasis is the lungs, but it can also spread to other bones and organs. Early detection and treatment are crucial to prevent the spread of cancer cells. - What are the treatment options for bone cancer?
The primary treatments for bone cancer include surgery to remove the tumor, chemotherapy to destroy cancer cells, and radiation therapy to shrink tumors. The type of treatment depends on the stage and type of bone cancer, as well as the patient’s overall health. - Can bone cancer be cured?
Bone cancer can be curable, especially when detected early. Success rates vary depending on the type of cancer, its stage at diagnosis, and how well the patient responds to treatment. Osteosarcoma and Ewing sarcoma in younger patients often have better outcomes when treated early. - How can I reduce the risk of developing bone cancer?
Though bone cancer cannot always be prevented, you can lower your risk by minimizing exposure to radiation, avoiding tobacco, and leading a healthy lifestyle. Regular medical check-ups, especially if you have risk factors, are essential for early detection. - Is bone cancer hereditary?
While bone cancer itself is not always hereditary, certain genetic conditions, such as hereditary retinoblastoma or Li-Fraumeni syndrome, can increase the likelihood of developing bone cancer. If you have a family history of these conditions, it is advisable to discuss your risks with a healthcare provider.


